Ethnicity has been defined as “a complex multidimensional construct reflecting the confluence of biological factors and geographic origins, culture, economic, political, and legal factors, as well as racism.” A useful, simple definition is: “in its most elemental form, ethnicity is an expression of language, culture, social mores and folklore, while race is determined by external features—the most important of which are skin color … and hair texture.” This understanding may have contributed to the move away from the designation: “Black American” to “African American.” Ethnicity embodies cultural practices and dietary preferences that may influence disease predilection. However, unlike gender, the use of ethnicity in scientific discourse is problematic as its effect on disease is difficult to measure. With the exception of remote societies, ethnicity is often difficult to categorize, particularly in cities with large admixture. A tangible danger of ethnic profiling is when effective treatment is denied patients because it is deemed ineffective in their group. A contrary argument is that abandoning ethnic categories could hide disparities in health care delivery.
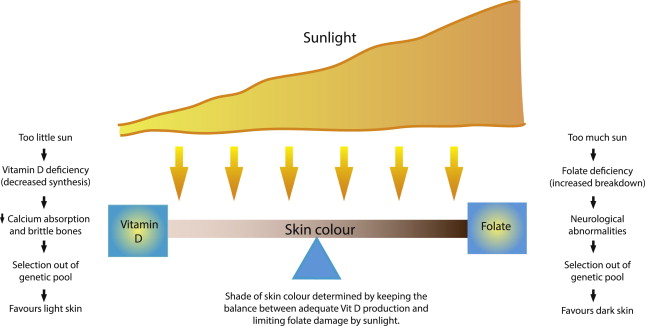
The influence of geography (climate, etc) on human variation is worth considering. The relationship between sun exposure and skin cancer is well established. However, sun-induced skin cancers predominantly occur in adults after the reproductive years and are thus unlikely to have exerted an evolutionary force for skin color variation. In this issue of Dermatologic Clinics , we are privileged to share the contribution by Jablonski and Chaplin, which elucidates the phenotypic variation within the African continent. They also proposed the most plausible hypothesis for the evolution of skin color. They suggested that skin color may have evolved because of the need to balance requirements for vitamin D synthesis versus protection against ultraviolet folate photolysis. Simply put, as humans migrated out of Africa, because of limited sunlight, those with dark skin were unable absorb enough ultraviolet light to synthesize adequate vitamin D (or efficiently absorb calcium for strong bones), were more likely to give birth to children with rickets who were less likely to successfully carry a fetus to term, and were thus selected out of the genetic pool. On the other hand, very pale skin close to the equator is prone to ultraviolet photolysis and folate deficiency. Folate is needed by rapidly dividing cells and deficiency in pregnancy increases the risk of neurologic deformities (eg, anencephaly, spina bifida), which are incompatible with a healthy life and successful reproduction ( Fig. 1 ).
The current hypothesis for the evolution of hair curl suggests that tighter curls are better for hot environments. While there is a high correlation of skin color to solar strength worldwide, this may not be the case with hair curl. For example, people in the South of India are as dark as or even darker than most Southern Africans yet have straight hair compared with tightly curly hair. This apparent discordance of skin color and hair curl warrants scientific scrutiny that may advance a new hypothesis for the evolution of hair curl.
Skin color and hair texture are variables that do confer susceptibility to dermatologic disease, as is the case in folliculitis keloidalis and pseudofolliculitis barbae so well discussed by Alexis, Heath, and Halder in this issue. The contribution by Ud-Din and Bayat takes us into the next generation of molecular mechanisms and future potential targeted treatments for keloids, hypertrophic scars, and striae. National regulatory bodies do not recognize cosmeceuticals or “cosmetics with drug-like efficacy.” However, because of various skin-benefit claims, their popularity is increasing in all populations. Draelos’s article is informative, as cosmeceuticals may confound dermatologic presentations and treatment effects. Taylor, Padya, and Molinar discuss the objective assessment and management of the prevalent problem of facial hyperpigmentation. The widely used Fitzpatrick’s classification depends on historic responses to sun exposure and is thus subjective. The use of validated cards with color shades such as the Taylor hyperpigmentation scale seems useful. Colorimetric measurements may be more objective, but no single tool has received universal acceptance.
Until recently, hair curl was classified racially—African, Caucasian, and Asian. Variation within groups becomes magnified when one considers that “Caucasian” hair can range from tightly curly to ultra-straight. The recently published quantitative classification of human hair uses 3 geometric measurements to classify human hair into 8 types. Most Afro-textured hair falls into types 5 through 8. If validated, this classification could help measure the influence of texture on hairstyle choice and alopecia. Mirmira and coauthor present potentially achievable goals. It is not common in medicine that we have, as in traction alopecia (TA), study data that can easily be translated for disease prevention. The challenge is how to bridge the kap-gap (ie, the gap between knowledge, attitudes, and practice). Unlike TA, unconquered frontiers include the commonest form of scarring alopecia comprehensively discussed by Ogunleye, McMichael and Olsen. The other is hair restoration–Rogers and Callender are pioneers because many hair transplantation centres do not offer the procedure to patients with tightly curly afro-textured hair. Yin and Tosti demonstrate how dermoscopy complements clinical examination; how it can reduce the need for scalp biopsies and guide the choice of biopsy site.
The title of this issue of Dermatologic Clinics also infers geography; sub-Saharan Africa has the highest burden of the human immunodeficiency virus (HIV). Motswaledi and Visser, in their contribution on infective and inflammatory disorders in HIV, illustrate dramatic postinflammatory dyspigmentation that often masks the diagnosis and complicates management of common dermatoses. Although antiretrovirals have dramatically improved mortality, the colliding epidemics of tuberculosis and HIV have contributed to an exponential rise in severe adverse drug reactions and exaggerated clinical presentations as eloquently demonstrated by Lehloenya and Kgokolo.
The little known human T-cell leucotropic virus (HTLV-1)-associated dermatitis discussed by Hlela and Bittencourt has been included in this issue of Dermatologic Clinics for various reasons. First, HTLV1 is a retrovirus with some similarities to HIV. Second, and important for dermatologists, the infection is associated with a childhood chronic dermatitis that may be mistaken for seborrheic (and atopic) dermatitis. Finally, HTLV1-associated dermatitis in childhood may precede hemopoietic malignancy and disabling neurologic disease in adulthood.
Finally, this issue of Dermatologic Clinics focuses on disorders that predominately affect people of African ancestry mostly because of their skin color, hair form, or geographic origin. Several overlapping terms are worth considering:
- 1.
“Phenotype” is an important disease determinant in dermatology (skin color and skin cancer, hair texture and specific alopecias).
- 2.
“Race” is not the same as phenotype or ethnicity and its use should be discarded.
- 3.
“Ethnic skin/hair” is nonspecific and could mean any population subgroup (eg, Greek, Chinese, or fair-skinned Scandinavians).
- 4.
“Ethnicity” is not the same as phenotype (eg, Africans may look similar but be different in every other way—African Muslims are culturally closer to Arabs than sub-Saharan Africans).
- 5.
Ethnicity is difficult to categorize or measure its effect in scientific studies. However, it is important to include where relevant to measure social justice and fairness.
As a result of population migration, skin color and specific genetic susceptibility may correlate. However, variability within groups and admixture make the use of skin color as a general marker of disease predilection unscientific. Skin color and hair texture do influence specific dermatologic disease, but unlike ethnicity, they are amenable to measurement. As dermatologists and scientists, the utopia would be for us to disabuse our discipline of all reference to race and, yes, even ethnicity. Various attempts have been made to objectively classify skin color and, recently, hair curl. What’s needed is the development of simple validated tools. International consensus would allow universal adoption of objective assessments that could improve study quality and patient care. What now, as we march toward this objective ideal? We use ethnicity (eg, African ancestry, Afro-textured hair—only when clinically indicated) but we do so with the recognition that it is an imprecise surrogate that should be replaced as soon as possible.
Congratulations to South Africa, the Rainbow Nation, on 20 years of Democracy. May we each contribute to the greater good, daily…
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree