Bilobar and Trilobar Forehead and Scalp Flaps
M. NARAYANAN
Immediate reconstruction of head and neck defects resulting from excisions of huge cancers is a unique procedure in plastic surgery. The principles of immediate reconstruction after excision of oropharyngeal cancers are well documented (1, 2, 3).
Wide variations are reported in the geographic incidence of squamous cell carcinoma of the mouth. Although it is as low as 2% of all cancers in Western countries, it offers a formidable problem in South India, accounting for 39.52% of all cancers in males and 18.80% of all cancers in females. Management becomes even more difficult because 86% of these patients report in the late stages of their disease; consequently, conventional radiotherapy cannot cure the primary growth more than 50% (4).
In patients with residual primary growth, the threat to life can be treated only operatively. If the tumor and the draining lymph nodes can be excised and the face reconstructed, solutions to the problems of offensive odor, trismus, pain, and drooling can be offered. Fortunately, distant metastasis occurs in only 1% of patients. The predominant concern of the surgeon is cancer clearance, however mutilating the excision may be. Not less important, though, are reconstruction and rehabilitation of the patient. The surgeon is encouraged to perform a wider excision if a versatile flap that can effectively reconstruct large postexcisional defects is available.
INDICATIONS
In the flaps described below, irradiation is still possible postoperatively because the blood supply to the flaps is quite good. In males, a beard can be grown to help conceal facial asymmetry.
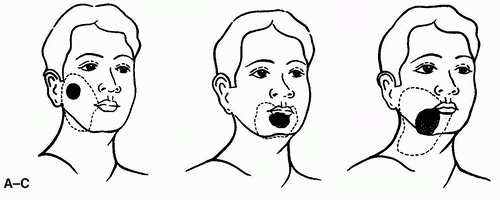
The anatomic locations of postexcisional facial and neck defects are shown in Figure 107.1. Treatment of the primary tumor, including neck dissection, was previously described by the author (5).
FLAP DESIGN AND DIMENSIONS
Bilobar Flap
The superficial temporal artery divides into a frontal and an equally large parietal (posterior) branch. The frontal branch is the one used for the forehead flap, and it can be used to reconstruct the intraoral mucosa. The scalp, supplied by the parietal branch, can be used for external skin coverage (see also Chapter 108).
OPERATIVE TECHNIQUE
Bilobar Flap
The branches of the superficial temporal artery are identified by palpation or with a Doppler device. The lines of incision start as with the standard forehead flap, but at a point about 5 cm above the bifurcation of the anterior and posterior branches of the temporal artery, the incision deviates posteriorly to enclose a wide parietal scalp flap that has the exact dimensions of the skin defect. The flaps can be measured accurately by cutting out patterns of the mucosal and skin defects on sterile gauze. The frontalis muscle and the parietal scalp flap are raised at this same loose areolar tissue level.
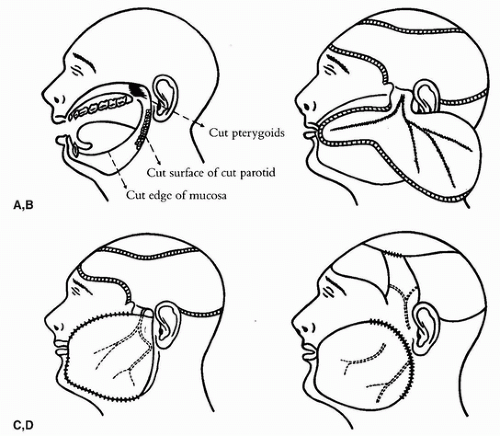 FIGURE 107.2 A: Defect of cheek and upper neck at completion of tumor excision. B: Scheme of the bilobar forehead skin and scalp flap based on the frontal and parietal branches of the superficial temporal artery. The forehead portion is used to restore cheek lining to the defect. C: Scheme of folding over the scalp portion of the flap to provide skin coverage. Note that the fold posteriorly is not divided or set into place at this operation, so a fistula is present. The scalp defect is skin-grafted. D: Several weeks later, the fold in the flap is divided. The inner edge is used to close the lining, and the outer edge is used to close the skin surface. (From Narayanan, ref. 5, with permission.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|