Cheek Rotation Skin (Mustardé) Flap to The Lower Eyelid
J. C. MUSTARDÉ
Reconstruction of the full thickness of an eyelid requires two basic layers: a skin-covering layer and a mucous-secreting layer. One of these layers can be a free graft, but at least one must be in the form of a flap with a continuous blood supply.
INDICATIONS
Eyelid tissues, including the tarsal plate and margin, will stretch to some degree, and a defect of about a quarter of the lower lid width can be closed directly. Closure of a defect only a few millimeters greater than a quarter of the lower lid width can usually be obtained by dividing the lower crus of the lateral canthal ligament. Where this does not allow sufficient relaxation to permit closure, a cheek rotation flap can then be used.
In defects involving from one-quarter to one-half of the eyelid, a comparatively small cheek rotation is required. Because of the stretch of tissues just alluded to, the dimension of the actual full-thickness lid reconstruction that must be carried out will be only about a quarter of the original width of the lid, i.e., about 6 to 7 mm. It is probable that adequate lining for the reconstructed segment will be available from the tissues of the lower fornix (Fig. 13.1).
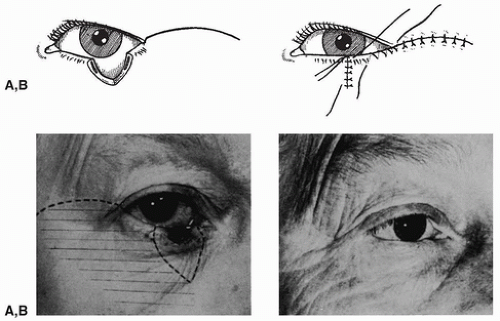 FIGURE 13.1 Reconstruction of a quarter to a half of the lower lid. A small rotation of the cheek is sufficient to provide skin cover, while lining can often be obtained from the conjunctiva in the lower fornix. (From Mustardé, ref. 1, with permission.) |
This does not provide a very defined, stable margin, but such a small sector of the lid is involved, lying in an area where the cornea is unlikely to be affected, that the instability of the reconstructed margin may be of little importance. If adequate conjunctiva is not available, however, or if the reconstructed area is wider than about 6 mm, it is best to line the reconstructed part of the lid with a small composite nasal septal graft.
Where a defect greater than half the eyelid exists and the width of the reconstructed lid part is greater than one-quarter of the lid width, a much larger cheek rotation skin flap must be used. This presents no great problem in itself, but the instability of the weak reconstructed margin, both with respect to the possibility of it turning outward (which will produce epiphora) or turning in (where the squamous epithelium may come to rub on the cornea), as well as the lack of permanent support to the reconstructed lid segment, must be taken into account.
A mucus-secreting lining for the skin flap can be provided by using a graft of any mucosal surface. However, there will be no orbicularis muscle in the reconstructed lid segment, and because of the constant lifting action of the orbicularis muscle, skin flaps, mucosal grafts, and even tarsal plate from another
eyelid will slowly stretch under the influence of gravity and time (witness the end result in seventh nerve palsy affecting a completely normal lower eyelid). It is therefore necessary in a reconstruction of any extent in a lower eyelid to provide not only a mucus-secreting lining, but also some supportive material that will permit the fashioning of a permanently stable margin and that also will give constant positive support to the reconstructed segment of the lid (1).
eyelid will slowly stretch under the influence of gravity and time (witness the end result in seventh nerve palsy affecting a completely normal lower eyelid). It is therefore necessary in a reconstruction of any extent in a lower eyelid to provide not only a mucus-secreting lining, but also some supportive material that will permit the fashioning of a permanently stable margin and that also will give constant positive support to the reconstructed segment of the lid (1).
FLAP DESIGN AND DIMENSIONS
I believe that the best foundation for lower eyelid reconstruction is to use a flap for the skin layer. Skin for this purpose may be obtained from almost any region around the orbit, but one of the simplest and most logical techniques is to use a cheek rotation flap to carry the thin skin that lies lateral to the lateral canthus into the region of the reconstructed eyelid. The incision line of the flap should curve upward and outward from the lateral canthus. The length of the cheek incision, as well as the amount of undermining to be carried out, is determined on a trial-and-error basis by constantly checking whether the flap can be rotated across to fill the defect. Rotation of the cheek flap is facilitated by resecting a skin triangle below the eyelid defect (Fig. 13.1C).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








