62. Body Contouring in Massive-Weight-Loss Patients
Jeff Chang, Rohit K. Khosla, Joseph Hunstad
CLASSIFICATION OF MORBID OBESITY1,2 (Table 62-1)
Table 62-1 National Institutes of Health Classification of Overweight and Obesity
| BMI (kg/m2) | Obesity Class | |
| Underweight | <18.5 | |
| Normal | 18.6-24.9 | |
| Overweight | 25.0-29.9 | |
| Obese | 30.1-34.9 | I |
| Severely obese | 35.0-39-9 | II |
| Extremely obese | 40.0+ | III |
■ Obesity: Body mass index (BMI) >30 kg/m2
■ Severe obesity: BMI >35 kg/m2
■ Morbid obesity: BMI >40 kg/m2. Morbidly obese patients exceed their ideal body weight (IBW) by >100 pounds or are >100% their IBW.
■ Super obesity: BMI >50 kg/m2. These patients exceed their IBW by >225%.
COMORBIDITIES OF MORBID OBESITY1,2
■ Osteoarthritis
■ Obstructive sleep apnea
■ Gastroesophageal reflux
■ Lipid abnormalities
■ Hypertension
■ Diabetes mellitus
■ Congestive heart failure
■ Asthma
SENIOR AUTHOR TIP: Following massive weight loss (MWL), 70% of patients experience a significant reduction in self-image due to the deflated nature of their tissues.
COMPLICATIONS OF SKIN REDUNDANCY
■ Intertriginous infections/rashes
■ Musculoskeletal pain
■ Functional impairment, especially with ambulation, urination, and sexual activity
■ Psychological issues such as depression and low self-esteem
BARIATRIC SURGERY TECHNIQUES2
■ Performed through traditional open techniques or laparoscopic techniques.
Laparoscopic techniques substantially reduce the morbidity from postoperative wound infections, dehiscence, and incisional hernias.
RESTRICTIVE PROCEDURES
■ Manipulate the stomach only
■ Reduce caloric intake by decreasing the quantity of food consumed at a single meal
• Vertical banded gastroplasty (VBG): Not very effective, because >50% of patients unable to maintain weight loss
• Laparoscopic adjustable gastric band (lap band): Achieves approximately 50% reduction of excess weight
• Gastric sleeve
► Gastric tube created by resecting greater curvature of stomach
► 70% remission of type 2 diabetes, which is less than with gastric bypass3
► Mean excess weight loss 50% at 6 years3
• Orbera weight loss balloon (Apollo Endosurgery)
► Fluid-filled intragastric balloon to decrease gastric capacity
COMBINATION RESTRICTIVE AND MALABSORPTIVE PROCEDURES2,3,4
■ Superior for weight reduction and decreases in comorbidities (Fig. 62-1)
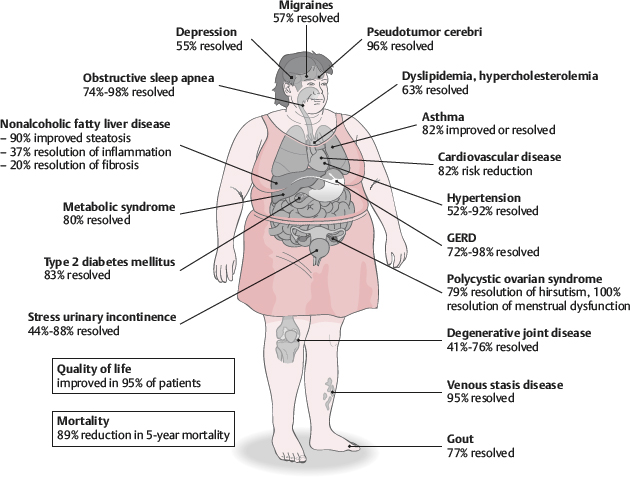
Fig. 62-1 Comorbidity reduction after bariatric surgery.
• Biliopancreatic diversion (BPD): Achieves nearly 75%-80% reduction of excess weight, produces significant nutritional deficiencies
• BPD with duodenal switch: Approximately 73% of excess weight loss
• Roux-en-Y gastric bypass (RYGB): This is the most common bariatric procedure performed and is considered the benchmark. It achieves excess weight loss >50%. Vitamin and mineral deficiencies present in 30%-40% of patients.
SENIOR AUTHOR TIP: Space-occupying balloons are becoming more popular in the United States and worldwide. They have been shown to be effective for achieving weight loss, particularly for the low and moderate BMI patients. Laparoscopic adjustable bands are losing popularity because of subsequent weight gain that is frequently seen.
FUNDAMENTALS OF BODY CONTOURING AFTER MASSIVE WEIGHT LOSS1,4,5
LIPOSUCTION
■ Not effective as a sole modality in massive-weight-loss patients
■ Can be used in areas of mild contour irregularities as an adjunct to excision procedures
■ Can be performed after recovery from major excisional procedures for refinement of contour
■ Can be performed at the excision or as a staged surgery. Table 62-2 presents the pros and cons of liposuction in massive-weight-loss patients.6
Table 62-2 Pros and Cons of Single or Multiple Procedures
| Pros | Cons | |
Single procedure | Elimination of additional surgery Areas are treated one at a time, which allows the area to be rejuvenated in one sitting | Significant edema may compromise the results/scarring Potential to compromise vascularity of the flaps |
Separate procedures | Requires additional surgical stage Debulking is completed prior to excision Avoids edema associated with liposuction | Additional surgical stage is necessary Cost of additional surgery Additional recovery time Tissues may stiffen and make later advancement more difficult |
TIMING OF BODY CONTOURING AFTER BARIATRIC SURGERY1,4,5,7
■ Delay surgery until the patient’s weight has stabilized for at least 6 months. This corresponds to ~12-18 months after gastric bypass.
■ Reasons to delay surgery until stable weight achieved:
• Patients have time to achieve metabolic and nutritional homeostasis.
• The period of rapid weight loss is detrimental to wound healing.
• Aesthetic outcomes are better for patients near their IBW.
■ Most patients will settle at a BMI of 30-35 kg/m2 after bariatric surgery.
• Consider motivated patients in this category for an initial panniculectomy or breast reduction to improve comfort during exercise.
• This may facilitate lifestyle changes that will result in further weight loss and provide better aesthetic outcomes with subsequent surgery.
■ The best candidates for extensive body contouring after massive weight loss will have a BMI of 25-30 kg/m2.
SENIOR AUTHOR TIP: Massive-weight-loss patients can be considered either “complete” or “incomplete,” based on residual subcutaneous fat. Most massive-weight-loss patients fall in the “incomplete” category, requiring reduction of subcutaneous tissue in addition to skin resection.
PREOPERATIVE EVALUATION1,4,8
■ Record greatest and presenting BMI.
■ Assess stability of medical comorbidities and psychiatric problems.
• 40% of bariatric patients are treated for psychiatric diagnoses.
■ Determine smoking history.
■ Common nutritional deficiencies
• Iron deficiency anemia
• Vitamin B12
• Calcium
• Potassium
• Zinc
• Fat-soluble vitamins (A, D, E, K)
• Protein deficiencies
■ Preoperative laboratory tests should include complete blood cell count (CBC), electrolytes, blood urea nitrogen (BUN), creatinine, uric acid, liver function tests, glucose, calcium, ferritin, total protein, albumin/prealbumin, B12/folate, prothrombin/partial thromboplastin time (PT/PTT), fat-soluble vitamins.
SENIOR AUTHOR TIP: “Complete” weight-loss patients are more likely to have had a significant bypass procedure resulting in anemia, protein, and other deficiencies. Preoperative evaluation and treatment is imperative for proper wound healing.
SURGICAL STRATEGY
■ The goals of surgery are to alleviate the functional, aesthetic, and psychological impairments from skin redundancy.
■ Determine the priorities of the patient. However, general sequence should be:
1. Trunk, abdomen, buttocks, lower thighs
2. Upper thorax/breasts, arms
3. Medial thighs
4. Facial rejuvenation
STAGING CONSIDERATIONS9
■ Body contouring surgery in patients requiring several areas of correction is multistaged to best minimize complications, pain, and need for blood transfusions.
■ Solo surgeon versus team approach
• The team approach can accomplish more in one stage.
• Patient safety is paramount.
• Longer operative times will increase likelihood of morbidities (e.g., hypothermia, anemia, thromboembolism, and wound complications).
• Design operating times that are patient-, surgeon-, and practice-specific.
■ The greater the drop in BMI, usually the greater the deflation.
■ Generally, more resection can be accomplished at one time with greater deflation or lower BMI.
■ Determine patient’s ability to tolerate long procedures.
■ Evaluate patient’s assistance at home for recovery process.
■ Patients should be back to their preoperative health status before returning to the operating room. Recovery of at least 3 months is usually required before performing additional stages.
SENIOR AUTHOR TIP: A sequence of three procedures is usually required to complete body contouring following massive weight loss. This can often require 1 year or more.
PHYSICAL EXAMINATION
■ Assess body habitus of patient.
■ Evaluate regional fat deposition.
■ Evaluate laxity of the skin envelope.
■ Evaluate quality of skin-fat envelope, which depends on degree of deflation.
■ Estimate extent of tissue resection using a pinch test.
■ Assess “translation of pull,” which is the extent that distant tissue is affected with region of resection.
■ Evaluate for old scars.
■ Anticipate location of scars and expect scar migration.
TISSUE CHARACTERISTICS AND SURGICAL TECHNIQUES
TRUNK/ABDOMEN1,6,7,10
■ The abdomen usually has the greatest deformity in massive-weight-loss patients.
■ Most tissue descent is seen along the lateral axillary lines.
■ The truncal tissues take on an appearance of an inverted cone (Fig. 62-2).
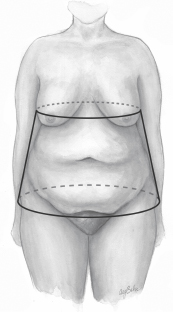
Fig. 62-2 Truncal body contour after massive weight loss. The trunk takes on the form of an inverted cone. The soft tissue is narrow at the rib cage and wider at the pelvic rim. A belt lipectomy eliminates the inferior aspect of the cone.
■ The mons pubis will have varying degree of ptosis.
■ Surgical goals
• Flatten contour.
• Tighten abdominal wall with fascial plication.
• Repair ventral hernia, if present.
• Elevate the mons pubis.
Preoperative Evaluation of the Trunk/Abdomen
■ Identify locations of old scars on the abdomen.
■ Determine the extent of the panniculus and descent of abdomen onto lateral thighs.
■ Identify any presence of hernias.
■ Assess extent of mons ptosis.
■ Assess for presence/extent of midback or lower back rolls.
■ Assess for buttock ptosis and contour. Determine if patient may benefit from buttock autoaugmentation.
Surgical Approach to the Trunk/Abdomen1,6,7,10
■ Traditional abdominoplasty techniques fail to maximally improve body contour in this patient population, because they do not address the lateral tissue laxity.
■ Fleur-de-lis abdominoplasty (Fig. 62-3) can be performed for patients without back and lateral thigh ptosis.
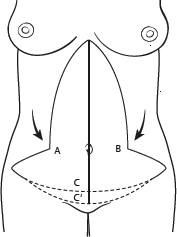
Fig. 62-3 Markings for a fleur-de-lis abdominoplasty. Redundant vertical tissue above the umbilicus is removed as a triangle connected to the redundant skin in the lower abdomen, which is marked as a standard abdominoplasty. Points A and B will join as an inverted-T closure in the midline at the pubic symphysis (point C). In patients with significant mons ptosis, point C is marked 4-6 cm below to resect additional inferior redundancy and to elevate the mons.
■ Circumferential belt lipectomy/lower body lift (Fig. 62-4) addresses the circumferential nature of the tissue ptosis seen in the trunk.7
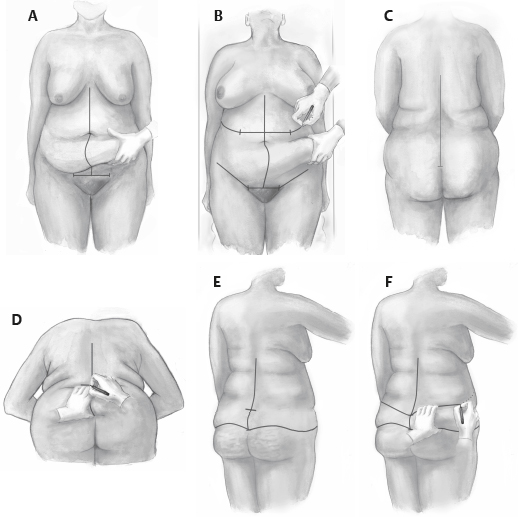
Fig. 62-4 Markings for a belt lipectomy. A, The midline is marked initially. The horizontal pubic incision is marked below the natural hairline to allow elevation of the mons. The inferior midline of the closure should be level with the pubic symphysis. The pannus is elevated superiorly and medially in the direction of the arrows to allow marking of the lateral extension of the inferior incision to just below the anterior superior iliac spine (ASIS). B, The superior markings are made anteriorly using a pinch technique to determine the extent of resection. C, The midline of the back is marked with the inferior point at the coccyx. D, The patient is slightly bent at the waist, and the pinch test is used to estimate the superior extent of resection. E and F, The superior and inferior back marks are made to meet the abdominal marks laterally.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree