Breast Aesthetics in the Nonoperated and Reoperative Breast
Obtaining the optimal aesthetic outcome in breast surgery is a goal that every breast surgeon strives to achieve, but it is also a goal that often remains elusive. Although definitions of the ideal breast exist, each surgeon’s attempts at such creation are an internalized artistic vision that is brought to the operating table after careful preoperative assessment and planning. This can be a learned form of artistry. It requires experience, surgical skill, and the ability to understand the particular patient’s concerns and anatomic challenges.
Breast aesthetics are determined by the shape, volume, and position of the breast mound relative to a patient’s anterior torso. To optimize the aesthetic outcome, the surgeon must be able to image what alteration he or she is trying to create in a particular patient’s breast with regard to these relationships. In addition, the surgeon must take into account how expected alterations will be affected by wound healing, eventual softening, and gravitational settling of the breast’s tissues following surgery.
Breast aesthetics involves two senses: the visual and the tactile. Visual characteristics that are most important are symmetry, contour, flow, and proportion. The main tactile features are softness, mobility of the breast tissues on the chest wall, and the patient’s individual breast sensitivity. As previously noted, I believe that it is important for every surgeon to preoperatively image what alteration he or she is trying to create in a particular patient’s breast. This is achieved by developing a concept of a normal attractive breast with an understanding of how breast landmarks and a particular patient’s anatomic features and proportions contribute to it.
BREAST DEVELOPMENT AND ANATOMIC DISTRIBUTION
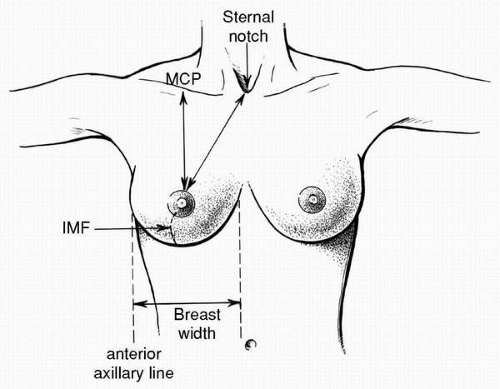
Anatomically, the breast vertically overlies the second through sixth ribs (Fig. 2-1). In the horizontal dimension it most typically extends from the lateral sternal border to the mid axillary line (Fig. 2-2). On frontal view the breast extends beyond the lateral margin of the ribs as it flows toward the lateral edge of the latissimus dorsi muscle (Fig. 2-2). This horizontal dimension at the widest point of the inferior-most aspect of the breast on the frontal view
represents the base width, which is an important visual characteristic (Fig. 2-3). Differences in breast base width are readily recognized as asymmetries, especially in the setting of reconstructive breast surgery. This dimension is critical for tissue expander and implant selection, as well as serving as an important benchmark for revision surgery planning.
represents the base width, which is an important visual characteristic (Fig. 2-3). Differences in breast base width are readily recognized as asymmetries, especially in the setting of reconstructive breast surgery. This dimension is critical for tissue expander and implant selection, as well as serving as an important benchmark for revision surgery planning.
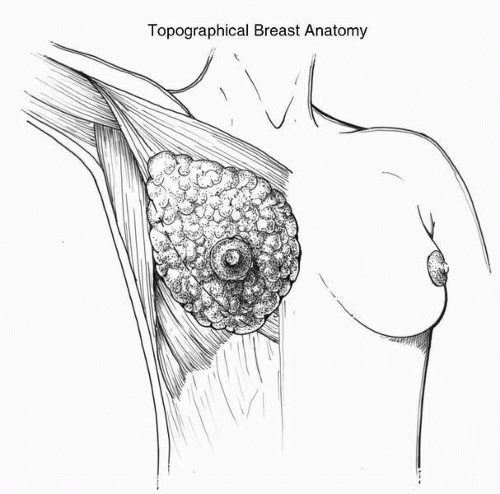 FIGURE 2-1. Topographical distribution of the breast parenchyma extending from the second to the sixth rib. Note that the lower pole extends below the origin of the pectoralis major muscle. |
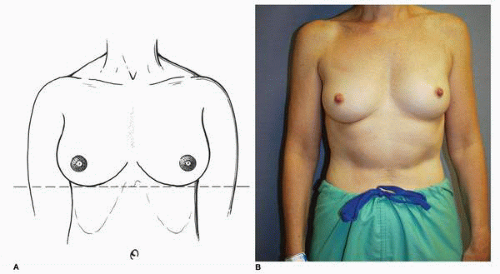 FIGURE 2-2. In AP view the breast extends from the parasternal area laterally beyond the lateral rib margin. |
These anatomic boundaries and surface relationships are foreshadowed by events that take place early after fertilization leads to the creation of the embryo. The breast develops in utero along the mammary ridge, which is a line that extends from the axilla to the groin (Fig. 2-4). The breast bud develops from an ectodermal precursor, which invaginates at the sixth week of in utero development such that this aggregate of ectoderm (which is the breast in the developing embryo) comes to lie beneath the skin. This embryologic breast then actually develops within the anterior and posterior layers of the superficial fascia of the chest wall. Although there are foci of breast tissue precursors along the entire mammary ridge (Fig. 2-4), in the normal situation only the aggregate in the fourth intercostal space persists after birth, and thus this accounts for the normal topographic location of the breast. Persistence of breast tissue elsewhere along this line can be present as supranumerary nipples (Fig. 2-5) or as ectopic breast tissue (Fig. 2-6).
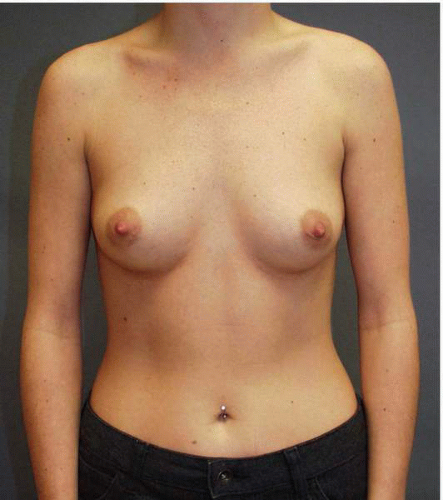
Normal breast development begins at approximately 10 years of age at the time of puberty and is usually complete by 16 to 18 years of age. Under the influence of various hormones, most notably estrogen, the gland assumes a rounded, hemispheric shape characteristic of puberty (Fig. 2-7A). The volume,
or parenchyma, is predominantly distributed as a round lower pole, which in youth projects maximally at the nipple and tapers to fill the upper hemisphere of the breast (Fig. 2-7B).
or parenchyma, is predominantly distributed as a round lower pole, which in youth projects maximally at the nipple and tapers to fill the upper hemisphere of the breast (Fig. 2-7B).
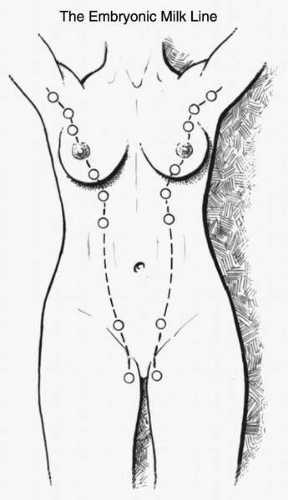 FIGURE 2-4. Depiction of mammary ridge, or milk line, extending from axilla to groin—noted in embryo. |
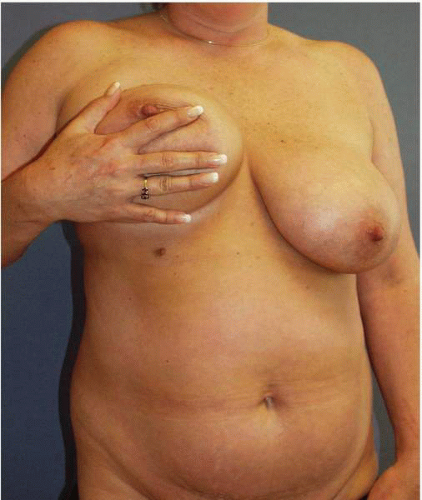 FIGURE 2-5. Supernumerary nipple noted in the milk line. This is the most commonly encountered congenital breast abnormality. |
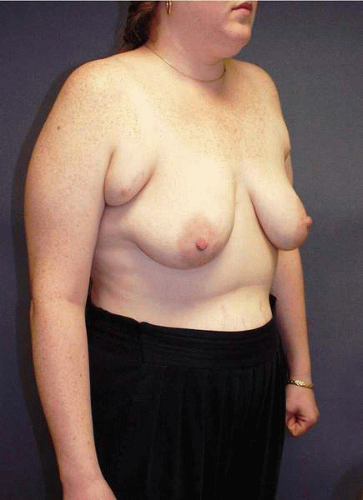 FIGURE 2-6. Ectopic breast tissue with accompanying nipples noted bilaterally in the axilla. Patients often request excision of this degree of tissue. |
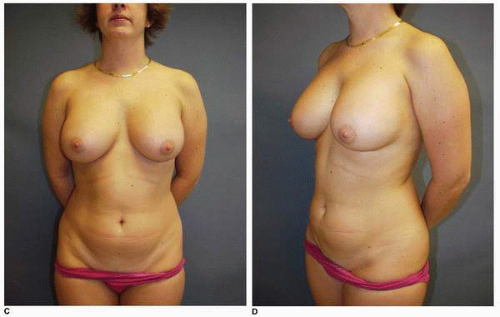
After puberty, the parenchyma becomes less firm as the patient ages and the ratio of adipose tissue to breast tissue increases. The breast parenchyma, therefore, contributes to the feel of the breast and to its elasticity. This elasticity changes and decreases with alterations in weight, age, and hormonal milieu—most notably pregnancy (Fig. 2-7C-E).
DETERMINANTS OF BREAST AESTHETICS
Breast aesthetics are determined by the volume, parenchymal distribution, tissue elasticity, the location and appearance of the nipple areolar complex (NAC), the quality of the skin envelope, and the relationship of the resulting breast to the patient’s anterior chest structures. Of paramount importance is the visual relationship of one breast to its counterpart on the opposite side of the midline. Simply stated, these components produce the image of breast shape and symmetry (Fig. 2-8).
Breast Volume and Skin Envelope
The ideal breast (Fig. 2-8) exhibits elasticity of the skin and parenchyma, a majority of volume in the lower pole, and an NAC that is at the highest point of the breast mound. On frontal or anteroposterior (AP) view the breast has less fullness in the upper pole and more fullness below and lateral to the NAC in the lower pole. On lateral view the breast parenchyma is positioned above the inframammary (IM) fold and exhibits roundness of the lower pole and a subtle fullness above the NAC, a feature that is especially noted in youth.
Nipple Areolar Complex
The NAC (Fig. 2-9) is central to breast aesthetics. It is the visual focal point of the breast and the eye is immediately drawn to it. All breast lines flow toward it. In the youthful breast it is usually located at the highest point of the breast mound along the midbreast meridian, which is a perpendicular line dropped from the midclavicular point inferiorly (Fig. 2-10). It is located slightly above the IM fold. It has approximately 4 to 6 mm of projection on the average and slight medial inclination. In most patients, the areolar diameter varies between 38 and 42 mm and exhibits a characteristic color that is notable. That is to say, the color in the nipple and areola is often a strong contributing factor to breast aesthetics. The position of the NAC may differ between breasts in a particular patient. With aging the NAC assumes a more dependent position on the breast mound (see Fig. 2-7E). The relationship of the NAC to the IM fold and the breast parenchyma is very important as it forms the basis of the most commonly used classification of mammary ptosis (Fig. 2-11).1 It is the hallmark of defining the youthful, aesthetic appearance of the breast. This relationship of the NAC to the breast mound forms the basis of a system of applied aesthetics as described in the following section, wherein the IM fold is used to help determine the new position of the NAC when it is relocated during bilateral mammoplasty.
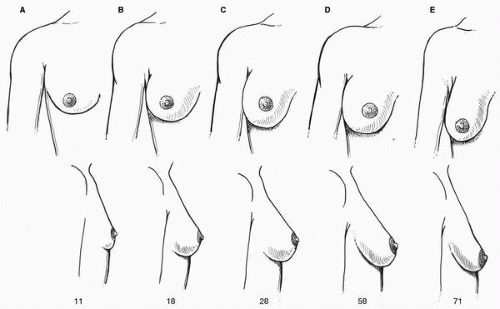 FIGURE 2-7. A-E, Changes in shape of breast gland as a function of age. Note progressive degree of ptosis. |
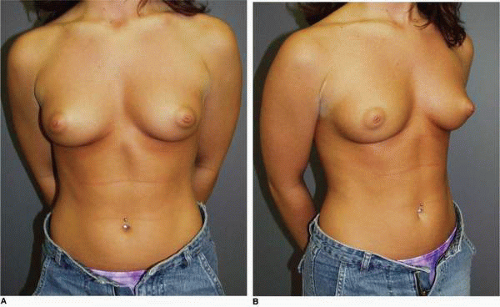 FIGURE 2-8. Parenchymal distribution and skin envelope appearance of the teenage (A, B) and mature (C, D) female breast. |
APPLIED AESTHETICS
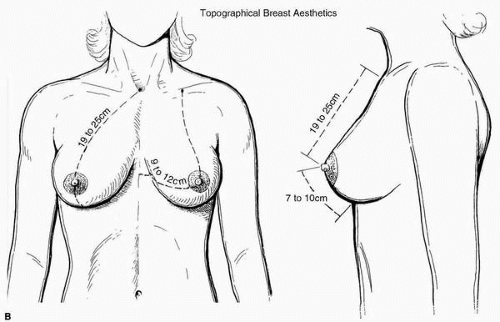
A simplification of breast aesthetic analysis may be done using topographical measurements from fixed points on the torso to points on the breast itself. It is most common to use the suprasternal notch (SSN), nipple location, breast base width, and distance from the nipple to the IM fold (see Fig. 2-3). As previously mentioned, the NAC is the focal point of the breast (see Fig. 2-9). For this reason, determining new nipple position is a critical part of every procedure on the breast. As noted earlier, this is often done by using distances from a fixed reference point such as the SSN, the midline of the sternum, and midposition of the clavicle. The midmeridian of the breast is defined by a line dropped in a perpendicular manner from the midpoint of the clavicle, which is midway between the SSN and the acromioclavicular joint. The nipple is most often situated on a line 19 to 25 cm from the SSN in the midmeridian of the breast, depending on the patient’s height. In youth it is best envisioned at or slightly above a transposition of the IM fold. The method for establishing the optimal position of the nipple during mammoplasty has been classically taught by placing one’s middle
finger behind the breast to project the position of the IM fold anteriorly (Fig. 2-11). If done incorrectly (and it is commonly done incorrectly) this can result in too high a placement of the nipple. For this reason I believe that the most accurate way of establishing nipple position based on the IM fold level is by placing a tape measure directly in the fold (Fig. 2-12). The utility and reliability of this maneuver is illustrated in later chapters.
finger behind the breast to project the position of the IM fold anteriorly (Fig. 2-11). If done incorrectly (and it is commonly done incorrectly) this can result in too high a placement of the nipple. For this reason I believe that the most accurate way of establishing nipple position based on the IM fold level is by placing a tape measure directly in the fold (Fig. 2-12). The utility and reliability of this maneuver is illustrated in later chapters.
The distance from the midsternal line to the nipple is usually between 9 and 12 cm, and the average distance between the nipple and the IM fold varies between 7 and 10 cm. The base width of the breast in the frontal view varies between 11 and 16 cm in most patients, and the distance over the surface of the breast skin from the lateral sternal border to the midaxillary line at the level of the nipple is most often 17 to 23 cm. I find it helpful to record these dimensions on a diagram in the chart of every patient (see Fig. 3-2).
It is important for the plastic surgeon to recognize that these distances are relative and that real aesthetic relationships vary according to a particular patient’s height, weight, body build, heredity, and age.
The fallibility of clinging to absolute measurements alone when planning a breast operation is perhaps best illustrated by focusing on the distance from the SSN to the nipple. An often-cited publication from the 1950s suggests that the position of the nipple on the breast mound relative to the SSN
forms an equilateral triangle with the SSN to nipple distance being 21 cm and the internipple distance also being 21 cm.2 A careful reading of the paper reveals that the subjects who were studied were “healthy young volunteers,” namely thin women in the late teens or early twenties. I have not found that this article pertains to most of the patients I see in consultation for breast surgery, especially patients I am evaluating for a revisional surgical procedure. That is to say, the distance from the SSN to the nipple is not 21 cm in the majority of patients I have encountered in the reoperative setting. Therefore, positioning the nipple at this distance may be unwise and inappropriate for many patients. Rather, the specific anatomy, height, weight, and tissue elasticity of each patient must be taken into account when planning a revision mammoplasty in which the NAC will be transposed.
forms an equilateral triangle with the SSN to nipple distance being 21 cm and the internipple distance also being 21 cm.2 A careful reading of the paper reveals that the subjects who were studied were “healthy young volunteers,” namely thin women in the late teens or early twenties. I have not found that this article pertains to most of the patients I see in consultation for breast surgery, especially patients I am evaluating for a revisional surgical procedure. That is to say, the distance from the SSN to the nipple is not 21 cm in the majority of patients I have encountered in the reoperative setting. Therefore, positioning the nipple at this distance may be unwise and inappropriate for many patients. Rather, the specific anatomy, height, weight, and tissue elasticity of each patient must be taken into account when planning a revision mammoplasty in which the NAC will be transposed.
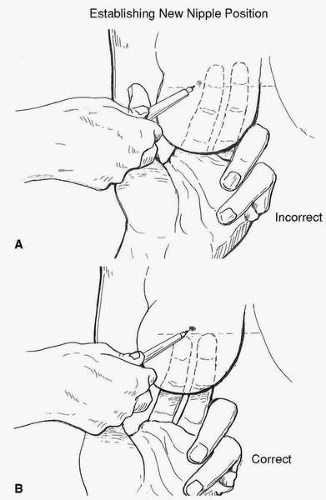 FIGURE 2-11. A-B, Use of the middle finger to indicate the transposition of the IM fold to the anterior breast. It is important not to displace the fold too superiorly (incorrect method). |
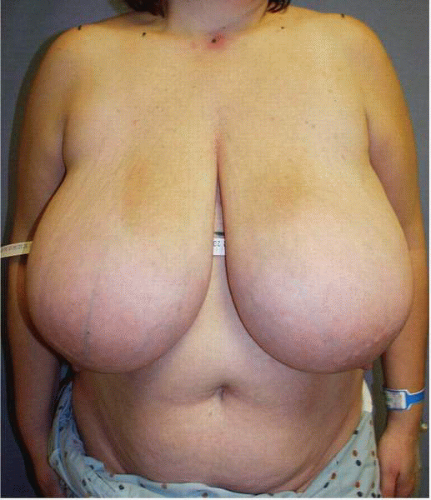 FIGURE 2-12. A more accurate delineation of the IM fold level is obtained by placing a tape measure in the IM fold and drawing a line on the skin. |
Nevertheless it is common, and I believe helpful, to use quantitative measurements in reoperative surgery of the breast. Measurements of the breast base width and vertical height recorded in centimeters (see Fig. 2-3) are important aides in selecting the appropriate implant or tissue expander, for establishing the skin paddle dimensions on flaps that are transferred to the breast in a patient undergoing a delayed or redo breast reconstruction (Fig. 2-13), and for adjusting the skin envelope (by adding or removing skin) in a given revision procedure. These dimensions provide a framework for planning specific maneuvers and for selecting certain techniques rather than others. In addition, referring to them after the procedure is completed allows the surgeon to verify the accuracy of such planning and to develop a sense of predictability relative to the outcome of such planning.
BREAST SUPPORTING STRUCTURES
Cooper’s Ligaments
The breast actually develops within the anterior and posterior layers of the superficial fascia of the chest wall. During the first three decades of life the shape of the breast is largely determined by the support conferred to the parenchyma via condensations of connective tissue arising from the pectoralis muscle fascia, which run through the interlobular planes of the breast gland and insert on the dermis (Fig. 2-14). These ligaments were first described by Sir Astley Cooper and are thus called Cooper’s ligaments. They are the most important supporting structure of the breast from an anatomic standpoint. These structures are not visible during breast surgery and therefore they cannot be reconstructed. They are inelastic. Therefore, when they are stretched beyond a certain point they cannot recoil, and subsequently their ability to support the breast parenchyma is severely compromised. This stretching of Cooper’s ligaments is most commonly noted following pregnancy or with large or repeated fluctuations in a patient’s weight. These two conditions represent the most common clinical situations producing a marked change in the shape of a patient’s breast.
Skin
The skin is an essential medium for breast appearance, and it contributes strongly to overall breast aesthetics. By its essential features of color and elasticity, the skin conveys a sense of beauty and youthfulness to the breast. In addition, its elasticity helps determine breast shape.
In youth the skin is relatively taut (see Fig. 2-8), but changes during aging produce thinning and loss of elasticity. In the absence of previous surgery, changes in the skin that are typically encountered by the plastic surgeon during a consultation with a patient requesting a breast procedure include altered skin elasticity. These changes are seen in this nulliparous 35-year-old athletic patient with significant (grade III) breast ptosis (Fig. 2-15A).
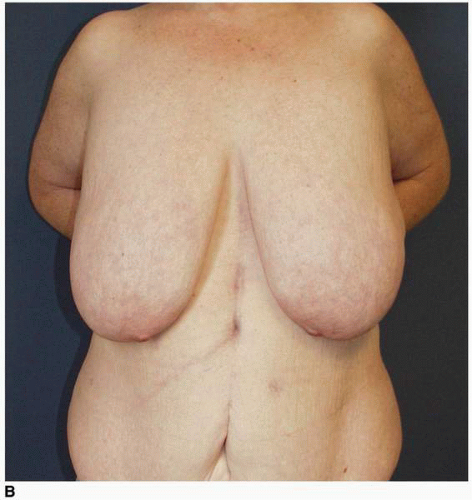
Most often this is marked by the presence of striae (which are physical evidence of rupture of the elastin fibers within the breast skin), a prominent superficial subcutaneous vessel pattern that is most often a visible network of fine reticular blood vessels, or skin that is simply stretched. These skin changes are most commonly seen in the setting of macromastia associated with obesity or breast ptosis due to postpartum involution, significant weight loss (Fig. 2-15B), or repeated fluctuations in a patient’s weight.
Most often this is marked by the presence of striae (which are physical evidence of rupture of the elastin fibers within the breast skin), a prominent superficial subcutaneous vessel pattern that is most often a visible network of fine reticular blood vessels, or skin that is simply stretched. These skin changes are most commonly seen in the setting of macromastia associated with obesity or breast ptosis due to postpartum involution, significant weight loss (Fig. 2-15B), or repeated fluctuations in a patient’s weight.
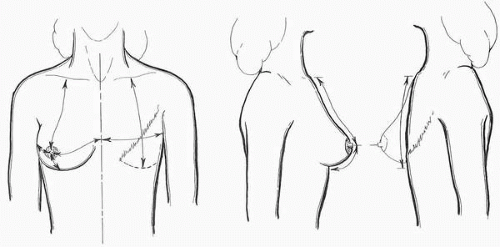 FIGURE 2-13. Careful measurement of the quantitative skin deficiency in both the vertical and horizontal dimension is part of the planning for every delayed breast reconstruction as illustrated. |
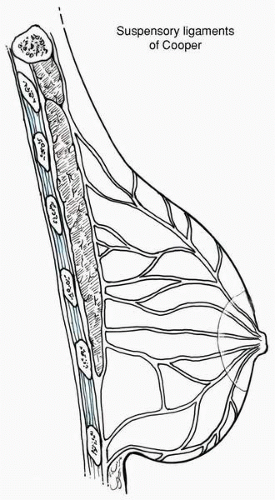 FIGURE 2-14. The anatomic position of Cooper’s ligaments course through the parenchyma in the interlobular area of the breast. |
In most patients progressive thinning of the skin occurs with aging, thus reducing the skin’s contribution to breast support and maintaining shape (see Fig. 2-7E). The presence of decreased skin elasticity is important to note because it is a predictor of recurrent ptosis or gravitational changes following many breast procedures in which skin support is relied on to maintain a change in shape. Despite these limitations imposed by aging and the other factors noted, historically the skin has been the medium of the breast that is most often altered by plastic surgeons in procedures aimed at improving breast aesthetics. Newer breast reshaping operations such as vertical scar mammoplasty rely on parenchymal reshaping with internal suturing to more significantly maintain changes in breast shape and improved aesthetics. These parenchymal reshaping and stabilizing techniques may improve the longevity of changes they produce in the breast.
Inframammary Fold
The IM fold is the most important architectural element for defining the shape and appearance of the female breast. In my opinion, the IM fold is perhaps the key structure for determining breast aesthetics in almost all operative and reoperative breast cases. It is the foundation on which the breast is configured, and it contributes strongly to shape, projection, and upper pole fullness when the patient is standing upright. Therefore a careful analysis of the fold for shape, degree of development or tightness, and symmetry constitutes an important part of every aesthetic analysis of the breast that is conducted before surgery. An understanding of IM fold anatomy and its contribution to the breast shape or problems with breast shape in a particular patient is a critical tool in the breast surgeon’s surgical repertoire.
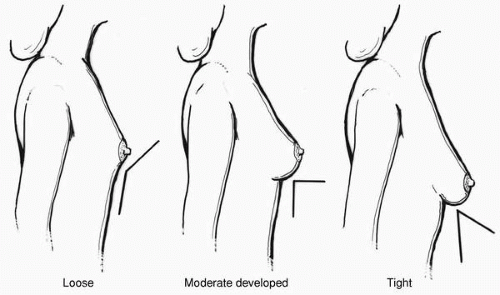
Clinically the IM fold extends from the parasternal area to the anterior axillary line in the frontal view. This fold subtends a smooth convex downward curve, which is most often symmetric when the breasts are examined in the AP view (Fig. 2-16). Very importantly, I have come to recognize that the IM fold displays different degrees of development in different patients. That is to say, it displays various degrees of looseness or tightness in a given individual (Fig. 2-17A-C). The curve or convexity of the fold is most often symmetric, but any areas of asymmetry must be noted. The most inferior or lowest point of the IM fold lies on or close to the vertically oriented midbreast meridian, which is a vertical line drawn from the midclavicular point through the most projecting point of the breast, which usually corresponds to the nipple (see Fig. 2-10). The fold is positioned 4 to 6 cm from the lower areolar margin in small- to medium-size breasts and 7 to 9 cm in larger breasts.
The architecture and histologic composition of the IM fold has been studied for more than 150 years, beginning with Sir Astley Cooper’s description in 1845.3 However, there is still considerable debate about its exact anatomic makeup. I have reviewed many of the recently published anatomic studies and have derived the following concepts regarding the anatomy of the IM fold from these studies and from 20 years of surgical experience.4-6
The IM fold is formed by the condensation of connective tissue arising from the superficial fascia that extend vertically, coursing superficially through the subcutaneous tissue to insert into the dermis at the IM fold, producing the characteristic appearance of the fold. To a much lesser degree some of these vertical fibrous bands extend deep to the superficial fascia toward the pectoralis major muscle (PMM).
The relative definition or tightness of the IM fold varies in different patients (see Fig. 2-17A-C). I believe that the IM fold definition is related to the density of connective tissue relative to the amount of adipose tissue (the ratio of fibrous tissue to subcutaneous adipose tissue) in the fold. The greater the amount of adipose tissue, the lesser the definition of the fold. Conversely, the lesser the amount of subcutaneous adipose tissue and the greater the concentration of fibrous tissue, the more developed or tight the IM fold development (Fig. 2-18A,B). In some patients with tight folds, these connective tissue condensations may extend below the superficial fascia toward the pectoralis muscle fascia in greater concentration. That is to say there are more fibrous elements connecting the superficial fascial system (SFS) to the PMM fascia in patients with tight folds.
As previously outlined, most embryologists believe that the breast develops within a split of the SFS (i.e., between the anterior and posterior layers of this fascia) on the anterior trunk.1 These layers of the superficial fascia form the corresponding anterior and posterior capsule layers of the breast. As illustrated in Figure 2-1, the breast proper extends from the second to the sixth intercostal space. Therefore the lower aspect of the breast extends well below the origin of the PMM and its fascia in most patients. For this reason I do not believe that there is a ligament joining these fibrous tissue elements to the pectoralis muscle fascia as has been suggested.6 I believe that most of the vertically oriented fibrous connective tissue elements that are responsible for creating the fold lie between the SFS layer and the skin.4
 FIGURE 2-15. A, Decreased skin elasticity in this nulliparous patient with major (grade III) ptosis. B, Massive weight loss patients have an extreme form of this condition. |
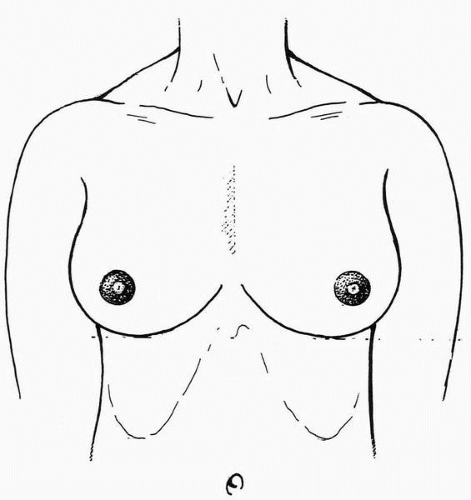 FIGURE 2-16. IM fold seen on AP view as a convex downward arc extending from parasternal area to anterior axillary line. |
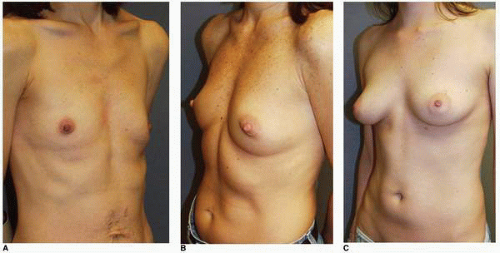 FIGURE 2-17. Clinical variations in the tightness of the IM fold. A, Loose fold. B, Moderately tight fold. C, Extremely tight fold. |
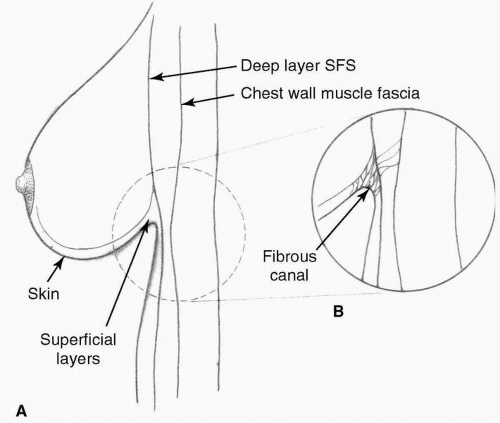 FIGURE 2-18. A-B, The density of the fibrous connective tissue in the fold determines its degree of looseness or tightness. (From Acland PRS Feb 2002, with permission.) |
As noted earlier, clinically the fold outlines an arc beginning near the midline in the parasternal area and continues laterally, where it extends to the lateral aspect of the breast at its juncture with the lateral chest wall at the anterior axillary line (see Fig. 2-16). Different patients exhibit different degrees of development of the IM fold. These vary from a loose fold, or no development of the IM fold, to a moderately tight fold, or moderate development of the IM fold, to a tight IM fold (see Fig. 2-17A-C). I envision and classify the various degrees of tightness of the IM fold in different patients as illustrated in Figure 2-19.
The degree of tightness of the fold has a definite effect not only on breast shape, but also on the selection of procedure for certain breast operations. This is true for both cosmetic and reconstructive breast surgical procedures.
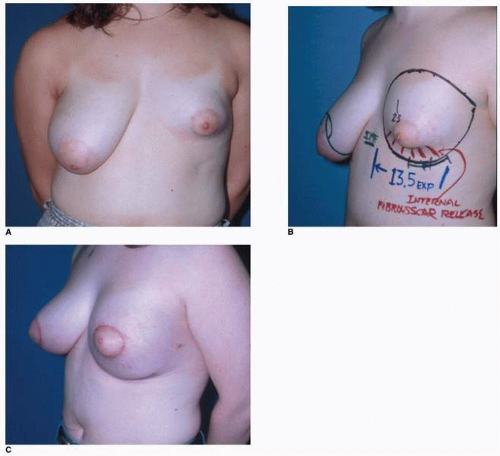
For example, from a clinical standpoint I do not believe it is routinely possible to completely eradicate and redefine or reset a tight IM fold in most cases. This becomes important in breast augmentation in a patient with an extremely tight fold where lowering of the IM fold is planned as part of a breast augmentation. If such a maneuver (attempting to lower a tight IM fold by placing an implant beneath it) is carried out in a patient with a very tight fold, a not uncommon sequela is the appearance of a “double bubble” (Fig. 2-20). On the other hand, in reconstruction of the constricted breast deformity (Fig. 2-21A-C), releasing, remolding, and reshaping the tight IM fold is essential. This is best accomplished with an operation that entails a complete disinsertion of the breast parenchyma from the skin above and the PMM fascia below, coupled with the placement of an implant. In some cases with an extremely tight fold, a two-staged approach with the release described earlier, along with the placement of a tissue expander to gradually mold a new IM fold contour, followed by the placement of an implant, may be most effective in resetting and reconstructing the fold from the perspective of optimizing symmetry and avoiding a double bubble deformity. I make additional comments on this in Chapter 3.
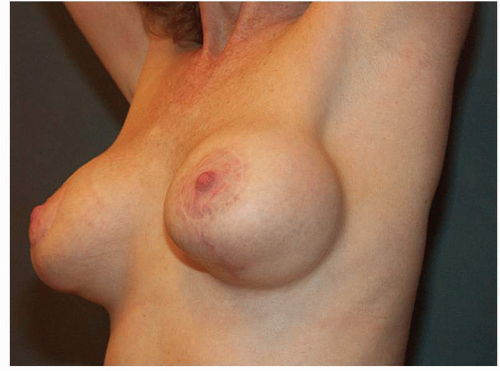 FIGURE 2-20. The double bubble is created when a subpectoral implant is positioned below a tight IM fold. |
Most often the IM fold is roughly symmetric when comparing both breasts. However, the surgeon must carefully note any element of asymmetry in the position and the architecture of the IM fold as both breasts are analyzed. Be aware that abnormalities in the IM fold architecture can have a profound effect on virtually every breast surgical procedure from the standpoint of affecting symmetry. Asymmetry in the level of the IM fold is a very commonly noted abnormality following previous breast surgery (Fig. 2-22A,B) and is one that often requires correction with revisional breast surgery to achieve a better aesthetic result (Fig. 2-22C).
Possible deformities produced by variations in the IM fold development include a spectrum of constricted breast deformities and a frank tuberous or tubular breast deformity (see Fig. 2-23A-C). A classification of this constriction is proposed by Grolleau et al.7 Diagrammatically it is illustrated in Figure 2-24. The constricted breast (see Fig. 2-21A,B




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree