CHAPTER 5 PYOGENIC GRANULOMA
KEY POINTS
Most pyogenic granulomas require treatment, because they are at risk for bleeding.
A barrier dressing (for example, a Band-Aid) is used to cover the lesion to avoid incidental trauma and hemorrhage.
Interventions that do not treat the entire depth of the dermis have a higher recurrence rate.
Full-thickness skin excision is used for large lesions.
Small pyogenic granulomas or those with a narrow base can be treated with needle-tip cautery through the dermis.
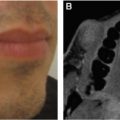
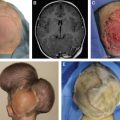
A pyogenic granuloma (PG) is also referred to as a lobular capillary hemangioma. It is unique in the field of vascular anomalies, because almost all PGs are treated surgically. Many other types of vascular anomalies are managed by observation, pharmacotherapy (topical, intralesional, or systemic), laser, sclerotherapy, and/or embolization. A PG is red and may be sessile or pedunculated. Lesions average 6 mm in diameter, and the mean age of onset is 6 years. PGs most commonly affect the head/neck (two thirds), followed by the trunk, upper extremity, and lower extremity. The integument or mucous membranes are involved. Numerous treatments have been described: curettage, cryotherapy, full-thickness skin excision, laser, shave excision, and superficial cautery; pharmacotherapy is not effective. Because PGs involve the reticular dermis, interventions that do not treat the entire depth of the skin have an approximately 50% recurrence rate (for example, curettage, shave excision, superficial cautery, and laser therapy).
SURGICAL INDICATIONS
Surgical management of a PG is usually mandatory. Unlike many other types of vascular anomalies that are often removed to improve the patient’s appearance, PGs have a significant risk of ulceration and bleeding. Consequently, asymptomatic lesions are extirpated to obviate the risk of hemorrhage. A secondary indication to remove a PG is to improve the patient’s self-esteem, which can be lowered if the tumor is located in a visible area.
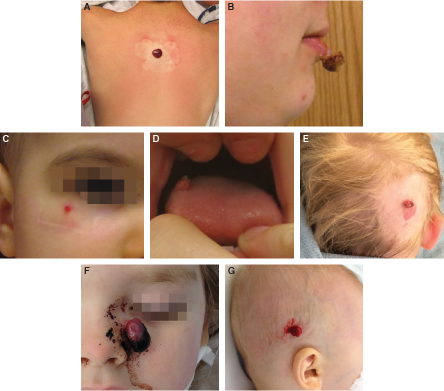
The phenotypes and morbidity of PGs are demonstrated. A large sessile lesion of the posterior trunk is seen (A). A pedunculated PG of the lip causing psychosocial morbidity is shown (B). A small lesion of the cheek is seen (C). An intraoral PG is visible (D). A PG that developed in a capillary malformation is seen (E). An ulcerated lesion (F) and a bleeding PG (G) are shown.
SURGICAL MANAGEMENT
TIMING OF INTERVENTION
A PG requires intervention, regardless of the age of the patient. Most individuals present after the lesion has bled; many have been managed in an emergency department for hemorrhage before their referral. Although the amount of blood loss is not harmful to the patient, bleeding can cause significant anxiety for the individual and family. Consequently, the procedure is scheduled as soon as possible. Lesions that have not yet bled can be scheduled less acutely. Rarely a small and flat PG may exist for a long period without a history of hemorrhage. Consideration is given to treating the lesion before 4 years of age, when the patient’s long-term memory and self-esteem begin to form. In older children, adolescents, and adults, the onset of a PG can cause psychosocial morbidity, and the patient will seek intervention to improve his or her appearance (see Video 5-1, Pyogenic Granuloma).
While awaiting treatment, a PG will occasionally “fall off” as a result of incidental trauma, ulceration, or bleeding. The lesion usually reenlarges, because the component in the deep dermis remains. If the PG has “disappeared,” I examine the patient, and if a cutaneous component is present, I will offer treatment to eliminate the risk of regrowth (if the lesion enlarges and begins to bleed again, the morbidity and scar will be worse). If I am unable to identify the PG after it has fallen off, the patient is observed.
CONTROL OF THE LESION UNTIL SURGICAL TREATMENT
A PG typically hemorrhages from incidental trauma and does not bleed spontaneously. Patients and families are counseled to cover the lesion with a Band-Aid for protection until it is treated. If a PG bleeds, families are instructed to cover the lesion with a Band-Aid and then apply pressure with a washcloth soaked in ice water over the Band-Aid. If a washcloth is touching the PG, the lesion will rebleed after pressure is discontinued, because the lesion/clot will be adherent to the washcloth.
TYPE OF ANESTHESIA
Determining whether a PG can be treated with local or general anesthesia depends on the age of the patient, the location of the lesion, and the size of the PG. A young child with a large lesion on the face is more likely to require general anesthesia than an older individual with a small PG on the trunk. Generally, removal of facial lesions cannot be performed with the patient under local anesthesia before adolescence. PGs located on the trunk or extremity may be able to be excised in the office in older children. If I am comfortable removing a lesion with either a local or general anesthetic, I will let the patient/family chose which method they prefer.
FULL-THICKNESS SKIN EXCISION
My first-line treatment for PGs is excision of the skin involving the lesion, because it eliminates the risk of recurrence. An additional advantage of resection is that the specimen can be sent for histopathologic examination. The borders of the PG are marked, and the surgical site is infiltrated with 0.25% bupivacaine with epinephrine. I prefer a long-acting local anesthetic to give the patient a greater duration of pain control. Epinephrine can be administered anywhere in the body (including fingers and toes); it facilitates the procedure by reducing blood loss. If the PG is sessile, the excision borders are at the junction of the lesion and normal surrounding tissue. A margin of normal skin should not be harvested, because the PG is benign and the length of the scar will increase. Most PGs have a small base attached to the skin with a larger, superficial component (similar to a mushroom). It is important to lift the PG and outline only the base for excision. Usually a much smaller incision and scar are necessary than was initially expected. Lesions can be removed with a No. 67 Beaver blade or a No. 11 blade. After resection to the subcutis, the base of the wound is cauterized to injure any possible remaining lesional tissue to reduce the risk of recurrence.
After excision of a PG, the wound can be closed in three ways:
Linearly
As a circle
Allowed to heal secondarily
Linear closure is used for lesions located on the trunk or extremity or head/neck in a nonconspicuous location (for example, the scalp) or for noncircular lesions. In children I place absorbable sutures to avoid removal, which can be traumatic for the patient and parents. PGs that are circular and located in unfavorable locations on the face (for example, the nose, lip, or cheek) are best managed by circular excision and purse-string closure. Although a circular excision limits the length of the scar, a disadvantage is that a second procedure may be necessary to convert the round scar into a line. If a second stage is performed, the length of the scar will be approximately the same size as the diameter of the original lesion. More than one half of patients are satisfied with the appearance of the circular scar and are not interested in a second stage to convert it into a line. The circular scar can appear similar to a chicken pock or acne scar. Occasionally I allow small circular PGs located in unfavorable locations (for example, the mucocutaneous junction of the lip and nasal tip) to heal secondarily. Placing sutures into very small openings can be difficult and lengthen the scar; allowing a circular area to contract also minimizes distortion of surrounding structures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree