(1)
University of Pittsburgh Medical Center, Pittsburgh, PA, USA
Electronic supplementary materialThe online version of this chapter (doi:10.1007/978-3-662-46976-7_4) contains supplementary material, which is available to authorized users.
4.1 Background: Enhancing Female Features
After massive weight loss (MWL), pregnancies, and aging, concerned women request body-contouring surgery to remove lose skin and raise and reshape ptotic breasts, mons pubis, and buttocks. While the skin is being tightened and raised, subcutaneous deposits of adipose need to be feminized. Soft tissue and musculoskeletal female aesthetics (Sect. 2.2) are analyzed in the context of patient demands. Regardless of final BMI, MWL often leads to an androgynous appearance. Shaping curves are unique challenges for each body type. An optimal, complex surgical treatment plan is proposed, which is adjusted by the patient’s goals.
Comprehensive surgery is demonstrated through a variety of case presentations (Table 4.1). Each case brings a perspective to meeting challenges of deformity and patient expectations. Most cases have before images and preoperative surgical markings and an identical set of after views for comparison. Most of the instructive cases are organized by regions in Sects. 4.3 and 4.4. Section 4.6 focuses on autogenous breast reshaping for Mommy Makeover. As the bridge between the upper torso and thighs, abdominoplasty is the keystone operation. Its position in a single-stage TBL is the focus of Case 4.4. Unless the lower body is massively oversized or the patient prefers otherwise, complex surgical rehabilitation starts with the lower body and thighs. Accordingly, Sect. 4.3 details though photographs and video the lower body lift (LBL) thighplasty combination. Following that clinical introduction, there is a discussion of the surgical dynamics. A major concern remains disturbing partial recurrence of saddlebag deformity. Despite initial optimism (Hurwitz et al. 2004), severe saddlebags at times partially recur after a LBL. The deformity appears corrected at a month, but recurrence may occur within 6 months (Fig. 3.5). Sections 4.43–4.46 are TBL surgery with upper body lift transverse excision with Spiral Flap reshaping of the breast (Hurwitz and Agha-Mohammedi 2006). A shapely back is routinely obtained without having a scar cross the posterior midline. Brachioplasty with liposuction is presented. Sections 4.4.5–4.4.11 have TBL that included J-torsoplasty reshaping of the breasts (Clavijo-Alvarez and Hurwitz 2012). In that procedure scars are avoided across the mid back entirely. The combining liposuction with L-brachioplasty in an oversized arm is presented on video. Section 4.6 is devoted to Mommy Makeover single-stage TBL for both thin and overweight patients. In either case, the effort is for sensuous lines. The latest VASER technology for cellulite correction is introduced. With its incredible sparing of neurovasculature and structural elastic connective tissue, the sophisticated use of VASERlipo plays a major role in primary TBL surgery and residual deformity (Sect. 3.5).
Table 4.1
Demonstrative case presentations
Case | Operation | Lessons |
|---|---|---|
4.1 | Fleur de Lys abdominoplasty (FDL) with oblique flank excisions, spiral thighplasty/vertical extension | Optimal combination to feminize mid and lower torso with reasonable scars in young. Marking spiral thighplasty/vertical extension |
4.2 | Lipoabdominoplasty/oblique flank excisions, buttock lipoaug. | Effectively deepening waist with oblique flank excisions, VASER techn. |
4.3 | VASERlipo of torso, thighs, buttock lipoaug. | Staging torso VASERlipo/buttock lipoaugmentation, lipoabdom |
2nd stage: VASERlipo thighs, lipoabdominoplasty, buttock lipoaug. | Aggressive epigastric VASERlipo in high central lipoabdominoplasty | |
4.4 | Lipoabdom, lower body lift (LBL), spiral thighplasty/vertical ext. buttock augmentation flap, Quill suspension mastopexy | Complex single stage TBL. With intraoperative photos of buttock flap aug., central high tension abdominoplasty, Quill suspension mastopexy |
4.5 | LBL, spiral thighplasty/vert. buttock augmentation flap | LBL technique, spiral thighplasty/vert. in thin, severe deformity |
2nd stage: implant aug./mastopexy | Mastopexy, saline breast aug. under local, with no late sag | |
3rd stage: VASERlipo revision, lipoaugmentation of hips | Successful VASERlipo of recurrent saddlebags | |
4.6 | LBL, spiral thighplasty/limited vertical extension | Aggressive surgery for mild thigh skin sag, no saddlebag recurrence |
4.7 | FDL, LBL, spiral thighplasty/vertical extension | Video of markings and operation of severe deformity |
4.8 | FDL, picture frame monsplasty, spiral thighplasty/vert. extensive UAL | Intraoperative photos, spiral thighplasty, monsplasty in obese patient |
2nd stage: knee, legplasty | Successful direct reduction of legs and supra patella regions | |
4.9 | Abdominoplasty, LBL, butt flap augmentation, L brachioplasty | Treating severe thigh deformity followed by recurrent saddlebags |
2nd stage: aug./mastopexy, revision brachioplasty, spiral thighplasty/vert. | Breast ptosis treated with saline implants and Wise pattern mastop. | |
3rd stage: VASERlipo correction of secondary saddlebags | VASERlipo corrects secondary saddlebags | |
4.10 | Spiral breast reshaping, circumferential transverse upper body lift | Multiple heavy back rolls requiring transverse bra line UBL |
4.11 | Spiral breast, transverse UBL, L brachioplasty, LBL, horizontal thighplasty | Details of spiral flaps, noncircumferential UBL |
2nd stage: breast aug., vertical thighplasty | 10-year result, UBL and brachioplasty are OK, LBL sags | |
4.12 | FDL, LBL, spiral thighplasty/vertical extension | Obese, typical first stage TBL with severe deformity |
2nd stage: transverse UBL, spiral flap breast reshaping, L brachioplasty | Complete photos of operation, excellent late result despite weight gain | |
4.13 | L brachioplasty, spiral flap breast reshaping, transverse UBL, limited vert. thighplasty, abdominoplasty | 5-year result of single stage TBL in over weight patient in supine position only |
4.14 | L brachioplasty, spiral breast reshaping, transverse UBL, abdominoplasty, LBL, spiral thighplasty/vertical extension | Desired small breasts, 8-year excellent result with single stage TBL in ideal candidate |
4.15 | L brachioplasty, spiral flap breast reshaping, UBL, abdominoplasty LBL, buttock flap | 5-year excellent of result single stage TBL despite 20 pound weight loss she maintained contours |
4.16 | L brachioplasty, spiral breast reshaping, J-torsoplasty, FDL | Single stage supine TBL. Marking for FDL and J-torsoplasty |
2nd stage: vert. thighplasty, UAL thighs | Breast shape/position good contours and faded scar at two years | |
4.17 | FDL, LBL, buttock flap | Excessive lower body size, large mid torso rolls |
2nd stage: L brachioplasty, spiral flap breast reshaping, J-torsoplasty | Video of markings, operation, full breasts, partial saddlebag recurrence | |
3rd stage: VASERlipo, back scar revision | 60 pound weight gain partially reversed through liposuction | |
4.18 | Abdominoplasty, LBL, butt flap | Staged TBL shaping of an ectomorph |
2nd stage: L brach, spiral flap breast reshaping, J-torsoplasty | 2-year follow up with feminine curves | |
4.19 | L brachioplasty, FDL, LBL | Photos of marking and operation of L brachioplasty. Good result |
4.20 | L brachioplasty, abdominoplasty revision, breast reduction | Video of markings and operation of L brachioplasty with liposuction |
2nd stage: VASERlipo | 40 pound weight gain contours of back and arms reversed by VASERlipo | |
4.21 | Spiral flap, J-torsoplasty, limited abdominoplasty, VASERlipo | Complex Mommy Makeover with breast reshaping without an implant |
4.22 | Quill suspension mastopexy, abdominoplasty followed by VASERlipo | Over corrected mastopexy with Quill suspension technique, scarring after laser liposuction |
4.23 | Quill suspension mastopexy | 2-year excellent Quill suture suspension mastopexy |
The underlying theme is gender-specific surgery. The first case attempts to sculpture a female from an androgynous form through a Fleur De Lys abdominoplasty (FDL) extended posteriorly along the bulging flanks and inferiorly with a spiral thighplasty and a medial vertical extension.
4.1.1 Case 4.1 Androgynous to Feminine Form
Case 4.1, 5′ 2″, 155 lb, requests staged TBL surgery to remove excess skin of her torso and extremities. She desires a feminine shape without enlargement of her breasts and buttocks. Tormented by her oversized body and hanging pannus throughout childhood, she suffers from depression and self-mutilation. She stopped her antidepressants, changed her lifestyle, and rapidly lost 100 of her 250 lb (Fig. 4.1). As is customary, the lower body and thighs are treated first. Her saddlebags were negligible, and her buttocks are already slightly flat, so a lower body lift (LBL) is not indicated. A combination of midtorso operations are designed to maximally narrow her midtorso, accentuate her hips and buttocks, and taper her thighs. Inclusion of many of her self-inflicted epigastric scars was an added benefit of the FDL. Markings for her FDL extend obliquely with excisions directly over her flanks, a picture frame monsplasty, and a spiral thighplasty with vertical medial extensions down the thighs (Fig. 4.2). The progression of the spiral thighplasty markings is diagramed (Figs. 4.3, 4.4, 4.5, 4.6, 4.7, and 4.8). After the loose skin of her lower torso and thighs was removed, her result is seen 8 months later (Fig. 4.9). The FDL and oblique excision of the bulging flanks combined for a deeper waist and rounder hips and buttocks. The thighs are now smooth and conical with scars within the labial thigh crease, under her medial buttock fold, and posterior to the medial longitudinal line. The technical details to perform these operations are described in subsequent case reports. Case 4.1 is an interplay of wide and deep tissue excisions. Extreme bulging tissues, as seen in her epigastrium and flanks, were excised directly and thoroughly. When fully explained to the patient, he or she will agree that significantly improved contours make longer and more visible scars acceptable. Fortunately, her scars faded rapidly. Her upper body lift, brachioplasty, and breast reshaping are scheduled next year.
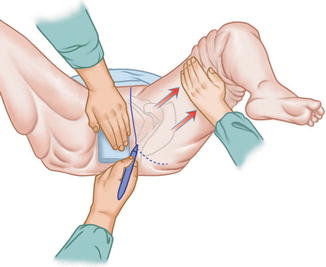
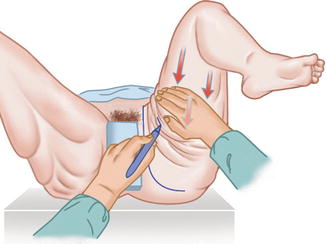
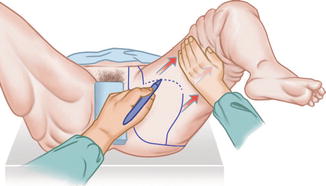
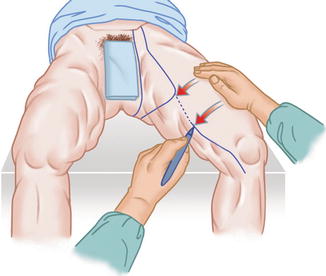
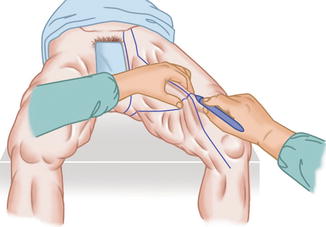
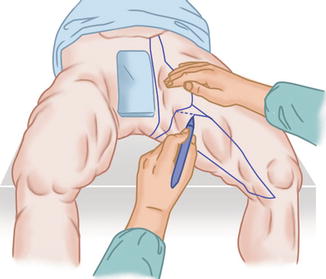
Fig. 4.1
Case 4.1 lost 100 lb and presented for first-stage TBL surgery for removal of lose skin and to create a more feminine appearance. Right anterior oblique (a), right lateral (b), and posterior (c) views convey the loose skin and broad androgynous shape
Fig. 4.2
The markings for Case 4.1 are for Fleur de Lys abdominoplasty (FDL) with large oblique excision extensions across the flanks, a picture frame pubic monsplasty, and spiral thighplasty with medial vertical extensions to her knees
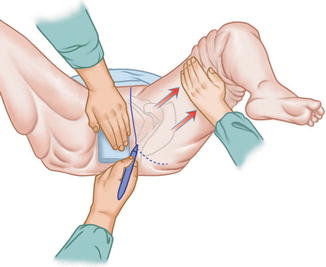
Fig. 4.3
Drawing of spiral thighplasty, 1: 6–7 cm from the suprapubic midline, a vertical is drawn between the mons pubis and groin and then continued as seen here between the labia majora and the medial thigh skin, as the thigh is abducted
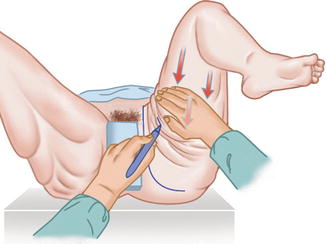
Fig. 4.4
Drawing of spiral thighplasty. 2: The inferior limit of the horizontal excision is marked in the medial midline with the thigh adducted
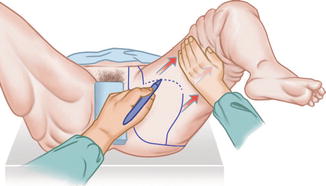
Fig. 4.5
Drawing of spiral thighplasty. 3: Continuing from a vertical excision line parallel to the first public line, a crescent incision is drawn out to meet the horizontal excision mark on the medial thigh
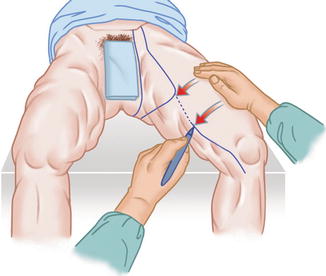
Fig. 4.6
Drawing of spiral thighplasty. 4: Dragging loose anterior thigh skin medially, a vertical incision line from labia to the knee is placed slightly posterior to the mid-medial line
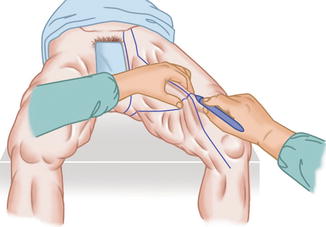
Fig. 4.7
Drawing of spiral thighplasty. 5: At the mid-medial thigh, excess medial thigh skin is gathered at the maximal width of excision and marked
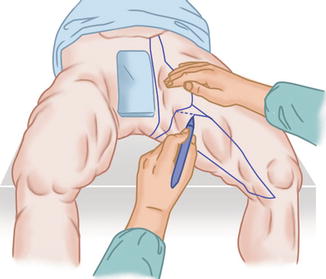
Fig. 4.8
Drawing of spiral thighplasty. 6: The anterior line of excision is adjusted slightly posterior to minimize the visibility of the scar and to avoid over resection of skin where the cone of the thigh is widest
Fig. 4.9
Case 4.1: Result 8 months later shows removal of pannus and loses thigh skin with feminine reshaping of her waist, hips, and thighs. (a) In right anterior oblique view, excess abdominal skin has been clearly removed. A smooth slightly rounded contour of the lower abdomen to mons pubis. The waist is narrowed and smoothly transitions to broader hips. Conical thighs smoothly taper to the knees. Vertical medial thigh scars lie just posterior to the medial midline. (b) Right lateral shows a deeper waist that transitions to a rounder buttocks. The high oblique scar is no issue. (c) Posterior view shows the buttocks is smaller, circumference, better defined, and round. The symmetrical thin flank scars are acceptable
As was the situation in Case 4.1, the FDL is usually selected when there is epigastric scarring. Other indications are considerable upper abdominal transverse skin laxity, or the patient desires the greatest reduction of the midtorso but refuses upper body lift surgery. The spiral thighplasty with a medial vertical extension is commonly performed at the same stage as the abdominoplasty with no troublesome competing vectors of tension at closure. The operations that most deeply carve out the waist are an FDL and direct oblique excisions of the flanks.
4.1.2 Case 4.2 Feminizing an older MWL Patient
Case 4.2 is a 59 year old with a BMI of 27, 3 years after losing 65 pounds from Lap band surgery. She seeks removal of mid and lower torso rolls. Never blessed with a sensual form, she agreed to maximum accentuation of her waist and fat augmentation of her buttocks. She is marked for VASER lipoabdominoplasty, deep oblique flank excisions and lipoaugmentation of the buttocks (Fig. 4.10 upper). Video 4.1 presents the essential markings and procedures to create this transformation. The operation began with her lipoabdominoplasty that included VASER removal and harvesting of 2,100 cc. of fat emulsion from the entire abdomen extended to the lateral lower chest. After turning her prone, the flank excisions were performed. 300 cc. of processed fat was injected into each buttocks. The use of VASER for removal and processing fat for lipoaugmentation is shown in detail (Video 4.1). Her early postoperative result reveals tight, flat abdomen with deep long waists, more so on her right then her left, because she had that structural asymmetry to start with (Fig. 4.10 lower). Her buttocks are shorter, wider and more projecting. She happily wears form fitting clothes that reveal her appealing curvaceous torso.
Fig. 4.10
Case 4.2 Frontal and right posterior oblique views before and after feminizing body contouring surgery. Upper. Moderately excess mid and lower torso fat with sagging skin. Broad flanks indistinctly flow over her hips to narrow flat buttocks. Lower abdomen contours are distorted by a midline vertical surgical scar. Markings are for lipoabdominoplasty with oblique flank excisions, plus marks 2,100 cc. liposuction and green minus marks for 300 cc. lipoaugmentation of each buttock. Note the midlateral torso liposuction markings to help narrow the waist both superior and close to the oblique excisions. Lower. Result at 5 weeks show the desired improved abdominal contours have been obtained with the long low lying symmetrical abdominal scar that obliquely extends over the iliac crests to the mid back. Deep waists abruptly expand over the hips to broader, more projecting and firm buttocks
4.2 Integrating Central High-Tension Lipoabdominoplasty
With only a long low-lying scar and reliable superb abdominal contours, central high-tension lipoabdominoplasty (CHTLA) is the preferred abdominoplasty procedure. Due to its location, CHTLA is the keystone operation between upper body, back, and thigh surgery. Usually that means CHTLA is sandwiched between the upper and lower body lifts and thighplasties. With the advanced capabilities of new liposuction technologies, such as VASERlipo, CHTLA maybe the only excisional component of TBL surgery (Fig. 3.11).
4.2.1 Case 4.3 High Central Tension Lipoabdominoplasty with VASERlipo of the Back and Upper Thighs and Lipoaugmentation of the Buttocks
Case 4.3: A 50-year-old, 5′4″ tall, 208 lb, woman seeking to rid of bulging body rolls, reduction of hips and thighs, and enlargement of buttocks. She preferred outpatient surgery, and so for safety, the treatment was two staged. For the first stage, she was marked for VASERlipo of the arms, back, lateral chest, flanks, low back, and upper thighs (Fig. 4.11). After the tedious infusion of 4 l of saline with xylocaine and epinephrine, a three-ring VASER in 80 % VASER mode emulsified the fat (Fig. 4.12). 4,500 cc of fatty emulsion was removed with 1,200 cc of filtered fat lipoinjected into the buttocks. At the end of her first post-op week, she started on 6 one-hour treatments of topical ultrasound through VASERshape (Fig. 4.13). Within 2 weeks of her large-volume VASERlipo, she returned to work. Four months later, she was marked for CHTLA with VASERlipo of the epigastrium, lateral abdomen, and medial thighs (Fig. 4.14). 1,200 of aspirated fatty emulsion yielded 600 cc of usable fat for the lower lateral buttocks. Selected images of her operation show critical moments to achieve the central high tension (Figs. 4.15 and 4.16). Four months later (Fig. 4.17), Case 4.3 has achieved the desired torso and upper thigh transformation by combining staged VASERlipo with CHTLA. Lipotransfer from her back, abdomen, and thighs to her buttocks has smoothly reduced her midtorso and enlarged her buttocks to the desired body shape.




Fig. 4.11
Case 4.3 5′ 4″, 208 lb woman desires rid of torso and thigh bulges. (a) Posterior and (b) right lateral views show the purple markings for stage 1 VASERlipo of the excess adipose of the arms, back, waist, and thighs. Green markings on the buttocks are areas for lipoaugmentation

Fig. 4.12
First-stage VASERlipo for Case 4.3. A 2-ring cannula at 70 % power in the VASER mode is being moved through the midline presacral 5 mm incision site. White skin protectors indicate the access sites in this prone only position. The stacked blue VASER console seen between the surgeon and the IV pole includes the infusion system of hanging IV bags with continuous reporting of output; the ultrasonic energy generator with settings and time of usage; and the aspiration machine with rheostat control and hanging collection canisters. 5,500 cc of saline infused. 40 min of energy applications. 4,500 cc of lipoaspirate and 1,200 cc of filter harvested fat for injection

Fig. 4.13
Post-op care for Case 4.3 includes strategic application of VASERshape for multiple one-hour sessions in the medispa

Fig. 4.14
Markings for Case 4.3 second stage, consisting of VASERlipo of the epigastrium and abdomen with CHTLA and lipoaugmentation of the lower lateral buttocks (not seen). Two lines are marked for the superior incision. A conservative line is drawn through the umbilicus. A more aggressive superior line is drawn to eliminate the thinned transverse adherence. After mobilizing the flap, the more superior line was safely incised

Fig. 4.15
Fully suctioned and dissected epigastric flap for Case 4.3. The epigastric flap is held with a central Deaver retractor and lateral towel clamps. VASERlipo removed 1,800 cc from the abdomen. Following direct undermining over the medial superior rectus abdominis muscles, discontinuous undermining of the abdominoplasty flap was performed with opening and closing of the long LaRoe dissector, lying on the lower abdomen. The bloodless, honeycomb appearance of these treated subcutaneous tissues is clearly seen. Stretching and debulking this flap allow it to easily reach a suprapubic transverse abdominoplasty incision
Fig. 4.16
Umbilicoplasty creating high central abdominal tension in Case 4.3. (a) With the abdomen flexed and the released abdominoplasty flap towel clipped to the mons pubis, the site for the circular umbilicoplasty is deepithelialized about 2 cm superior to the isolated umbilical stalk under the flap. Three small deepithelialized dermal flaps at 3, 6, and 9 o’clock position are created by an inverted Y incision. With no removal of underlying adipose, a straight path is bluntly dissected. (b) Through this path, four previous placed sutures with their attached needles are passed with the aid of a clamp. The first is a 3-0 blue Prolene suture from the 12 o’clock position on the umbilical skin sutured to the same position on the abdominal circle. (c) The next three are 2-0 PDS from the fascial base of the umbilicus to their respected 3, 6, and 9 o’clock positions on the deepithelialized small flaps. (d) Tying the 2-0 PDS sutures umbilicates the epigastric flap around the umbilicus. It also tenses the midline of the epigastric flap and relieves some of the tension along the suprapubic closure. The two-layer #2 PDO Quill and 3-0 Monoderm Quill closure is being performed during the umbilical inset. A 4-0 Prolene running baseball closure finely approximates the cutaneous umbilicus to the abdominal flap inset
Fig. 4.17
A satisfied Case 4.3, 4 months after the second stage, weighs 13 lb less than when she started, which is consistent with the weight of fat removed. (a) Anterior view shows that the arms, abdomen, and thighs are smaller and curvaceous. (b) Posterior view shows that the bulging arm, back, chest, and thigh rolls are corrected or markedly diminished. The buttocks are fuller and spherical. (c) Right lateral view shows her flat abdomen, narrow waist, and sharply protruding large buttocks that match the patient’s expectations
The next patient, Case 4.4, is a single-stage TBL that highlights CHTLA and barbed suture suspension mastopexy. The double-armed Quill device submammary suspension of her flatted, previously reduced breasts shows promise as a relatively simple and safe treatment of breast reduction deformity. The entire base of the gland is raised to fill the superior pole and reduce the inferior pole without dissecting Wise pattern skin and breast flaps. The techniques of spiral thighplasty with vertical extension combined with lower body lift and deepithelialized adipose fascial buttock flaps are presented in detail.
4.2.2 Case 4.4 Central High-Tension Lipoabdominoplasty with TBL
A 42-year-old, 5′ 5″, 147 lb, female requests a body lift. Thirteen months after her gastric bypass, she has lost 90 lb. She had a breast reduction 15 years prior. She is unhappy with low, bottomed out breasts and sagging skin of lower body and thighs. Her figure, fully marked for a TBL, is androgynous with a broader upper body and minimal narrowing of the waist (Fig. 4.18). The Pittsburgh grading body contour documentation form is filled out (Table 4.2). Her breasts are broad and flat with Wise pattern scars, empty superior poles, and sagging lower poles. Her full abdomen exhibits moderate skin laxity, a suprapubic hanging pannus, and a transverse umbilical abdominal adherence. Mature striae scatter about the central and lower abdomen. The back and flanks exhibit mild skin laxity and fullness. The flat and wrinkled buttocks slither into the posterior thighs. The anterior thighs are broad from adipose, while the medial thighs are loose and wrinkled.
Fig. 4.18
Case 4.4: With preoperative completed markings in anterior, left anterior oblique, lateral, and posterior views. The abdominoplasty excision lines extend posteriorly into a lower body lift (LBL). The oblique line buttock markings indicate deepithelialization of adipose fascial flaps for buttock augmentation. The plus marks (+, ++, ++++) on her epigastrium, thighs, and left lateral chest indicated the magnitude of fat for UAL. The chest midline has the levels of the desired new IMF and the right and left current IMFs. The high dashed marks indicate the extent of submammary undermining
Table 4.2
The lipoabdominoplasty surgical markings are central to Case 4.4 TBL (Fig. 4.18). All the skin between the umbilicus and pubis is marked for excision, taking care to be superior enough to include the mid-abdominal transverse adherence. The superior incision is continued to the level posterior over the iliac crests to several centimeters above the intergluteal cleft. Plus signs indicate excess adipose of the epigastrium and anterior thighs to be removed through UAL liposuction. Epigastric liposuction discontinuously undermines and deflates the superior abdominoplasty flap with preservation of perforating blood supply to safely increase its excursion towards the suprapubic region. The inferior abdominoplasty incision, obscured by the overhanging pannus, is a horizontal 12 cm line centered over the suprapubic midline and extended towards the anterior superior iliac spines. That line continues across the lateral thigh and over the sagging buttocks, ending at the intergluteal creases. The width between that inferior line and the previously drawn superior line includes all loose skin of the lateral thigh and buttocks. Across the buttocks, the low-lying excision pattern is cross-hatched for deepithelialization for buried buttock adipose fascial flaps for augmentation. The markings for her spiral thighplasty, extended by a full-length medial thigh vertical excisions and picture frame pubic monsplasty, are obscured by overlapping skin. Finally, the breasts were marked with an IMF incision for the superior internal suture advancement for a Quill suspension mastopexy. Her midtorso is long enough that the downward force of the abdominoplasty closure will not prohibit the upward force of suspending her breasts. The sternal midline has three lower marks indicating the left IMF, the right IMF, and the most superior the new IMF for both breasts. The superior chest dashed crescent line indicates the extent of superior undermining between the breast and pectoralis muscle for suture suspension.
The operation starts prone with the legs widely abducted on arm boards attached to the lower end of the operating room table (Fig. 4.19a). There is an operating surgeon on each side of the table. The foot of the table is dropped for an assistant. The left adipose fascial flap, labeled with (1), is marked for deepithelialization. The dashed line would be the inferior incision, but that is raised several centimeters to compensate for the added area needed to cover the buried flap. The left buttock island flap (1) is mobilized and advanced under the buttock skin flap to nearly the ischial tuberosity (Fig. 4.19b). A view from the head of the table shows that both buttock flaps (1, 2) are positioned under the gluteal flap (Fig. 4.19c). Upon preliminary closure of the buttock excision site over the buried flaps, the pleasing rounded fullness is clear (Fig. 4.19d). The medial vertical extension (3) of the thighplasty is depressed following thorough excision site liposuction.
Fig. 4.19
Case 4.4 starts prone with the LBL and buttock augmentation. (a) Oblique view with legs extended on arm boards. 1 is the left adipose fascial flap. 2 is the right adipose fascial flap. 3 is the vertical thighplasty excision. (b) To the right of the image, Deavers retract the buttock skin flap for inferior positioning of the left flap (1). (c) From the head of the table, the left flap (1) has been sutured in place, and the right flap (2) is being positioned. (d) The LBL closure has started to show the rounded contour of the buttock augmentation. The drop down of the foot of the operating room table facilitates a second team excising the skin between the buttocks and the posterior thighs for the start of the spiral thighplasty. The vertical excision site (3) has been radically defatted of fat through UAL
The start of the spiral thighplasty between the buttocks and posterior thigh is performed during closure of the LBL (Fig. 4.20a). The ischial tuberosity is palpated but not exposed. Three interrupted #1 braided Vicryl sutures advance the left posterior thigh subcutaneous fascia to the ischial periosteum (Fig. 4.20b). The left leg is adducted. After tying the left side sutures, a depression of the leading edge of the posterior thigh is seen; this will demarcate the gluteal thigh fold and tighten the posterior thigh (Fig. 4.20c). Then the interrupted sutures of the right side are placed and tied. The foot of the table is raised allowing both legs adducted on the operating room table (Fig. 4.20d). The contour improvement and well-placed closures are seen at the completion of the prone portion of the TBL.
Fig. 4.20
Case 4.4: Start of the spiral thighplasty. (a) The premarked elliptical excision of excess skin between the lower buttocks and thighs has been made to nearly to gluteal muscular fascia and fascia lata of the posterior thigh. The ischial tuberosities are palpated, but not exposed. (b) #1 absorbable braided suture is placed to advance the posterior thigh to the ischial tuberosity. (c) The left deep sutures that define the buttock thigh fold have been tied, as the right sutures are about to be tied to advance the posterior thigh to a more superior level. (d) Improve contours of the low back, hips, buttocks, and posterior thighs upon completion the operation in the prone position with closures symmetrical and in proper position. The posterior incision of the vertical thighplasty was made and then temporarily stapled closed
Case 4.4 is rolled over to a gurney and then slide back onto the operating room table. She is supine and frog legged (Fig. 4.21a). The medial thigh depressions indicate the fat emptied excision sites. UAL needs to be completed over the anterior thighs and epigastrium. The abdominoplasty is performed at the same time as excision of the vertical extensions of the medial thighs. Due to its tension on the upper thigh, abdominoplasty closure is started before excision of the upper horizontal medial thigh. From distal to proximal, the medial thigh skin is avulsed with scalpel cuts off the defatted subcutaneous tissue (Fig. 4.21b). The underlying neurovasculature is seen preserved. The wound edges are approximated with towel clips (Fig. 4.21c). If the closure is loose, then additional skin is excised along one of the wound edges. The two-layer closure is with #1 PDO Quill subcutaneous followed by 3-0 intradermal Monoderm (Fig. 4.21d).
Fig. 4.21
Case 4.4: Start of TBL in supine position. (a) Frog legged to facilitate the thighplasty and reduce closure tension on the abdominoplasty. The left excision site is depressed from the UAL. (b) At the left, a facelift rake pulls up the skin being cut/avulsed from the retained neurovasculature, after radical liposuction defatting. (c) Towel clamp approximation checks the adequacy of resection. (d) The two-layer vertical suture line is nearly closed. The horizontal portion of the thighplasty will not be closed until the abdominoplasty closure
Coincidental with the vertical thighplasty, a second team starts the abdominoplasty with the UAL of the epigastrium followed by the transverse superior incision (Fig. 4.22a). The central vertical adherence is sharply dissected from the linea alba and medial rectus sheaths (Fig. 4.22b). Electrosurgical dissection continues a 6–7 cm wide tract to the xiphoid (Fig. 4.22c). Lateral mobilization of the superior flap is performed by inserting and spreading a LaRoe dissecting forceps (Fig. 4.22d). Most perforating vessels to the abdominoplasty flap are preserved by this discontinuous undermining.
Fig. 4.22
Case 4.4: Central high-tension lipoabdominoplasty (CHTLA) starts simultaneous with the vertical thighplasty. (a) After UAL of the epigastrium, an incision is made through the umbilicus and superior to the transverse adherence. (b) After circumscribing the umbilicus, dissection is directly over the epigastric rectus fascia midline. (c) Elevation of the flap continues to the xiphoid. (d) Indirect undermining by spreading of the LaRoe dissector preserves most perforating vessels for the abdominoplasty flap
The abdominal flap is pulled down towards the pubis, and the exact line of inferior incision is confirmed. The incision is made with preservation of Scarpa’s fascia over the groins. The composite lower abdominal excision leaves behind the supramuscular fascia areolar tissue and fat except along the rectus midline (Fig. 4.23a). For 6 cm or so, Scarpa’s fascia is preserved over the groins. It can be grasped and held up (Fig. 4.23b). Diastasis of the midline rectus is approximated with the placement of horizontal #2 PDO Quill (Fig. 4.23c). The ends of the suture are pulled to close the midline (Fig. 4.23d). A complete row of horizontal passes is reinforced with simple over and over throws.
Fig. 4.23
Case 4.4: Lower portion of the abdominoplasty. (a) The inferior incision has been made as marked with preservation of Scarpa’s fascia over the groins. Sub-Scarpa’s fat and areolar tissue is preserved laterally. Along the midline, the rectus fascia is exposed. (b) Preserved Scarpa’s fascia over the groin and lower abdomen is grasped and raised. The open wound of the upper thigh will not be closed until after the abdominoplasty. (c) The medial edges of the rectus muscles have been drawn with a surgical marker. Along that line, four horizontal mattress throws of #2 PDO Quill are placed. (d) The ends of the suture are pulled to cinch close the diastasis recti
The umbilicoplasty participates in achieving central high closure. The circular new umbilical site is marked on the approximated abdominoplasty flap along the midline several centimeters superior to the native umbilicus. The epigastric flap will be buttonholed to the rectus fascia base of the umbilicus and sutured there through the tips of deepithelialized flaps. A single simple pass of a 3-0 Prolene suture is made at the 12 0’clock position. Horizontal mattress sutures of 2-0 PDS are placed at 3, 6, and 9 o’clock fascial base of the umbilicus and held with clamps (Fig. 4.24a). When the umbilical stalk is longer than the thickness of the umbilicoplasty site of the abdominoplasty flap, it is reduced. The previously place fascial sutures are sutured about two-thirds the way up the stalk (Fig. 4.24b). As the third detelescoping suture is tied, the umbilical stalk is shortened (Fig. 4.24c). The sutures are kept long and will be passed through a deepithelialized umbilical opening. Either a shield or round opening is made through the abdominoplasty flap several centimeters superior to the location of the current umbilical cord (Fig. 4.24d). The diameter of this opening is two-thirds the thickness of the abdominal wall. After deepithelialization, the three small flaps at 3, 6, and 9 o’clock positions are incised (Fig. 4.25a). Without removing fat, the passageway for the umbilicus is made with blunt and sharp dissection. With a clamp and helping hand, the PDS sutures at the base of the umbilicus are passed through the umbilical opening (Fig. 4.25b). The 3-0 Prolene suture orients and approximates the umbilicus to the opening. The three PDS sutures are aligned in their proper position on the abdomen. Each suture is placed through a horizontal bite at the tips of their respective deepithelialized flap so that the knots will be buried (Fig. 4.25c). Tying these sutures drags each deepithelialized flap to the rectus fascia, to impart an umbilical appearance to the central abdominal wall (Fig. 4.25d). The inferior drag places a depressed tension line towards the xiphoid and relieves some tension at the lower central abdomen. The tension reduction improves circulation of the most ischemic portion of the flap and allows for a slight rounded lower abdominal fullness. A 4-0 Prolene simple running suture closes the umbilicus to the umbilical opening. Meanwhile, horizontal portion of the medial thighplasty is completed. It is extended to the mons pubis for a properly sculptured monsplasty. Several large braided sutures approximate the upper medial thigh flap to the pubic Colle’s fascia. Then the upper thigh wound is closed with 0 PDO Quill and 3-0 Monoderm.
Fig. 4.24
Case 4.4: Umbilicoplasty with CHTLA. (a) 2-0 PDS sutures are passed through the inked dots at 3, 6, and 9 o’clock positions in the rectus fascia around the base of the umbilicus. A 3-0 Prolene is placed through the 12 o’clock position. All these long sutures will be pulled through an opening in the abdominoplasty flap made for the umbilicoplasty. (b) The long umbilical stalk is reduced in half by passing through it each of the PDS sutures. (c) Tying the three PDS sutures shortens the umbilicus. (d) With the abdominoplasty flap pulled down, the site of the umbilicus is marked, and then a circle or shield 2 cm superior is deepithelialized. An inverted Y is drawn for isolating three small flaps that will be sewn down to rectus fascia
Fig. 4.25
Case 4.4: Completing the umbilicoplasty. (a) Three small deepithelialized flaps for the umbilicus opening are incised. (b) Three 2-0 PDS sutures surrounding the umbilicus are individually drawn through the opening for the umbilicus. (c) These three PDS sutures lie at across the opening in the abdominal flap at 3, 6, and 9 o’clock. (d) An encircling suture of 4-0 Prolene is being started between the umbilicus and the umbilicated opening in the abdominal wall. With the abdominoplasty being closed, the excision and closure of the horizontal monsplasty are done
After 4 h of lower body and thigh team surgery, she lost about 400 cc of blood. Her vital signs were normal, including temperature. Her upper body forced hot air blanket is transferred to her completed lower body for starting the suture suspension mastopexy. The inframammary scar is incised and submammary dissection carried to the second rib (Fig. 4.26a). A double-armed #2 Prolene barbed suture is used for parenchymal suspension. Since the intramuscular bites can lead to prolonged pain, more recently absorbable #2 PDO suture is used. A single bite is taken through the pectoralis muscle onto the second rib (Fig. 4.26b). Large vertical bites with each needle were taken through the breast parenchyma (Fig. 4.26c). While pulling inferiorly, the upper breast was synched into a dome (Fig. 4.26d). The sutures are then passed through the pectoralis tissue at the desired raised IMF. The suturing continues through the lower chest flap to suspend it to the raised fold. Her appearance on the operating room table is seen at the end of the operation (Fig. 4.27). The breasts project better, with symmetrical and higher IMFs. The body and thigh contour are excellent. Ten days after her TBL and just prior to her leaving Pittsburgh, she is healing well with improved feminine contours (Fig. 4.28).
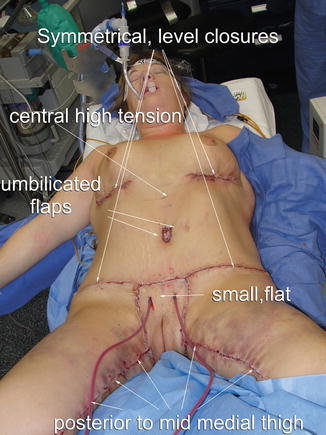
Fig. 4.26
Case 4.4: Quill suture suspension mastopexy to reposition parenchyma. (a) The IMF incision is made with retention of adipose to breast parenchyma. A Quill, double-armed clear #2 Prolene suture for suspension lies on the right breast after a complete submammary dissection. (b) With the breast retracted, the #2 Prolene suture is placed through the muscle and along the second rib. (c) Each limb of the bidirectional-barbed suture is stitched securely through the breast parenchyma. After two breast bites, the pectoralis muscle is sutured one more time. (d) Upon completion of the suspension, greater gland roundness and projection are seen. The previously protruding lower pole fat has been retracted superiorly. The Quill suture will be continue inferiorly to raise the IMF and lower chest skin
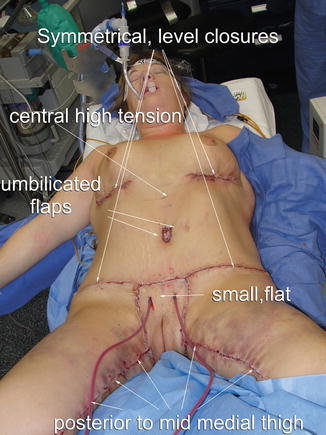
Fig. 4.27
Case 4.4 shows improved contours and symmetry at the end of the procedure
Fig. 4.28
Case 4.4: Result of TBL at 10 days. The Quill suture suspension has evenly redistributed the breast parenchyma over the upper and lower poles. The waist is narrower and the hips and buttocks fuller with a defined infragluteal fold. The thighs are smoothly cylindrical with a nearly hidden vertical scar
Case 4.4 sent a letter to the office soon after flying home. Her profound expression of gratitude is the only patient testimonial published in this book:
Dear Dr. Hurwitz,
There was so little time to be able to say all that I wanted to. We arrived home safely (after 10 hours in the airport!!). I had a lot of time to think about the last 10 days of my life. It has been an amazing journey from start to finish. I knew I had the right Dr. When I came in to see you last September…and you know when you know! Many people asked me before I left why on earth would I go all the way to PA to have this done and I always told them that I wanted the best and I wasn’t settling for anything less than that. They would ask me..“how do you know he’s the best?” and I would tell them “because I did my homework…and I just know.” Now I have the proof to show them.
…if you are an out of town patient, it is good to know that the ‘total’ experience is a successful one. But, in order to have that piece be successful, I believe that it has to start in the operating room. I wish I had more time to focus on you and your work during my appointment because, certainly, that was the best part of the experience. I was confident in you from the first moment I met you in September and that confidence never wavered.
It was tough getting to this point financially, but we were determined that if there was a way to make it happen, we would. I don’t believe you can put a monetary value on what you did for me and what you’ve done for others. It is worth every penny and then some. You cannot put a price tag on self-esteem, confidence and security. Not that these things are all found in the way you look… because i don’t believe they are…but it certainly contributes.
As I look at the days ahead, I am excited. I am walking forward in renewed confidence of who I am. And that, Dr. Hurwitz, has so much to do with you. I am grateful for the team you had assembled to do this huge work and I wish I could thank every one of them in person…I know you trust them and they may have had the same results with or without you..BUT… It was me KNOWING you were heading up that team that helped me to walk through it peacefully and successfully.
I could go on forever I am sure. I just wanted to say thank you once again. I hope to be a walking advertisement for you and that some of the people that I cross paths with, will seek you out for their surgeries. If you have any patients that would like to talk to someone..personally… who has already walked this road, please don’t hesitate to give them my contact information. I would consider it an honor. I pray that you are blessed as I have been blessed.
Case 4.4 sent follow-up views 4 years after her TBL (Fig. 4.29). The feminine contours have persisted, and the scars are well positioned and faint. The lower poles of the breast are not quit as full, but the IMFs have not dropped.
Fig. 4.29
Case 4.4: Result of TBL 4 years later. Out of town patient sent in photos demonstrating maintenance of feminine contours and faint scars. The left lateral view best shows favorable breast and buttock shape. She and her husband consider her sexy
At times an abdominoplasty has already been done, and so the lower body lift is combined with the spiral thighplasty with a vertical extension.
4.3 Lower Body Lift Combined with Spiral Thighplasty
The hemi-circumferential excision of lower back and hip skin followed by superior advancement of the lower suture line defines a lower body lift (LBL). LBL is routinely combined with an abdominoplasty and thighplasty. A thighplasty is excision of excess skin followed by tightening and suspension through wound closure.
4.3.1 Case 4.5 Severe Skin Laxity for LBL, Spiral Thighplasty
Case 4.5 is a 42-year-old, 5 foot, 115 lb, female, requesting body-contouring surgery (Fig. 4.30). Ten years earlier, at 300 lb she had gastric bypass surgery, followed by an abdominoplasty and hernia repair. One year later, she delivered her fifth child. She had bilateral brachioplasty 1 month prior to her initial consultation with the author. She was referred for correction of sagging thighs, buttocks, and breasts. Her left breast fills a B cup brassiere and her right breast slightly smaller. She has occasional lower leg edema that responds to diuretics. Arthritis of her back and knees are being treated with anti-inflammatory medications and Vicodin. In 2010, a right breast carcinoma was treated by lumpectomy, chemotherapy, and radiation. Mammogram in July 2012 was negative. Her thin upper body reveals rib contours. The breasts are asymmetrical and flat with grade II ptosis. Her narrow waist leads to flared hips. The buttocks are wrinkled, sagging, and flat with lateral depressions and no inferior gluteal fold. Her saddlebags are wrinkled. The thighs have bellowing skin redundancy with severe cellulite. The most severe skin laxity is along the mid-medial and upper lateral thighs. Her prior abdominoplasty has tightened the skin and rounded her mons pubis. The plan is a two-stage TBL to remove skin laxity of the thighs and create rounder and fuller buttocks, lateral thighs, and breasts. Stage 1 is a LBL with adipose fascial flap augmentation of the buttocks and a spiral thighplasty with a medial vertical extension. The oversized saddlebags will be advanced over a radically excised upper lateral thigh, imparting a taper to the thigh. The spiral of spiral thighplasty refers to the spiral course of the excision from the groin, through thigh-labial junction to across the infragluteal fold to the lateral thigh. As there was no neighboring soft tissue for augmentation, stage 2 is bilateral saline-filled sub-pectoralis muscle implant breast augmentation with Wise pattern mastopexy under local anesthesia. A limited budget precludes gel implants or even general anesthesia during the second stage.
Fig. 4.30
Case 4.5, after a 125 weight loss, abdominoplasty, and then brachioplasty elsewhere, presents for further body-contouring surgery. Upper torso is thin with minimal skin laxity and small ptotic breasts. The thighs have bellowing skin redundancy, sagging deposits of fat, and cellulite. The buttocks are flat, wrinkled, and ptotic
The preoperative markings for stage 1 are dictated by the skin laxity and goals for aesthetic curves (Sect. 3.2.1). Her smaller, slender upper body would be treated by an augmentation mastopexy at a second stage. Maintaining broad rounded upper lateral thighs was possible through a full-thickness lateral body excision that would include the lateral saddlebag depressions and suspend the relatively full lateral thighs. The frontal and right-side views show that considerable skin and underlying fat were marked for removal from the medial thighs and continuing across the groins to the hips (Fig. 4.31). The drawn lines are numbered in sequence. The initial line is a midline vertical (1) from umbilicus to labia majora commissure. From the prior abdominoplasty, there is no skin excess to be excised along the lower abdominal midline. That midline facilitates symmetry. Six centimeters from either side of the midline, a vertical line (2) is drawn down the lateral mons pubis and along the junction between labia majora and medial thigh. As part of the spiral thighplasty, that line continues to the ischial tuberosity and then along the gluteal fold when the patient is turned. With the right hip and knee flexed, the medial thigh skin falls to the mons pubis. The excess skin is marked, and through this mark, the inferior line (3) of the upper thigh crescent excision is drawn. With the right leg slightly abducted and the anterior thigh skin dragged medially, a vertical line (4) along the medial meridian is drawn to the medial knee. From that line in the middle of the thigh, a pinched test leads to marking the width of resection of the vertical excision. A long tapered posterior line (5) completes the medial vertical ellipse. The horizontal incision lines (2, 3) of the medial thighplasty taper almost together as they cross the groins on the way to the anterior superior iliac spines (ASIS). From there, superior anchor lines (6) are drawn straight across the hip and back to meet several centimeters superior to the gluteal cleft. This horizontal anchor line (6) holds the suspension from the advanced inferior flaps. Along the lateral thigh, the excess skin is pinched to the superior line with the widest point being at the saddlebag deformity. The inferior incision line (7) descends to that point through grasping that the lateral thigh no longer sags. Then the inferior line (7) proceeds across the buttocks to the top of the intergluteal cleft. Most of the posterior portion of the LBL excision is deepithelialized and stacked for buttock augmentation. The overhanging inferior buttocks obscure most of the planned excision at the buttock thigh junction.
Fig. 4.31
Frontal and right-side views of Case 4.5 show the preoperative markings for the LBL and spiral thighplasty with a vertical medial extension. The numbers indicate the sequence of line placement. The buttock segment of the LBL will be deepithelialized for adipose flap augmentation
Case 4.5 operation starts supine with legs abducted 45° on articulating arms boards (Fig. 4.32). Two operators work simultaneously on the symmetrical markings (Sect. 3.2.2). The primary surgeon excises along the left upper thigh, groin, and hip, while the assistant thoroughly performs opposite (right) medial thigh radical excision site liposuction (Fig. 4.32, upper). The LySonix long golf tee probe is over the right medial thigh skin, while a scalpel is poised for incision over the groin. Later, the teams switch sides. The surgeon excises premarked oblique strip of skin and superficial fat from upper anterior thigh bordering the labia majora, across the groin and over the crest of the pelvis. The deep subcutaneous fascia is the depth of resection until passing the anterior superior iliac spine (ASIS). Over the groin, Scarpa’s fascia is preserved to protect underlying lymphatics to mons pubis, lower abdomen, and anterior thigh, thereby reducing swelling and seromas. To reduce the oversized hips, the entire thickness of skin and fat is excised to the muscular fascia within the upper pelvis. Limited discontinuous lateral thigh undermining is performed with LaRoe dissectors (Fig. 4.32, lower). The isolated longitudinal depression of right medial thigh skin indicates radical excision site aspiration fat (Sect. 3.2.8).
Fig. 4.32
Operation for Case 4.5 starts supine. (Upper) The operator incises skin and fat from the left groin as an assistant holds a gulf tipped LySonix cannula over the right-side excision site. (Lower) The depressed right thigh excision site indicates completion of radical excision site liposuction. UAL of the right thigh is starting. There was full-thickness skin and fat resection of the left lateral thigh and partial thickness fat removal from the lower abdomen and groin. A LaRoe dissector (ASSI) is partially inserted over the fascia lata of the thigh and is opening for discontinuous undermining
With the leg abducted, the deep closure of the right hip wound is started by placing four throws of #2 PDO Quill (Fig. 4.33, upper) followed by pulling both ends to slowly approximate the wound edges (Fig. 4.33, lower) (Sect. 3.2.9). Each end of the suture will be continued across the groin and towards the posterior midline. Across to the opposite thigh, the skin excision over the medial thigh excision site liposuction (ESL) is essentially a full-thickness skin graft. Very little adipose remains on the medial thigh. In the middle of the thigh, four horizontal throws of #1 PDO Quill have been placed across the wound (Fig. 4.34 upper). Pulling the ends of the PDO suture approximates the closure (Fig. 4.34 lower). A towel clamp secures the proximal suture line as closure continues distally. The medial and anterior thigh closures are performed simultaneously in two layers with running horizontal subcutaneous #1PDO and intradermal 3-0 Monoderm Quill (Sect. 3.2.9). The tissues are stretched into optimal contours with symmetrical lines of closure (Fig. 4.35). The vertical thigh extension closures are several centimeters posterior to medial thigh midline. Prior to turning the patient prone, the legs are abducted. Open wounds are left at the lateral hip and ischial tuberosities.

Fig. 4.33
Case 4.5: Left hip closure. (Upper) Four deep throws of #2 PDO Quill start the deep closure of the left hip wound. (Lower) With the thigh abducted on an arm board, wound edges are approximated by pulling both ends
Fig. 4.34
Case 4.5: PDO Quill closure. (Upper) Two horizontal bites are taken on either side of the initial stitch. There is a fine latticework of retained neurovasculature and connective tissue along the right medial thigh excision site. (Lower) The wound is close by pulling on the sutures

Fig. 4.35
Case 4.5: Skin glue is applied to the two later closures at the completion of the operation in the supine position with the legs abducted. Open wounds remain at hips and posterior medial thighs
When the patient is turned prone, the buttocks are mushroomed. At 32 thousandths of an inch thickness, an electric dermatome removes epithelium to mid-dermis over the adipose fascial buttock flaps (Fig. 4.36a). The precise method of flap mobilization to fill the gluteal pockets by advancement, rotation, purse-string tightening, and/or overlap is determined. These low-lying flaps are circumferentially undermined several centimeters for adequate mobilization (Fig. 4.36b). A supragluteal space is elevated to accept the flaps (Fig. 4.36c). After the superior two-thirds of the buttocks are undermined over the gluteal fascia, the lateral portion of the right flap is flipped over to be suture advanced into the medial-inferior extent of the pocket (Fig. 4.37d). Matching flap augmentation is performed on the left side. Two or three large absorbable sutures advance the flaps in their buried location. The LBL incisions are closed with running #2 PDO Quill closure, followed by 2-0 intradermal Monoderm (Sect. 3.2.9). The final maneuver is excision of the elliptical excess between the inferior buttocks and posterior thigh, followed by suture suspension of the medial posterior thigh to the periosteum of the ischial tuberosity (Fig. 4.37). This termination of the spiral thighplasty tightens the posterior thigh, establishes a medial infragluteal crease, and supports the lower buttocks. Prior to excision of the marked left inferior gluteal thigh excess, the right-side excision and posterior thigh lift have been completed and the thigh adducted (Fig. 4.37 upper). The left posterior thigh fascia was advanced to the periosteum of the ischial tuberosity with large braided absorbable sutures followed by a two-layer Quill closure (Fig. 4.37, lower). Both thighs are seen adducted. The inferior buttock fold is well defined. The buttocks have exaggerated rounded projection. Two large JP drains exit at hips. Drains are used with buried flap LBL and neighboring liposuction. There needs to be immediate adherence of the deepithelialized flaps to the overlying buttock flap.
Fig. 4.36
Case 4.5: LBL with auto-augmentation of the buttocks. (Upper left) With the patient turned prone, the donor site adipose fascial flaps are deepithelialized with an electric dermatome. (Upper right) Deepithelialized flaps are isolated on subcutaneous islands. (Lower left) Right supragluteal pocket is exposed to receive flaps. (Lower right) The adipose fascial flap is turned into the supragluteal pocket for augmentation
Fig. 4.37
Case 4.5: Posterior portion of the spiral thighplasty. (Upper) With closure of the low back wound, bilateral adipose fascial flap augmentation of the buttocks and LBL have been completed. An ellipse of skin and fat is drawn to be removed from the left buttock thigh junction, while the thighs are still abducted. (Lower) The legs are now adducted, tightening the lateral thigh closures. Skin glue has been applied to all closures. Two 10 mm. JP drains exit at hips
The initial positioning for the LBL in Case 4.5 is supine and for the earlier Case 4.4 is prone. Several years ago, a fundamental change was made in the operative sequence of lower body-contouring surgery. Instead of starting prone, this operation may begin supine and end prone (Sect. 3.2.2). In that way lower body lift closure over the spine early in the operation is not compressed on the operating room table. Often those hours of motionless pressure during the abdominoplasty led to fat necrosis and delayed wound breakdown over the sacrum. With the change in position order, there were no presacral healing problems in the last 8 patients. She was discharged 2 days later and healing was uneventful. Five months later, her TBL was competed with Wise pattern mastopexy and subpectoral 250 cc. saline implant augmentation. The anticipated result of her TBL is realized 2 years later (Fig. 4.38). Her bikini pattern sun tan and new found intimacy are reflections of her satisfaction with her results. However, the final result was achieved through a revision. Six months prior, she was successfully treated for recurrent saddlebag deformity and lateral gluteal depressions with VASER liposculpture (Sect. 3.2.6).
Fig. 4.38
Case 4.5: Frontal and right-side views 18 months after her lower body and thigh surgery, 12 months after her saline implant augmentation and mastopexy, and 6 months after VASERlipo and augmentation of lateral gluteal and thighs as shown in Fig. 3.12. Her bikini tan lines reflect her comfort with her new body shape
The same set of operations are performed in a woman with moderate lower body and thigh skin laxity.
4.3.2 Case 4.6 LBL and Spiral Thighplasty with Minimal Skin Laxity
Case 4.6 is a 5′ 5″, 143 lb, 34-year-old woman who wants to correct body changes due to her two pregnancies and mild fluctuations in body weight (Fig. 4.39). In 2008 she underwent an abdominoplasty and bilateral 300 cc gel implant breast augmentation with periareolar mastopexy. She returns in 2013 to complete her TBL by correcting her sagging buttocks and thighs, which are shown with preoperative markings for a LBL, spiral thighplasty, and a limited medial vertical extension to the mid-thigh (Fig. 4.39). Her lateral hips are not only flat but depressed inferior to the iliac crests. The buttocks are broad and sagging with considerable cellulite and poor definition at the posterior thigh junction. The upper medial thighs are so full that they touch; however, there is no laxity along the distal half of the medial thighs. For skin laxity that extends beyond the upper third of the medial thigh but not down to the knees, a limited vertical extension to the spiral thighplasty is drawn half way down the thigh with care to keep the closure unseen in frontal view (Fig. 4.39). The upper crescent-shaped horizontal excision with the assistance of an anchor stitch in Colle’s fascia pulls up the vertical thigh closure several centimeters. The vertical extension angles posterior and ends at mid-thigh for less visibility. A tight closure of the vertical extension supports the horizontal position to minimize the chance for inferior drift of the superior scar or distraction of the labia majora. This shortened vertical scar extension is accepted by most scar phobic patients, as this operation is more effective and more stable than the horizontal excision alone. The terminal extent of the spiral thighplasty extends slightly beyond the infragluteal fold for a smooth contour transition to the lateral thigh. Posterior thigh suture suspension to the ischial tuberosity is essential for tightening the thigh and supporting the inferior buttocks with a medial defined fold. To correct her lateral gluteal depressions, the lateral excisions of the LBL remove skin only, and the lateral thigh flap is advanced over all retained lateral fat.
Fig. 4.39
Case 4.6: Preoperative markings for LBL with spiral thighplasty with limited vertical extension for mild deformity after a healed abdominoplasty. (a) There is concavity along the hips and skin laxity of the medial thighs. (b) The hip concavity is impressive. The vertical medial thigh excision extension stops 60 % down the thigh. (c, d) Symmetrical LBL excisions and crescent between the buttocks and posterior thighs
The early spiral thighplasty anterior/medial scars are seen wrapping around the groins, along the labia thigh junction and terminating in the buttock thigh fold. The vertical thighplasty scar lies at right angles to the thigh/labia majora scar and posterior to the medial meridian of the thigh. The loose skin has been corrected and the anticipated contours achieved. Note the excellent definition between the rounded inferior buttocks and the posterior thigh. At 12 months (Fig. 4.40), she has maintained her result and has left Pittsburgh for the Gulf Coast beaches.
Fig. 4.40
Case 4.6 One year postoperative views after LBL with a spiral thighplasty with a medial extension. (a) Frontal view shows symmetrical scars across the groins that course along the labial thigh groove. The medial thigh scars are not seen. (b) Slight convexity across the hips under the healed hip closure. (c, d) Symmetrical buttock convexity with well-defined medial fold
Case 4.6 underwent nearly the same operations as Case 4.5. Since Case 4.6 deformities were less, the procedures were less extensive. There was less width of skin resection, less weight on the thighs, and no buried adipose fascial flaps in the buttocks, and the medial vertical extensions were shorter. The buttock thigh junction was nonexistent in Case 4.5, so the excision was extended almost to the lateral thighs. As Case 4.6 anchor line did not drift inferiorly, there was no recurrence of the saddlebags or depression under the LBL lateral scar as in Case 4.5.
These cases demonstrate when a prior proper abdominoplasty adequately shapes the mons, the transition of the LBL to the thighs courses obliquely across the groins to the medial thighs. When the mons needs flattening, the excision runs vertical along the lateral aspects of the mons pubis. There is a continuum of skin laxity and distorted contours of the lower body and thighs. As such, the lower body and thighs are comprehended as a unit, because the operations to treat them are so intertwined. Since skin laxity and contour deformity are not isolated to a single region, correction of one area leaves a contiguous one unchanged, disrupting aesthetic harmony. The same harmonious approach is practiced for the treatment of facial aging, with the caveat that body-contouring surgery is performed on a much larger scale. With the assistance of an experienced team, the author has efficiently performed this combination of operations in healthy, nonobese, well-prepared patients with anticipated results and minimal morbidity. Throughout these operations, excess fat is aesthetically reduced through liposuction and thoroughly removed along the medial thigh excision site. The considerable magnitude of surgical trauma and high-tension closure of subcutaneous tissues is frequently complicated by small areas of delayed wound healing. As such, the optimal candidate is young, healthy, well nourished, and normal weight. These combinations are not indicated in the obese and when extensive liposuction is anticipated. There is simply too much tissue weight against the closure or too much swelling or tissue injury due to liposuction.
The defining artistry of comprehensive body-contouring surgery is the transition from one body area into another. The component operations seamlessly flow enhancing gender-specific contours. For the combination of the LBL, abdominoplasty and vertical thighplasty, the transverse limb of the thighplasty is the transition procedure. The spiral thighplasty interconnected the body and thighs. It is a twisting excision and closure that starts at the infragluteal fold, winds around the uppermost medial thigh, and then ascends to the groin. Similarly for the chest, back, breast, and arms, the short limb of the L-brachioplasty transitions arm reshaping with the upper body lift.
Many plastic surgeons avoid combining these operations either to limit the magnitude of surgical trauma or to avoid possible competing vectors. They feel the results are compromised when all the operations are combined. They also feel this complex surgery is too often followed by some recurrent thigh laxity and too many areas of delayed wound healing. This author’s analysis and practice have been contrary. The vector forces at closure are complimentary, not competing (Hurwitz et al. 2006). Posteriorly the buttocks and lateral thighs are vertically suture suspended to the back and hips, whereas the posterior thighs are vertically suspended to the ischial tuberosity. Anteriorly the groins and upper anterior thighs are vertically suture anchored to the upper abdominal skin and Colle’s fascia. A vertical medial thighplasty has a noncompetitive transverse vector force along its anterior to posterior thigh skin closure.
The aesthetic success of this set of operations depends on the preoperative planning which leaves the patients with marks indicating lines of excision, depths of resection, magnitudes of liposuction, and possible flap donor and recipient sites. Precise planning maximizes operative efficiency and the impact of each of the separate operations and integrates them into a continuum of body shaping. Preoperative marking is performed in a variety of patient positions taking advantage of presentation while upright and under varying effects of gravity. Preoperative markings allow for visualization and estimation of adipose thickness, whether it is appropriate, excess, or deficient. Excess tissue is pushed and pinched and otherwise gathered at key locations when determining the width and direction of resection.
Case 4.7 is a video presentation of lower body-contouring from drawing through surgery in a 60-year-old woman with severe skin laxity after MWL.
4.3.3 Case 4.7 with Severe Skin Laxity in Older Patient
Case 4.7 combines FDL, LBL, and spiral thighplasty with vertical medial extension (Figs. 4.41 and 4.42). Video 4.2 summarizes the markings and Video 4.3 the operation. Through dieting and exercise, this 60-year-old woman lost 52 lb. She desires removal of lax abdominal and thigh skin with narrowing of her waist and retaining full hips for a more feminine figure. She has diffusely sagging skin of the abdomen and buttocks and contour irregularities with wrinkled loose skin of the thighs. Her abdomen has asymmetrical transverse and vertical skin laxity with vertical and right subcostal scars. An inverted T-shaped abdominoplasty would include most of her abdominal scars and reduce the midtorso transverse laxity. A centrally positioned LBL will treat her diffusely lax lateral lower torso and thigh. A complete spiral thighplasty defines the lower buttock thigh junction and tightens the upper posterior thigh. A vertical extension medial thighplasty will extend to the knee to tighten the lower two-thirds of the thighs, accepting that the suprapatella region will have some remaining loose skin folds.
Figs. 4.41 and 4.42
Case 4.7: Preoperative markings for LBL and spiral thighplasty for a 5′ 5″, 143 lb, 60-year-old mother. The numbers are explained in the text. Her waist is partially obliterated by adipose bulging superior to the iliac crests. Her buttocks are flat and sagging and have cellulite. The LBL excision lines encompass the undesirable contour depression, leaving a high anchor line over the iliac crests. Oblique extensions spiral across the groins, around the medial thighs to end across the inferior buttock posterior thigh junction
The presurgical markings are captured on video with the completed set shown in Figs. 4.41 and 4.42. Usually the first set of markings is made standing, but in her case, she laid supine and reclined. Her abdominal midline (1) is drawn to the xiphoid to the commissure of the labia majora. Her umbilicus lies slightly to the right. About 6 cm superior to the labia majora commissure, a 12 cm horizontal line (2) is centered. This horizontal is continued (3) across the groins to the anterior superior iliac crest. After turning right-side lateral decubitus, the right leg is raised until the knee is higher than the hip, thereby abducting the thigh about 45°. The loose lateral thigh skin descends by gravity towards the hip. While in the abducted position, the lower incision (4) of the abdominoplasty is continued across to the lateral thigh to the intergluteal crease. The width of midlateral skin excision (5) is determined by forcibly gathering the hip upper thigh skin. In the left lateral decubitus position, the markings are repeated on the left side. The marking for the vertical portion of the Fleur de Lys abdominoplasty in this patient is made supine, although more commonly it is done standing. The approximate width of middle of the vertical resection is determined by gathering and folding epigastric skin equally across the midline. After those lines (6) are made, vertical lines (7) taper to the xiphoid and descend (8) several centimeters past the encircled (9) umbilicus. Point 8 can be gathered to the midline at the mons pubis. From point 8, transverse lines (10) arch across to previously marked upper incision line (5) of the LBL, thereby delineating the transverse width of the abdominoplasty excision.
The monsplasty and upper medial thighplasty lines interrelate (Figs. 4.3–4.8). While frog legged, about 5 cm from either side of the midline, verticals (11) are dropped across the mons to the labia majora/thigh groove at the level of the labial commissure and continued in that groove until sweeping slightly laterally to the ischial tuberosity. When the thigh is flexed and adducted, excess medial skin falls and is massaged to the pubis to mark the widest point of the width of anterior transverse thigh skin excision. Then the thigh is adducted, and a vertical (12) several centimeters lateral to the prior vertical (11) is dropped from the lower abdominoplasty incision parallel to the prior line and that demarcates the upper medial thigh excision.
Markings for the vertical medial extension of the spiral thighplasty follow (Figs. 4.7 and 4.8). With the foot flat on the table and the thigh flexed, the anterior thigh skin excess is massaged across to the mid-medial thigh. As the thigh skin is pushed further posterior, a straight line (13) is drawn from the labia, at the adductor tendon, to the medial knee several centimeters posterior to the medial meridian of the thigh. At the middle of the thigh, the excess medial skin is gathered together. The width of resection from the previously marked line to the posterior thigh is gathered. That point (14) becomes the center of an ellipse that tapers at the knee and the labia majora. The posterior line of the ellipse is adjusted to change the width of resection as determined by sequential gathering. The medial thigh markings are re-inked to imprint the color onto the opposite side by adducting the thighs and rolling them together. The appropriateness of the width of resection is determined by gathering the skin. When the marked lines meet under slight tension prior to the resection, there is confidence that closure is possible after actual skin and fat removal. Cross-hatch alignments are drawn.
Case 4.7 stands to allow confirmation of the anterior markings. Adequacy of resection, symmetry, and level are established. The patient is turned 180° to draw a superior anchor upper posterior excision line (15) along the lower back as a continuation of line 5 over the iliac crests. The left and right 15 lines meet several centimeters superior to the intergluteal cleft. Buttock skin resections remove loose skin and raise the buttocks. The width of resection is determined while standing and with upward pushing of the ptotic buttocks to line 15. She did not accept the increased wound healing risks of adipose fascia flap augmentation. As such, line 16 is drawn inferiorly so that descended buttocks can be pushed and squeezed superiorly to line 15. Line 16 tapers to the superior margin of the intergluteal fold. She pulls up on the buttocks to the extent of the planned resection for a line 17, which is a continuation of line 11




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








