55. Breast Reduction
Joshua Lemmon, Michael R. Lee, Daniel O. Beck, Elizabeth Hall-Findlay
PATHOPHYSIOLOGY
■ Breast hypertrophy is thought to be an abnormal end-organ response to circulating estrogens.1,2
■ Normal number of estrogen receptors and normal levels of circulating estrogens have been found in women with hypermastia; thus an increased sensitivity to the hormone is suspected.3
■ Hypermastia typically begins within the hormonal milieu of puberty or pregnancy.
■ With the increasing obesity epidemic, breast hypertrophy is often from excess adipose tissue rather than glandular hyperplasia.
■ Studies suggest that fat accounts for 46%-61% of modern breast reduction specimens.4,5
INDICATIONS FOR SURGERY
Breast reduction has an extremely high patient satisfaction rate and has been shown to improve self-image.6,7
MEDICAL INDICATIONS
■ Neck pain
■ Back pain
■ Shoulder pain
■ Bra strap grooving
■ Persistent or recurrent intertriginous infections, rashes, maceration, and irritation
■ Chronic headaches
■ In extreme cases, degenerative arthritis of the cervical and thoracic spine
EVIDENCE
■ Netscher et al8
• Symptomatic hypermastia is better defined by symptom complex than by volume of tissue removed.
• Symptomatic hypermastia affects quality of life on par with other significant chronic medical conditions (e.g., kidney transplant, living with moderate angina pectoris).
• Symptoms are more important than volume in determining health burden and surgical benefit.
• Weight loss, special bras, and medical treatments are not successful.
AESTHETIC INDICATIONS
■ Women with hypermastia frequently report aesthetic dissatisfaction with breast size and shape.
■ Complaints include pendulous appearance and wide nipple-aerola complex.
■ Excessive size may limit clothing selection and athletic participation.
TIP: Determining the aesthetic or medical necessity of reduction mammaplasty is ambiguous and nonstandardized by health insurance carriers in the United States.
PREOPERATIVE EVALUATION
PATIENT HISTORY
■ Age (>50 years of age with higher complication rate, according to Shermak et al11)
■ Medical history of comorbid disease(s), clotting disorders
■ Surgical history pertaining to breast
■ Social history of smoking or nicotine use
■ Familial history of breast disease, anesthesia problems, deep vein thrombosis (DVT)
■ Breast history of lactation, changes with pregnancy and weight fluctuations, tumors
■ Previous medical or therapeutic treatment for hypermastia
PHYSICAL EXAMINATION
■ Sternal notch-to-nipple distance: Allows detection of asymmetry in nipple position
■ Nipple-to-inframammary fold distance: Serves as a measurement of the redundancy of the lower pole skin envelope
■ Base width: Allows detection of asymmetrical breast footprint
■ Areolar diameter: Widening of the areola is very common in patients with hypermastia (normal areolar diameter is 38-45 mm).
■ Classification of ptosis severity (see Chapter 52)
■ Breast examination for mass or lymphadenopathy
ADDITIONAL CONSIDERATIONS
■ Skin quality: Presence of striae indicates the inelastic quality of affected skin.
■ Parenchymal quality: Fatty, fibrous, or glandular parenchyma
MAMMOGRAM
■ When indicated
PHOTOGRAPHY (see Chapter 3)
■ Anteroposterior (AP), lateral, and oblique photographs should be obtained.
■ Photographs of shoulder grooving and rashes, when present.
PATIENT EXPECTATIONS
■ Breast shape
• Reduction mammaplasty will not result in a virginal breast.
• Most techniques will naturally result in a pendulous, mature-looking breast, but with a size more proportionate to the body habitus of the patient.
■ Breast size
• The desired postoperative breast size can vary widely between patients and should be dicussed at length at the initial consultation.
• Inform patients that complications with breast reduction are more common in larger reductions (>700 g) and in patients with a higher BMI.12
TIP: Although surgeons and patients frequently discuss bra-cup size, surgeons can better determine patients’ wishes by asking them to find representative photographs of the desired postoperative size in magazines or professional portfolios.
INFORMED CONSENT
Recommend items to be included in the informed consent:
■ A general description of the procedure and location of incisions
■ A sufficient description of potential risks
• Bleeding and hematoma
• Infection
• Delayed healing and wound separation
• Nipple necrosis, complete or partial
• Change in nipple and skin sensation
• Potential changes in breast-feeding
• DVT and pulmonary embolism (significant risk with BMI >3013)
• Asymmetry and poor cosmetic result
• Poor lactation (70% of patients can lactate after surgery, but many require supplementary feeding.)14,15,16
• Poor scar quality
SURGICAL OPTIONS
■ Most techniques described in Chapter 53 were initially developed for breast reduction. Most patients with hypermastia also have breast ptosis. For detailed information on short-scar techniques, please see Chapter 53.
■ Liposuction has been described as an additional or sole treatment for reduction mammaplasty.
■ Reduction mammaplasty by excision can be thought to include the following four elements:
1. Selecting a pedicle to provide vascularity and innervation to the nipple-areola complex (NAC)
2. Determining the quadrants of the breast from which to resect tissue
3. Excising excess skin after removal of breast parenchyma
4. Creating an overall aesthetic breast shape.17
SUCTION LIPECTOMY
■ Liposuction is often used in combination with excisional techniques to limit scar burden but can be used alone to reduce breast size.18
PATIENT SELECTION/INDICATIONS
■ Ideal candidates:
• Have a normally positioned NAC
• Good skin quality
• Predominantly fatty breasts.
■ A useful technique in elderly patients with significant symptoms of hypermastia and insignificant cosmetic concerns19
ADVANTAGES
■ Smaller scars
■ Preserves lactation and vascular supply to the NAC
■ Preserves existing sensation
■ Can be easily performed with local and intravenous sedation
DISADVANTAGES
■ Most surgeons agree that breast ptosis cannot be adequately treated with suction lipectomy alone and may be worsened in patients with poor skin quality.
■ Postoperative edema and induration often take months to resolve.
■ The evacuated breast tissue cannot effectively be sent for pathological evaluation.
• Unexpected breast malignancy may go undetected.20,21
• The absence of adequate pathological evaluation has brought controversy.15,22–24
TECHNIQUE
■ Lateral and medial inframammary fold (IMF) stab incisions are used.
■ Wetting solution is infiltrated.
■ 3-5 mm cannulas are used to treat both superficially and deep.
■ Postoperative compressive bras are worn for 6 weeks.
NOTE: Ultrasound-assisted liposuction has been used in the breast, but surgeons are advised to obtain exhaustive informed consents from their patients, discussing the unknown effects of ultrasonic energy on breast tissue.
EXCISIONAL TECHNIQUES
PEDICLE SELECTION
■ Options include inferior pedicle, superior/superomedial pedicle, and central mound technique.
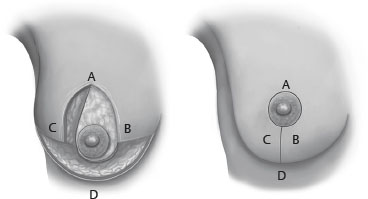
Inferior Pedicle (Fig. 55-1)

Fig. 55-1 Inferior pedicle technique.
■ Has been the preferred method (in the United States) and is easily teachable25
■ NAC maintained on an inferior dermal-parenchymal pedicle
■ Lateral, medial, and superior breast tissue can be removed.
■ Usually paired with an inverted-T skin excision
■ May use short-scar periareolar inferior pedicle (SPAIR) introduced by Hammond26
■ Advantages
• Large parenchymal resections can be done safely.
• Reliable neurovascular supply
• Lactation preserved in most patients14,15
• Low complication profile (11.4%)27
• When nipple to fold is >18 cm, the pedicle becomes bulky, limiting extent of reduction.
• Passive creation of breast shape from tailoring skin around parenchyma
• Often creates a boxy breast
• High rate of bottoming out
Superior/Superomedial Pedicle (Fig. 55-2)
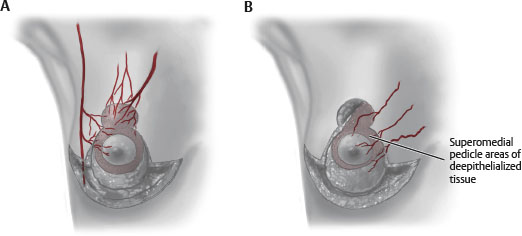
Fig. 55-2 A, Superior pedicle. B, Superomedial pedicle.
■ Lassus28,29 is credited with introduction of the superior pedicle technique.
■ Lejour22,30 is credited with refinements and popularization of the technique.
■ Hall-Findlay31popularized the superomedial pedicle.
■ Nahabedian and Mofid32 and Lista and Ahmad33 made contributions.
■ Modifications include Strombeck horizontal bipedicle technique.34
■ NAC is maintained on a superior or superomedial dermal-parenchymal pedicle.
■ Lateral, medial, and inferior breast tissue can be removed.
■ Advantages
• Large parenchymal resections can be done safely, and involve resection of the ptotic tissue.
• Pedicle is created from main blood supply of NAC.35
• Pedicle is superior, where fullness is commonly desired.
• Allows creation of inferior pillar support to limit bottoming out
• Ease of use with short-scar techniques
• Nipple-areolar sensation reliably maintained
■ Disadvantages
• Learning curve for technique
• Creates dead space at dependent part of breast, where fluid may accumulate
Central Mound Technique (Fig. 55-3)
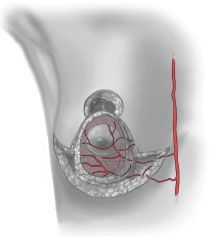
Fig. 55-3 Central pedicle/mound.
■ NAC is maintained on a central parenchymal pedicle (without dermis).
■ Breast tissue can be excised laterally, medially, superiorly, and inferiorly, leaving a central glandular component.
■ Advantages
• Less reliable nipple-areolar neurovascular supply
• Ideal to preserve lactation
• Allows variable resection of parenchyma in multiple quadrants
■ Disadvantages
• Underresection is common.
• Safety issues with undermining pedicle as blood supply comes from chest wall.
• Breast shape/support largely dependent on dermal support
• Possible bottoming out.
TIP: With all pedicle patterns, nipple viability should be checked before thinning the breast flaps. If the NAC is ischemic, the operation can be converted to a free nipple graft and the pedicle debrided to the appropriate level without compromising breast volume.
SKIN RESECTION PATTERNS
■ Mastopexy procedures (or very small reductions) allow periareolar incisions and skin resection alone, but this is inappropriate for use in patients with true hypermastia.
Vertical Pattern (Fig. 55-4)
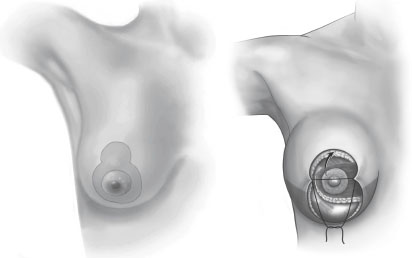
Fig. 55-4 Vertical pattern.
■ Allows excision of lax skin in horizontal dimension
■ With lateral (lazy-J) extension lax skin in the vertical dimension36,37
■ Some authors advocate tailor-tacking to facilitate incision placement.
■ Once desired shape and skin contour are obtained, the “tailored” resection pattern is marked and excised.
■ Other techniques avoid a transverse scar by gathering the skin in the vertical closure, leaving a dog-ear in the inframammary fold (IMF).31 This skin redundancy requires delayed excision in approximately 5% of patients.
• More recent evidence, however, cautions against the use of gathering sutures38
► Significantly reduce the incision length in the operating room but do not change the areola-to-IMF distance or pucker revision rate.
► Gathering negatively influences skin vascularity and wound healing.
SENIOR AUTHOR TIP: If the remaining dog-ear appears exceptionally large in the IMF, do not hesitate to excise it with a small horizontal excision. A small horizontal incisional scar is usually preferable to a revision procedure, even if done in the office.
Inverted-T (Wise) Pattern (Fig. 55-5)
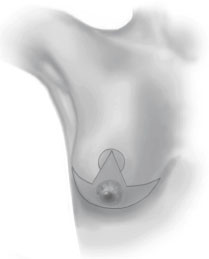
Fig. 55-5 Inverted-T pattern.
■ Skin excision includes both a vertical and horizontal excision.
■ Horizontal excess is removed through the vertical incision.
■ Vertical excess is removed with the horizontal excision placed in the inframammary fold.
■ Especially useful in large reductions with excessive amounts of skin redundancy
■ Wound separation is fairly common at the intersection point in the IMF.
SURGICAL TECHNIQUES
INFERIOR PEDICLE WITH INVERTED-T SKIN RESECTION39 (Fig. 55-6)
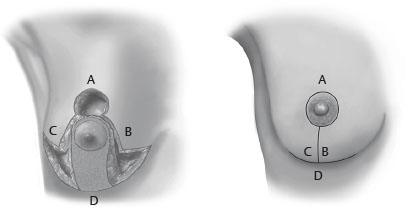
Fig. 55-6 Inferior pedicle with inverted-T skin resection.
Markings
■ Step 1: Place patient in an upright position.
■ Step 2: Mark the midline.
■ Step 3: Mark the breast meridian to determine a new horizontal nipple position.
■ Step 4: Mark the vertical nipple location (Pitanguy point) by transposition of IMF to front of breast.
■ Step 5: Mark the IMF position, elevating mark a few millimeters onto the breast. This keeps the IMF scar on the breast and not on the chest, because the base of the breast is narrowed during reduction.
■ Step 6: Measure bilaterally from notch to nipple and from midline to ensure symmetry.
■ Step 7: Mark the vertical limbs, which should measure approximately 7-8 cm under tension.
• Long limbs can always be shortened on the operating table; short limbs may result in closure under tension, which may compromise shape and skin viability.
• The angle of divergence determines amount of skin resection.
■ Step 8: Connect vertical limbs to the medial and lateral aspects of the IMF marking, following a lazy-S pattern.
■ Step 9: Mark the pedicle approximately 10-12 cm from the midline.
■ Step 10: Mark the areola at 42 mm; replace at 38 mm to minimize traction and distortion on the areola.
■ Step 11: Mark all areas to be liposuctioned.
Technical Tips
■ Develop the pedicle before raising skin flaps. To prevent undercutting, bevel away from pedicle.
■ Place the patient in a sitting position and tailor-tack, as needed, to achieve desired shape.
■ Hidalgo40 reviewed the inverted-T pattern markings, along with modifications to improve aesthetic outcome.