CHAPTER 1 TERMINOLOGY AND CLASSIFICATION
KEY POINTS
Correct biologic terminology should be used to describe vascular anomalies.
Vascular anomalies are divided into tumors and malformations.
Four types of tumors and four types of malformations constitute approximately 95% of lesions.
Approximately 90% of vascular anomalies can be diagnosed by assessing the patient’s history and the physical examination.
Vascular anomalies are common, affecting approximately 5% of the population. Lesions affect all components of the vasculature (for example, capillaries, arteries, veins, and lymphatics) and can occur in any anatomic area. Because the integument is the most commonly involved organ, patients most frequently present to a plastic surgeon or dermatologist. Although some lesions (for example, infantile hemangioma, pyogenic granuloma, and capillary malformation) can be managed by a single physician who is focused on this field, many types of lesions (for example, venous malformation, lymphatic malformation, and arteriovenous malformation) require interdisciplinary care. Patients with vascular anomalies pervade most medical and surgical specialties. Academic medical centers often have vascular anomalies centers where patients with complex lesions can be managed.
Historically, the field has been handicapped because the diagnosis and treatment of vascular anomalies are difficult. Physicians are often intimidated by the subject matter, because lesions have a similar appearance, and the terminology used to describe vascular anomalies has been imprecise. The topic is further complicated because the type of intervention is commonly based on the preference of the treating physician.
Before the surgeon determines the management of a patient with a vascular anomaly, the lesion must be accurately diagnosed with the correct current terminology. Surgical management of an individual with a vascular anomaly is not considered, unless the surgeon understands the pathophysiology of the lesion and available treatment options. This chapter serves as a framework for the role of surgical treatment of vascular anomalies.
TERMINOLOGY
Previously, vascular anomalies were labeled according to the type of food they resembled (for example, cherry, strawberry, and port-wine). Capillary or strawberry hemangiomas became associated with a red infantile hemangioma that involved the skin. If an infantile hemangioma was located below the integument and appeared bluish, it was often called a cavernous hemangioma. The terms capillary and cavernous were also used to describe capillary malformation and venous malformation, respectively. Another label for capillary malformation was port-wine stain. Cystic hygroma and lymphangioma became terms for macrocystic lymphatic malformation and microcystic lymphatic malformation, respectively. Hemangioma continues to be used to describe any type of vascular anomaly.
In 1982 Mulliken and Glowacki clarified the field of vascular anomalies by creating a biologic classification of these lesions. They reserved the suffix -oma (increased cell division) for vascular tumors. Terms such as lymphangioma, cystic hygroma, and cavernous hemangioma, which describe nonproliferating malformations, were no longer used. In 1996 the International Society for the Study of Vascular Anomalies (ISSVA) adopted the biologic classification of vascular anomalies.
Although significant progress has been made, incorrect terminology continues to pervade the medical community. Approximately 50% of patients evaluated at our center have an erroneous referral diagnosis; malformations are more likely to be misdiagnosed than tumors. Our review of the 2009 literature revealed that 71% used the term hemangioma incorrectly to describe another vascular anomaly. Patients whose lesions were mislabeled as a hemangioma had a 20% chance of being managed incorrectly.
CLASSIFICATION
The biologic classification of vascular anomalies has been revised based on the evolving understanding of the field (most recently in 2015). Vascular anomalies are classified based on their clinical behavior and cellular characteristics. Applying this framework, at least 90% of lesions can be diagnosed by history and physical examination. There are two broad types of vascular anomalies: tumors and malformations.
Tumors demonstrate endothelial proliferation and affect approximately 5% of the population. There are four major types:
Infantile hemangioma
Congenital hemangioma
Kaposiform hemangioendothelioma
Pyogenic granuloma
Vascular malformations are errors in vascular development and have minimal endothelial turnover. They affect approximately 0.5% of the population. There are four major categories based on the primary vessel that is malformed:
Capillary malformation
Lymphatic malformation
Venous malformation
Arteriovenous malformation
Malformations can be further divided into rheologically slow-flow lesions (for example, capillary, lymphatic, or venous) and fast-flow lesions (for example, arteriovenous malformations).

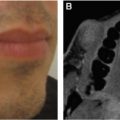
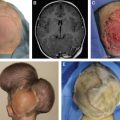
There are many phenotypic subtypes of the major categories of vascular anomalies (for example, glomuvenous malformation), combined lesions (for example, capillary-lymphatic-venous malformation), and eponymous syndromes (for example, Parkes Weber). The expanded classification of vascular anomalies can be overwhelming for a clinician not focused on these lesions. To simplify the field, if a physician focuses on the eight major types of lesions, he or she should be able to manage approximately 95% of patients with a vascular anomaly. The eight major types of vascular anomalies are shown: A, Infantile hemangioma; B, congenital hemangioma; C, kaposiform hemangioendothelioma; D, pyogenic granuloma; E, capillary malformation; F, venous malformation; G, lymphatic malformation; and H, arteriovenous malformation.
The classification of vascular anomalies continues to expand and become more precise as our knowledge increases. Recently the causative somatic mutation for many types of lesions has been identified. In the future the delineation of these lesions will shift from a clinical-histopathologic perspective to a molecular framework. Despite the widening classification of vascular anomalies, about 1% of patients referred to our center have a lesion that we are unable to diagnose.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree