Back-Table Preparation of the Liver for Transplantation
Sean C. Kumer
DEFINITION
Back-table preparation is defined as preparing the donor liver following procurement and prior to transplantation into the recipient. The back table is used to remove excess donor tissue and adequately prepare the allograft for implantation. Preparations are made to prevent hemorrhage after reperfusion of the donor liver. Aberrations of vascular anatomy are assessed and reconstructed prior to implantation of the liver.
PREPARATION
After arrival of the liver in the certified packaging, confirmation of the proper organ, identification numbers, and blood typing is performed.
The timing of the back-table preparation of the liver is determined by the recipient surgeon. The procedure takes between 30 and 90 minutes depending on the surgeon and need for arterial reconstruction.
A sterile back table with instruments, ties, sutures, clips, and a sterile basin with ice slush should be available.
The procured donor liver should be aseptically handed off to the back-table surgeon and placed within a bag containing preservation solution within the basin on ice. Care should be taken to avoid direct exposure of the organ to the ice.
TECHNIQUES
VENA CAVA
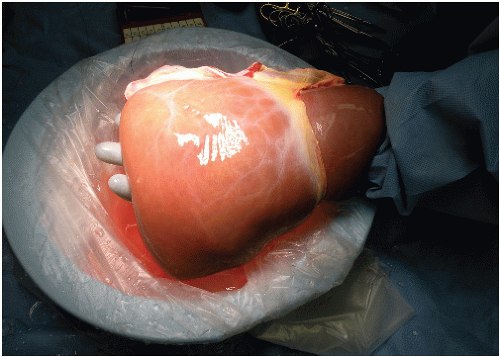
The liver should be placed with the posterior surface facing upward, exposing the vena cava along its length.
Silk sutures may be placed in either side of the suprahepatic and infrahepatic vena cava. This will allow for appropriate tension on the vena cava for dissection (FIG 3).
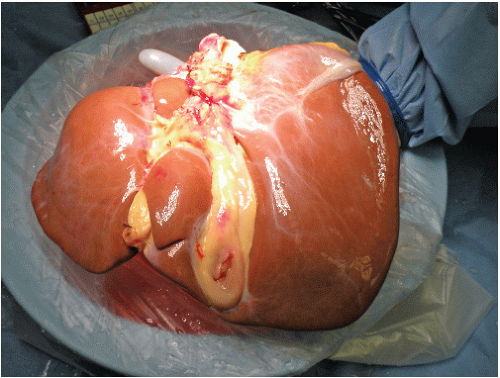
The diaphragm may be removed from the allograft with sharp dissection. The diaphragm should be cut close to the suprahepatic vena cava (FIG 4).
Excess cardiac tissue is removed from the suprahepatic vena cava.
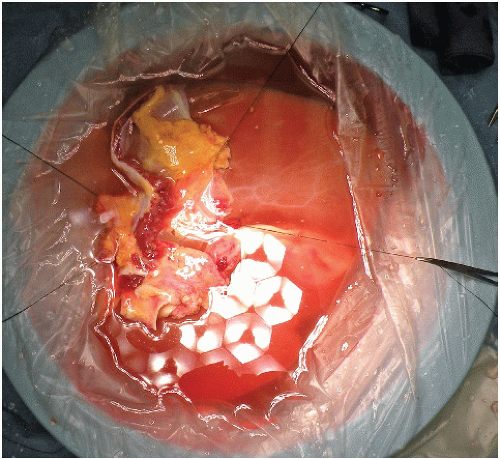
Ligation of the bilateral phrenic veins with ties, clips, or suture is performed at this step (FIG 5).
Care should be taken to avoid shortening the suprahepatic vena cava so as to prevent distortion or impingement on the hepatic venous outflow.
Dissection of the remaining vena cava should continue with ligation of the adrenal vein branches.
Occasionally, ligate and divide several of the short caudate venous branches to allow for more length on the infrahepatic vena cava. This decision depends in part on the plan for implantation (piggyback, caval replacement, or cavocavostomy).
Preparation of the vena cava may be variable at this point. Evaluation of the recipient’s anatomy and the recipient surgeon’s preference for implantation method
need to be considered. It is critical to keep several implantation options open, as the specific approach is at times determined during the hepatectomy. For example, the ability to do a bicaval liver transplant must be maintained for the recipient surgeon.
Piggyback technique—The infrahepatic vena cava should be oversewed, tied, or stapled (FIG 6).
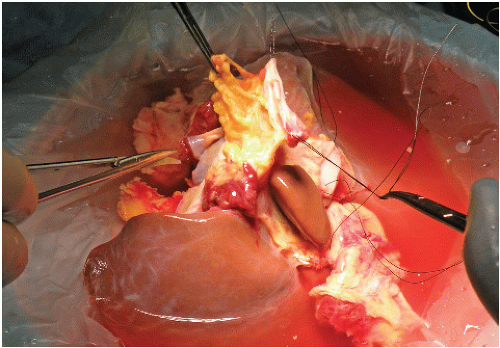
FIG 4 • Removal of diaphragm from donor liver and vena cava.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access