CHAPTER 13 ORAL CAVITY AND AIRWAY
KEY POINTS
Airway management is of paramount concern in patients with vascular malformations of the head and neck.
Complete resection of head and neck malformations is rarely possible and recurrence is common.
Functional considerations and the potential for large-volume blood loss may dictate surgical timing and planning.
Endoscopic and/or laser techniques may be necessary for upper airway lesions.
Radiofrequency ablation is a promising technique, which is most useful for superficial, microcystic lesions of the tongue and oral cavity.
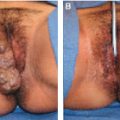
Cervicofacial vascular malformations can cause both short-term and long-term morbidity, including airway obstruction, feeding difficulty, bleeding, dysarthria, bony remodeling, and altered appearance. Although macrocystic lymphatic malformations typically occur below the level of the mylohyoid muscle and are amenable to excision or sclerotherapy, most lesions of the oral cavity have a microcystic component. The submucosal, infiltrative pattern of spread of these lesions often results in extension to adjacent subsites and deep neck spaces. The functional consequences of complete surgical resection may be unacceptably morbid because of the proximity of important neural, vascular, and muscular structures. Lesions affecting the airway can cause airway obstruction and become life-threatening. Subtotal excision can improve symptoms but is associated with a high rate of recurrence. For these reasons, extensive lesions of the tongue, oral cavity, and airway are particularly difficult to treat.
SURGICAL INDICATIONS
AIRWAY COMPROMISE
The airway is the primary concern in an infant with a vascular malformation involving the head and neck. Signs and symptoms usually correlate with the extent of the lesion. Extrinsic compression on the airway by the vascular anomaly or intrinsic involvement of the hypopharynx or larynx can occur. Narrowing of the airway demands prompt recognition and treatment, because a marginal airway can rapidly obstruct from small changes resulting from viral infection or intralesional bleeding.
A prenatal diagnosis of vascular malformations by ultrasonography and/or MRI is becoming increasingly common. If prenatal imaging identifies the potential for airway compromise, ex utero intrapartum treatment (EXIT) with intubation or tracheostomy should be planned.
INITIAL EVALUATION
Patients with vascular malformations of the oral cavity and upper airway will often present with recurrent infections, swelling, and tenderness. In addition, involvement of the tongue may cause dysphagia, dysarthria, or airway obstruction. Mucosal lymphatic vesicles may cause bleeding, tenderness, and oozing, which may often worsen during upper respiratory tract infections or after trauma.
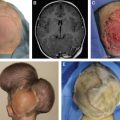
All patients presenting with a vascular malformation of the head and neck with possible airway involvement should undergo flexible fiberoptic nasopharyngolaryngoscopy to evaluate the involvement of the hypopharynx, supraglottis, and glottis. Examination findings should be integrated with radiologic evaluation to determine the complete extent of the lesion and its proximity to vital structures. In lymphatic malformations, ultrasonography will typically demonstrate multilocular cystic tissue without flow except in the septal areas; a CT scan reveals a low-attenuated lesion with enhancement of the channel walls after injection of contrast. An MRI with gadolinium is the single best radiologic technique for characterizing lymphatic malformations and typically shows cystic spaces and rim enhancement on T1-weighted images.
SURGICAL MANAGEMENT
Treatment goals for vascular malformations of the head and neck include providing a safe airway, reducing symptoms, correcting functional problems, and improving appearance. Because complete resection is rarely possible, treatment focuses on reducing symptoms while causing as little damage as possible to adjacent tissue.
Options for treatment include expectant management, surgical excision, sclerotherapy, and radiofrequency ablation (RFA).
CONSERVATIVE MANAGEMENT
Spontaneous regression of vascular malformations is rare, but invasive treatment can be avoided in a small subset of patients with no complaints, minor symptoms, or intermittent symptomatic periods effectively controlled with medical management. Medical therapy may include systemic antibiotics to treat infection and oral care with frequent rinses and dental treatment.
SURGICAL EXCISION
Resection is the only way to potentially “cure” a vascular malformation. The surgeon must consider possible involvement of neural and vascular structures. Limiting blood loss and preservation of vital structures are of paramount importance in these cases.
Open Resection
A number of issues should be considered when planning surgical resection of a vascular malformation. First, the timing of surgery is important, as is the mode of dissection, whether by sharp dissection, electrocautery, or laser. Second, it is important to consider whether it is best to attempt complete resection in a single procedure or whether staged resection is indicated. Dividing vascular malformations into subtypes is also often useful for surgical planning. Those lesions located below the level of the mylohyoid muscle in general may be safely resected within the first year of life. In this case sharp dissection is frequently the modality of choice, and they can often be resected during one procedure. Malformations above the level of the mylohyoid muscle are frequently poorly defined, and the planes between the malformation itself and the normal anatomy may be difficult to dissect. Complete surgical resection in these circumstances can be quite a challenge. The use of loupes or operating microscope is helpful, and a nerve stimulator is imperative, because normal anatomy is frequently disrupted. We recommend that surgery be performed before 5 years of age if possible. Factors such as expected blood loss, duration of the procedure, and extent of dissection may help to determine whether multiple procedures are needed.
Lingual excision should be avoided except in rare cases of solitary lesions of the anterior tongue. Transoral resection of the tongue base or floor of the mouth should be avoided because of the high likelihood of postoperative dysphagia and/or aspiration. We have found that RFA is a safe and effective treatment modality for many patients with lymphatic malformations of the oral cavity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree