Authors
Years
Surgery
Description
Halsted [1]
1894
Radical mastectomy
Removal of the breast, two muscles and axillary lymph nodes
Stewart [2]
1915
Radical modified mastectomy
Transverse incision, better aesthetic result
Urban [3]
1956
Ultraradical mastectomy
Removal of the breast, two muscles, axillary lymph nodes, and internal mammary lymphatic chain en bloc
Patey and Dyson [4]
1948
Radical modified mastectomy
Resection of the breast, pectoralis minor muscle, and axillary contents en bloc
Madden [5]
1965
Radical modified mastectomy
Resection of the breast and axillary contents en bloc, preserving both pectoral muscles
Fisher et al. [6]
1985
Breast conservative treatment
Tumor resection (lumpectomy and quadrantectomy), axillary dissection and radiotherapy
Veronesi et al. [7]
1986
Breast conservative treatment
Tumor resection (quadrantectomy), axillary dissection and radiotherapy
Toth and Lappert [8]
1991
Skin-sparing mastectomy
Mastectomy appeared in order to conserve skin as much as possible and facilitate breast reconstruction.
Audretsch et al. [9]
1994
Oncoplastic surgery
Association of plastic surgery techniques for conservative treatment
Giuliano et al. [10]
1994
Sentinel node biopsy
To avoid complete axillary dissection
Petit et al. [11]
2006
Nipple-sparing mastectomy
Mastectomy appeared in order to conserve skin the and nipple–areola complex, facilitating breast reconstruction. Associated with intraoperative radiotherapy of the nipple–areola complex
Nava et al. [12]
2006
Skin-reducing mastectomy
Combined flap technique to reconstruct large and medium-sized ptotic breasts in a single-stage operation by use of anatomical permanent implants
Notably, the choice of the procedure depends on both the location and the stage of the cancer. The development of diagnostic imaging techniques has increased the medical profession’s awareness of breast cancer and has led to earlier diagnoses. Because a greater percentage of cancers are detected at earlier stages, the need for skin-sparing techniques has increased [13].
Skin-sparing mastectomy (SSM) is classified further by the type of incision used and the amount of skin removed (Fig. 26.1, Table 26.2). Type I SSM is used commonly for prophylactic purposes and for patients whose cancer was diagnosed by needle biopsy. Lateral extension of the incision may be necessary to improve exposure to the axillary tail. Type II SSM is used when the superficial tumor or previous biopsy was near the areola. Type III SSM is used when the superficial tumor or previous incision was remote from the areola. Type IV SSM is used in large, ptotic breasts when a reduction was planned on the opposite breast [14].
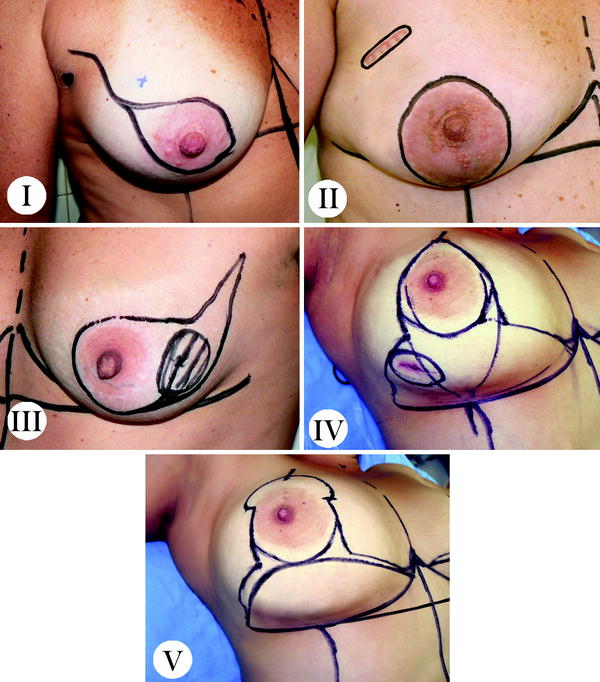
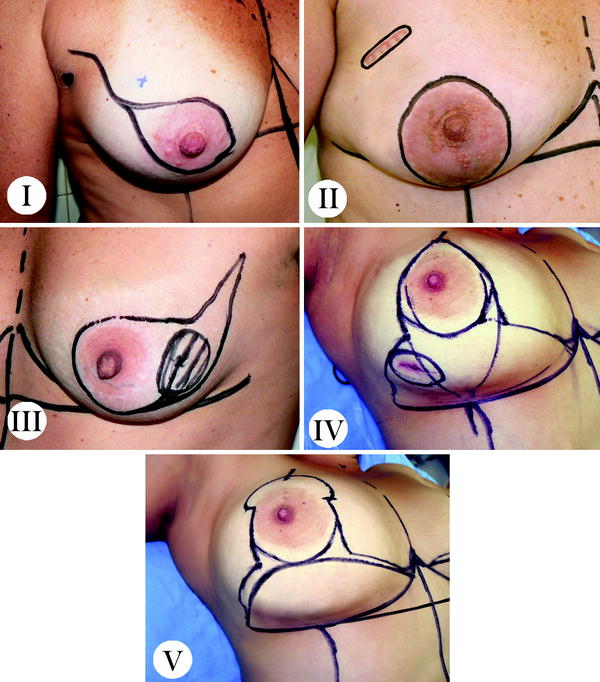
Fig. 26.1
Classification of skin-sparing mastectomy including skin-reducing mastectomy
Table 26.2
Modified classification of skin-sparing mastectomy
Type | Classification |
|---|---|
I | Only nipple–areola complex removed |
II | Nipple–areola complex, skin overlying superficial tumors, and previous biopsy incision removed in continuity with the nipple–areola complex |
III | Nipple–areola complex removed, skin overlying superficial tumors, and previous biopsy incision removed without intervening skin |
IV | Nipple–areola complex removed with an inverted or reduction pattern skin incision |
Type IV Wise-pattern SSM has had excellent results as immediate implant reconstruction in heavy- and pendulous-breasted patients who require a conspicuous reduction of the skin envelope and a contralateral reduction or mastopexy. However, on the side undergoing the SSM, the skin flaps are thin and wound-healing problems are well described, particularly skin necrosis at the ‘‘T’’ as frequently as 27 %, predisposing to prosthesis exposure and therefore limiting its utility [12]. Therefore, technique modifications that recruit local tissue to protect these areas of breakdown and support the implant have been proposed and the procedure has been called skin-reducing mastectomy (SRM; type V) [12, 15–17].
Reconstruction surgery in this subset of mastectomies can be performed by means of totally submuscular expanders or permanent prostheses rather than autologous flaps. Final scarring is similar to that from cosmetic surgery (inverted T) [12].
26.2 A Brief History
In different series of inverted-T mastectomies, relatively high morbidity (up to 27 %), which usually involved skin viability at the inverted-T junction, was reported [12]. In this way, many authors have tried to overcome necrosis and poor results using a modified Wise pattern rather than a subcutaneous pouch.
In 1990 Bostwick [18] tried to preserve a lower deepithelialized dermal flap during a Wise reduction pattern mastectomy to create a musculodermal pouch for the location of a definitive permanent silicone prosthesis that provided appropriate coverage of the implant. At that time there was no information about the possibility of saving skin during oncological procedures, so it was used for prophylactic mastectomies.
Hammond et al. [19] introduced Bostwick’s method in the treatment of breast cancer, in most cases using a two-step surgical approach with temporary expanders, followed by a second operation for permanent insertion of implants.
In 2006, Nava et al. [12] described a modification of this last type of SSM, renamed skin-reducing mastectomy (SRM), by which mammary reconstruction in selected patients is done in a single stage in which an anatomical silicone gel implant is placed in a dermal muscle flap pocket. They aimed to avoid complications of the type IV operation, such as lack of space in the inferior and medial aspects of the submuscular pouch that sometimes requires release of the inferior insertions of pectoralis major muscle with an incision, leaving the implant subcutaneously with a high risk of exposure, particularly when it is put under the long (and possibly ischemic) superior mastectomy flap.
26.3 Definition
SRM is a single-stage technique that helps us to overcome the cosmetic inadequacy of a type IV Wise-pattern SSM (final inverted-T scar) in heavy and pendulous breasts by filling the lower medial quadrant with adequate volume.
Its virtue lies in the manner it provides adequate implant coverage using muscle and a deepithelialized dermal flap, thus reducing the risk of implant extrusion and providing a good inframammary contour [17].
SRM with a complete release of the pectoralis muscle inferiorly and the sparing of a lower dermal flap sculpted down to the inframammary fold allows the creation of a dermomuscular pouch, achieving total implant coverage and overcoming all of the inadequacies of type IV SSM (upper pole fullness and lack of projection). By augmentation of the pocket and provision of a new tissue layer at the lower pole of the breast, complications are reduced and aesthetic outcomes are improved compared with the traditional inverted-T mastectomies.
26.4 Indications
SRM was originally deemed most suitable for early-stage breast cancer and risk-reduction patients with medium-sized to large breasts; however, the indications for its use could be expanded.
Ongoing controversies continue to result in the issues of SSM and sparing of the nipple–areola complex being debated. These controversies are focused on problems of nipple–areola complex survival and the reliability of methods from an oncologic point of view. Many published reports describe the reliability of subcutaneous mastectomy in certain indications. In early-stage breast cancer, immediate breast reconstruction after subcutaneous mastectomy is used with increasing frequency.
Recently, risk reducing mastectomy has been performed for patients displaying the following oncologic risk factors: a positive family history, BRCA1 and BRCA2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree