52. Breast Augmentation
Evan B. Katzel, Thornwell H. Parker III, Jeffrey E. Janis, Dennis C. Hammond
BACKGROUND
■ Breast augmentation is the second most common cosmetic surgery (after liposuction).1
■ Silicone implants were introduced in 1964.
■ Saline implants were introduced in 1970s as an alternative to silicone.
■ The U.S. FDA placed a moratorium on silicone implants in 1992 for primary augmentation because of concerns about autoimmune and connective tissue disease.
• In 1999 the NIH Institute of Medicine and the National Academy of Sciences reviewed 17 epidemiologic studies and were unable to detect any link between silicone and systemic, autoimmune, or prenatal disease.
• Studies found silicone in local macrophages, lymph nodes, and breast tissue.
• Studies did not demonstrate elevated systemic levels (normal liver, lung, and spleen).2
■ Saline implants increased in popularity during the 1990s because of silicone scare.
■ Silicone implants have evolved through different generations (Table 52-1).
Table 52-1 Generations of Silicone Gel-Filled Breast Implants
| Implant Generation | Production Period | Characteristics |
| First | 1960s | Thick shell (0.25 mm average) Thick viscous gel Dacron patch |
| Second | 1970s | Thin shell (0.13 mm average) Less viscous gel No patch |
| Third | 1980s | Thick, silica-reinforced barrier coated shells |
| Fourth | 1992-present | Stricter manufacturing standards Refined third-generation devices |
| Fifth | 1993-present | Cohesive silicone gel-filled devices Inner laminar layer to prevent gel bleed Form-stable devices |
NOTE: Some consider the introduction of textured surfaces and anatomic shapes to represent fourth or fifth generations.
■ Restriction on use of silicone gel implants for primary breast augmentation was lifted in November 2006.
• Before this change, silicone implants were approved only for breast reconstruction, silicone implant exchange, and replacement of saline implants with complications.3,4
■ Cohesive gel implants are considered to offer significant advantages.
• In Europe since 1995
• In Canada since 2000
• Advantages: More natural shape, less rippling, limited gel migration in event of rupture
• Disadvantages: Larger incision, more expensive, stiffer
INDICATIONS AND CONTRAINDICATIONS
INDICATIONS
■ Increase breast size
■ Restore prelactation breast appearance
■ Correct breast asymmetry
■ Enhance breast shape and volume
■ Improve body image, symmetry, and balance
■ Improves fit of clothing
■ Provide the appearance of a breast lift and increased cleavage
■ Rejuvenation after postpartum deflation
CONTRAINDICATIONS5
■ Significant breast disease (e.g., severe fibrocystic disease, ductal hyperplasia, breast cancer)
■ Collagen vascular disease
■ Body dysmorphic disorder
■ Psychological instability
■ Social instability (e.g., divorce or separation, searching for a relationship)
■ Patient responding to pressure from friends, family, or partner
■ Patient <18 years of age
■ Silicone implants are not FDA approved for women <22 years of age (see Chapter 1).
■ The following situations require mindfulness6:
• After obtaining the history, the surgeon does not like the patient.
• Patient desires an outcome the surgeon cannot deliver.
• Patient desires an outcome outside the surgeon’s aesthetic sense of normal.
• Patient is critical of previous surgeons or praises the current surgeon excessively.
• Patient lies, provides a false history or information.
• Patient refuses to be examined or photographed.
• Patient is a perfectionist and wants a guarantee of results.
• Patient is paranoid, delusional, or depressed.
• Patient fails to communicate or is unable to understand what informed consent entails.
PREOPERATIVE EVALUATION
HISTORY/INTERVIEW
■ Begins with open-ended questions
■ The patient talks and the surgeon listens.
■ Assessment:
• Motivation for surgery
• Psychological state of mind and stability
• Expectations
• Self-esteem
MEDICAL HISTORY
■ Full medical history
• Personal or family history of breast disease or cancer
• Pregnancy history and plans for future pregnancies
• Breast size before, during, and after pregnancy
• Mammography history (recommended for patients >35 years of age and those with significant breast cancer risk)
• Patients without significant history should have a mammogram every 2 years starting at 40 years of age, and every year beginning at 50 years of age.7
• Previous surgeries or procedures on breasts
• Previous cosmetic procedures
• Tobacco or nicotine replacement use, drug use
• Anticoagulation use
• Current breast size
• Desired breast size (many patients will bring pictures to clinic)
PHYSICAL EXAMINATION
■ Breast examination
• Masses, dimpling, discharge, lymph nodes
• Cancer screening
■ Skin quality
• Stretch marks, tone, elasticity
■ Asymmetries: Chest wall, scoliosis, breast
• Difference in breast volume
• Difference in inframammary fold (IMF) height
• Difference in nipple-areolar complex (NAC) height
■ Soft tissue pinch test
• <2 cm, may obtain a better result with a submuscular implant placement
• Ptosis (see Chapter 53)
• Mild ptosis is improved by augmentation.
• Moderate to severe ptosis may require mastopexy.
■ Measurements (patient sitting up straight)
• Breast width at its widest point
• Breast height
• Intermammary distance
• Mark true midline of the chest
• Mark IMF
• Height, weight, body frame (small to large)
• Sternal notch to nipple (SN-N)
• Nipple to inframammary fold (N-IMF) during stretch
• Base width (width of breast base)
• Parenchymal coverage (pinch test)
• Superior pole
• Lower pole
• Anterior-pull skin stretch (centimeters of anterior stretch with pull at edge of areola)
• Parenchymal fill (percentage of skin envelope filled by parenchyma)
■ Photographs (all jewelry and identifying markers removed) (see Chapter 3)
• Chin to below navel
• Front, lateral, oblique, with arms at rest and elevated
■ Point out and document
• Chest wall deformities
• Spinal curvature
• Asymmetries (nipple shape and size, nipple position, IMF position, breast size, breast ptosis)
INFORMED CONSENT
■ Not just signing a paper
■ Photographic review
• Note asymmetries, ptosis, cleavage.
• Note that asymmetries, ptosis, and cleavage are often unchanged or even accentuated by breast augmentation alone.
■ Implant selection
• Review and discuss risks and benefits of implant type, texture, volume, positioning, and access incisions.
• Review and discuss previous restrictions on silicone implants.
■ The patient must be thoroughly informed about:
• Risks and complications
• Bleeding
• Infection
• Capsular contracture
• Change in nipple and skin sensation
• Scarring
• Breast calcifications
• Breast implant-associated anaplastic large cell lymphoma (BIA-ALCL)
• Seroma
• Hematoma
• Breast venous thrombosis
• Implant failure
• Implant extrusion
• Changes in mammography detection
• Implant visibility and palpability
• Implant wrinkling or rippling
• Implant malposition or displacement
• Leakage of filling substance
• Rare difficulties with breast-feeding
• Chest wall deformation
• Animation deformities (if submuscular)
• Limitations of high-impact activity
• Unsatisfactory result
• The need for additional surgeries
► Many insurance carriers do not cover cosmetic operations, correction of complications that may arise from surgery, and changes that necessitate revision surgery.
• Implant weight, aging, weight loss or gain, and pregnancy will result in expected changes in breast appearance.
• Benefits
► Enhances natural body contour
► Corrects loss of volume after pregnancy and lactation
► Balances asymmetries
► Replaces ruptured or displaced implants
• Alternatives
► Silicone versus saline
► Fat grafting
► Autologous tissue transfer
► No surgery
■ Can use official ASPS informed consents
■ Document desired implant type, size, and shape discussed with patient.
EQUIPMENT
INSTRUMENTATION
■ Double hooks
■ Lighted breast retractor versus headlight
■ Army-Navy retractors
■ Extended Bovie tip
■ Endoscopic retractor (transaxillary approach, transumbilical augmentation)
■ Closed-loop saline-filled setup (saline-filled implants)
■ Implant sizers (if applicable)
■ Triple antibiotic solution
• 50,000 units bacitracin, 1g cefazolin, 80mg gentamicin per 500 ml saline solution (may reduce infection rate and capsular contracture)8
■ Keller funnel (Allergan)
• Allows no-touch insertion of silicone implant through minimal-sized incision
■ Implants
FILLER MATERIAL
Saline
■ Advantages
• Historically lower contracture rates
• Adjusts quickly to body core temperature
• Leaks easily detected and safely absorbed by body
• Size more customizable—easier to adjust for size and correct breast asymmetry
■ Disadvantages
• Wrinkling
• Less natural look and feel
• Complete deflation with leak
■ Construction
• Silicone shell filled with physiologic saline solution
Silicone
■ Advantages
• More natural feel and appearance than saline implants
■ Disadvantages
• Historically higher contracture rate
• Must be ≥22 years of age to receive silicone implant per FDA
• Adjusts slowly to temperature change (e.g., implants remain cold after swimming)
• Ruptures more difficult to detect and can cause local inflammation and granulomas
• MRI recommended 3 years after surgery, then every 2 years to monitor for rupture, as per FDA
• More expensive
■ Construction
• Silicone shell with silicone filler
• Silicone: Polymer of dimethylsiloxane. Longer chains with greater interchain cross-linking lead to increased viscosity.
Double-Lumen (Becker Implant, Mentor)
■ Advantages
• Natural feel of silicone
• Allows postoperative adjustments to inner-lumen saline volume
• Useful for asymmetry and for patients uncertain of desired size
■ Disadvantages
• Fill port temporarily implanted, requiring second procedure to remove
• Possible fill valve failure
■ Construction
• Outer and inner silicone shell: Outer lumen filled with silicone, and adjustable inner lumen filled with saline
VOLUME
■ Patient preference
• Sizers put in bra to establish desired volume (not recommended)
• Photos of other women
• Digital imaging
■ Surgeon’s experience
• 125-150 cc to increase by one cup size
• Larger body frames require larger implant volumes to increase cup size
■ Breast analysis
• High Five system9
• Objective measures to determine optimal implant and volume
• Volume based on breast base width
• Add or subtract volume based on skin stretch, breast envelope fill, and N-IMF
■ Intraoperative breast sizers
■ Pitfalls of large implant volume
• Stretching and stressing of tissues
• Atrophy and thinning of parenchyma and skin
• Increased palpability
• Traction rippling
CAUTION: Large implant can have detrimental effects on overlying soft tissues.
TEXTURE
SMOOTH
■ Advantages
• Thinner capsule formed
• Less palpable: Preferable for patients with thin coverage
■ Disadvantages
• Higher contracture rates
• Requires larger pocket dissection
• Requires displacement exercises to prevent contracture
TEXTURED
■ All shaped implants are textured to prevent malposition.
■ Advantages
• Lower contracture rate (surface disorients collagen deposition)
• Less migration and implant rotation
■ Disadvantages
• Require precise pocket dissection
• More palpable
• Traction rippling more common
• Greater association with BIA-ALCL based on current data
■ Technique
• Intraoperative positioning of implant is critical, because textured surface resists migration or movement in pocket.
• Base must be properly oriented along IMF.
POLYURETHANE-COVERED
■ Advantage
• Dramatically low contracture rates (<1% over 10 years)
■ Disadvantage
• Pulled from U.S. market, because polyurethane breaks down as a carcinogenic compound, although levels likely insignificant
■ Construction
• Polyurethane coating separates over weeks to months and becomes incorporated into the capsule, helping to disperse contractile forces.
• Textured implants were developed to mimic the effect of polyurethane on the capsule.
SHAPE/DIMENSION
ROUND (CIRCULAR IMPLANT)
■ Advantages
• Offered in many different projections and sizes
■ Disadvantages
• Less natural appearance
■ Low-profile
■ Moderate-profile
■ High-profile
• Increased projection for given base width
• Increased projection with less volume
• Advantage with a constricted lower pole or a narrow breast base width
SHAPED/ANATOMIC
■ Implant height different than width
■ Increased implant height and projection for a given base width
■ Upper pole tapered; fuller lower pole, reducing upper pole collapse and filling out lower pole of breast
■ Most textured to maintain position
■ Advantages
• Designed to give more natural appearance
• Less upper pole fullness
• More natural upper pole contour
■ Disadvantage
• Must be oriented properly and symmetrically
• More prone to malposition
• Fewer available implant sizes in the United States
SIZE
■ Based on:
• Patient’s desired size and projection
• Breast base width
• Implant should be slightly narrower than the patient’s breast width
• Dimensions and compliance of the patient’s breast
■ High-volume implants (>400 cc) are more prone to complications.
• Many surgeons have special consent forms for such implants.
• Rule of thumb: 125-150 cc per cup size increase
SENIOR AUTHOR TIP: While the anatomically shaped implants may help with the creation of natural breast contours, the real advantage of these devices is that they are wrinkle resistant. As a result of the anatomic shape of the shell combined with the more cohesive gel, these devices resist collapse and wrinkle formation which greatly reduces stress on the shell resulting from fold flaw failure. As a result, the rupture rates at 10 years for these devices are impressively low which can make these implants an attractive option for patients and surgeons alike.
TECHNIQUE
MARKINGS
■ IMF
■ True midline
POCKET POSITION
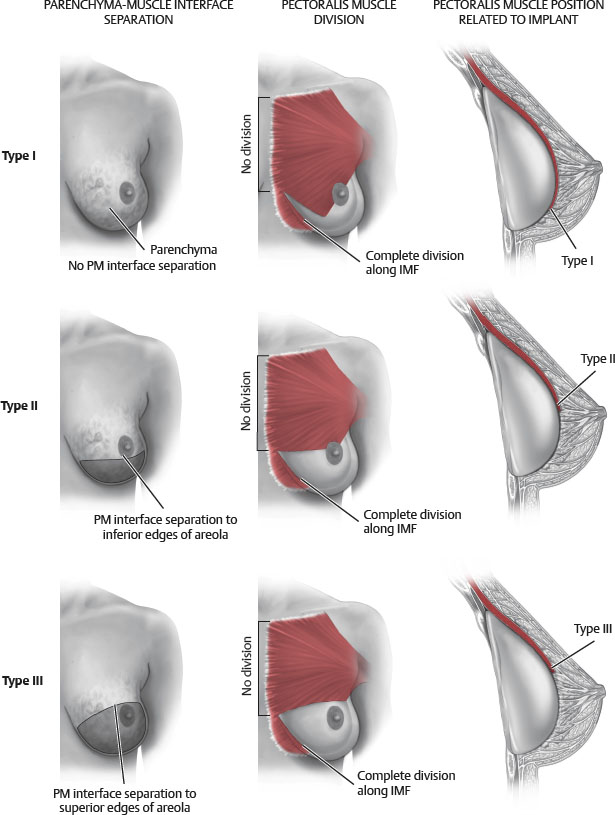
■ Pocket dissection is based on type of implant (Fig. 52-1).
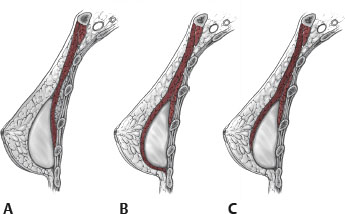
Fig. 52-1 Pocket plane and dissection.
A, Subglandular augmentation.
B, Submuscular augmentation.
C, Biplanar augmentation.
• Smooth gel implants can use larger pockets and displacement exercises to prevent capsular contracture formation.
• Textured implants are placed in and are only slightly larger than the footprint of the implant to minimize malposition.
Subglandular/Subfascial
■ Subglandular: The implant rests under the breast gland.
■ Subfascial: The implant is placed under the anterior pectoralis major fascia and the pectoralis major muscle.
■ Advantages
• Avoids implant distortion with pectoralis activity and in muscular patients
• More anatomic
• Better implant projection
■ Disadvantages
• Higher capsular contracture rate
• Visible implant wrinkling or rippling, especially if paucity of native breast tissue
• Implant edges may be palpable
• Interference with mammography
■ Technique
• Dissection on top of pectoralis major, below gland
• If pinch test is greater than 2 cm, the implant can safely be placed in the subglandular/subfascial plane.
► Thin parenchymal coverage if upper pole pinch test is <2 cm
Total Subpectoral
■ Rarely performed in cosmetic surgery
■ Advantages
• Lowest capsular contracture rates (<10%)
• Thick soft tissue coverage
• Good preservation of nipple sensation
■ Disadvantages
• Implant shifts with pectoralis activity
• “Dancing breasts” during pectoralis contraction
• Implant malposition over time (superiorly and laterally)
• Difficult to control upper pole fill
■ Relative contraindication
• Muscular or active patient
■ Technique
• Dissection below pectoralis major but above pectoralis minor
• The implant is placed completely under the pectoralis major muscle
• Does not disrupt inferior attachments of pectoralis if “total subpectoral”
Dual Plane10
■ The origin of the pectoralis major is completely divided from its origin at the level of the IMF, stopping at the medial aspect of the IMF.
■ The upper pole of the implant is placed under the pectoralis, and the lower pole is placed subglandularly.
■ The attachments of the pectoralis to the breast parenchyma are selectively divided. (The amount of dissection differentiates dual plane type I, II, and III.)
■ Advantages
• Decreases implant displacement caused by pectoralis contraction
• Provides thick upper pole soft tissue coverage with subpectoral placement
• Lower capsular contracture rates than with subglandular placement
• Increased control of IMF position compared to submuscular
• The breast parenchyma and the pectoralis can be dissected apart to adjust for differing types of breasts.
• Low contracture rate
• Increases implant-parenchymal interface, which expands lower pole and prevents double-bubble deformity
■ Disadvantage
• Usually restricted to IMF incision when performing dual plane II and III
■ Contraindication
• IMF pinch test <0.4 cm
■ Rationale
• Complete muscle coverage restricts expansion of inferior pole, forcing implant superiorly and laterally.
• Especially with ptotic and loose breast parenchyma, breast tissue may slide inferior to the axis of the implant while implant remains fixed higher on the chest wall, causing a type A double-bubble deformity.
• Dual plane techniques release inferior pectoralis attachments, allowing some pectoralis retraction superiorly.
• This maximizes implant contact with lower pole breast parenchyma, with the advantage of upper pole coverage by the pectoralis.
■ Dual plane type I10 (Fig. 52-2)