Babysitter Nerves for Facial Reanimation
Adel Y. Fattah
DEFINITION
The aim of facial reanimation is to provide facial symmetry at rest and synchronized coordinated facial expression.
When the facial nerve is unusable but facial musculature is intact, reinnervation is preferred.
Cross face nerve grafting (XFNG) allows for the contralateral facial nerve to direct its activity to the paralyzed side.
The main issue for this technique is the long period of time for nerve regeneration to occur along the graft. This results in irreversible muscle atrophy unless the grafts are performed soon after initial denervation, as it typically takes 6 to 12 months for axons to reach their target muscle.
To overcome this, the babysitter procedure was introduced to provide a rapid reinnervation to the muscle while awaiting nerve growth across these long grafts.3
The term babysitting in its original context is used to describe the maintenance of viable musculature while waiting for the cross face nerve grafts to grow and reinnervate the musculature to achieve spontaneous animation.
Since its inception using the hypoglossal nerve, the principle has developed, and other cranial nerves have been used to babysit the facial musculature such as the motor nerve to masseter.4
The author has exclusively used the masseter nerve because there is less morbidity.
There is little or no functional deficit produced by using the motor nerve to masseter as a donor. By contrast, hypoglossal nerve sacrifice can result in issues with speech and swallowing, even in the minihypoglossal transfer.
There is no synkinesis with tongue movement; there is some with chewing, but this abates with training.
There is no need for interposition grafts of sural or greater auricular nerves with their own donor sensory deficits. Additionally, axons will only have to cross one neurorrhaphy, which reduces time to reinnervation.
To combat the axonal dropout in XFNG, another form of babysitting may be used.
This involves the coaptation of an end-to-side sensory nerve to the cross face nerve graft at a point along its length to provide a source of neurotrophic factors to encourage axonal growth toward the target.5
Therefore, reanimation of the paralyzed face can be optimized by using a motor nerve to babysit the musculature and sensory nerves to babysit the cross face nerve graft.
In this chapter, the author will describe the preparation of the motor nerve to masseter and its transfer to the ipsilateral facial nerve to babysit the facial musculature. The sensory babysitting of the cross face nerve graft will also be described.
ANATOMY
The masseter muscle is one of the muscles of mastication.
It arises from the lower border and medial surface of the zygomatic arch and inserts into the lateral surface of the mandible.
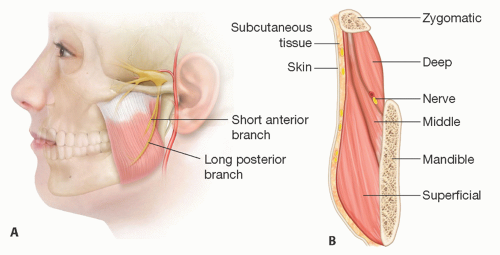
The muscle consists of three layers—superficial, middle, and deep (FIG 1).
The superficial muscle fibers pass backward and downward, and the deeper fibers are more vertical. The motor nerve to masseter is derived from the mandibular division of the trigeminal nerve. It leaves the infratemporal fossa by passing over the lateral pterygoid muscle and
mandibular notch. It enters the masseter muscle from its deep surface and courses down between its deep and middle layers having a diameter of 1 to 2 mm. It becomes more superficial distally toward the anterior inferior part of the muscle and runs alongside the (friable) vascular pedicle that arises from the inferior alveolar artery. Proximally, within the muscle, it gives a number of small short branches, but it typically has one or two significant branches, one longer than the other, that can yield 2 to 3 cm of useful nerve before terminal branching.6,7,8
The facial nerve exits the stylomastoid foramen, turns superficially, and immediately enters the substance of the parotid gland where it is classically described as dividing into five branches—temporal (frontal), zygomatic, buccal, mandibular, and cervical.
The nerve usually divides into upper (temporal) and lower (cervical) trunks at first, from which these branches arise. In practice, they comprise five variably interconnected groups of branches hereafter referred to as divisions.
Despite the various studies of facial nerve anatomy, it may be more useful to envision the facial nerve as consisting of physiological and functional divisions that do not necessarily correlate to the anatomic distribution of branches but instead relate to muscular groups and actions.
The temporal branch of the facial nerve exits from the upper pole of the parotid gland at the level of the zygomatic arch and becomes superficial being plastered onto the underside of the temporoparietal fascia.
The course of the nerve follows a line drawn from 0.5 cm below the tragus to 1.5 cm above the eyebrow, but 3D modeling demonstrates that the branches cover a triangular area bordered between a line through the palpable zygomaticofrontal and zygomaticotemporal sutures and a vertical line 1 cm in front of the auditory meatus.9 At the lateral margin of frontalis, these branches run deep to frontalis and orbicularis oculi (which it innervates), eventually reaching the glabella region to supply the depressors of the brow.
The zygomatic division leaves the parotid gland to run just inferior the zygomatic arch immediately deep to the superficial musculoaponeurotic system (SMAS) to innervate the elevators of the upper lip and lower portion of orbicularis oculi.
Distally, it runs on the undersurface of the zygomaticus muscle complex before ramifying more medially in the face. The buccal branches exit the anterior border of the parotid gland and run inferior to the parotid duct and on the surface of the buccal fat pad deep to the SMAS layer to supply the muscles of the mouth and cheek.
Both zygomatic and buccal divisions have a highly overlapping distribution of innervation that allows transection of one or more branches without weakness; this is the basis of XFNG.
The mandibular branch leaves the lower portion of the parotid gland and swings down below the ramus of the mandible to supply the muscles of the lip and chin.
Cadaveric dissections demonstrate that the nerve always comprises at least three major branches that run on the undersurface of the platysma and superficial to the facial vessels.10
PATHOGENESIS
A nerve injury that is significant enough to damage the axon leads to Wallerian degeneration. It takes around 72 hours for the process to become established to the point that nerve conduction fails.
One method of determining such axonotmesis vs neurapraxia is to demonstrate conduction in the peripheral nerve segment. When there is no regrowth of axons distally, the end organs eventually undergo irreversible changes, which hinder muscle recovery from prolonged denervation.11
The quality of the recovery following repair depends chiefly on the number of axons that successfully reach their correct targets and the subsequent myelination of these axons.
Therefore, treatment is best achieved by reinnervating the end organ as effectively as possible, specifically delivering as many axons as soon as possible to the end organ.
As well as changes in the muscles, nerves that are chronically denervated (ie, have suffered axonotmesis) undergo changes proximally; the myelin sheaths collapse with reductions in conduction velocity and changes in the cell bodies.
Long nerve grafts such as XFNGs also suffer chronic denervation changes reducing the capacity for nerve regeneration. Donor axons from sensory nerves can protect nerve grafts from chronic denervation and thereby improve axonal growth through the graft.5 Such protection of chronically denervated nerves improves regeneration due to endogenous trophic support.12
PATIENT HISTORY AND PHYSICAL FINDINGS
The most important factor in the history is determining the premorbid status of facial animation and time since the injury as this will determine the presence of viable facial musculature that may act as a target for reinnervation.
In general, the sooner innervation is re-established, the greater the likelihood of a better functional outcome.
Most clinicians would suggest that reinnervation of musculature is attempted within 12 to 24 months of injury. Thereafter, results may be unpredictable.
The examination is directed toward muscle-specific objectives and determines the presence of intact donor nerves. Therefore, examination of the facial nerve of the affected side should delineate that the deficit one is attempting to reconstruct.
Muscle-specific treatment goals include brow elevation, eyelid closure, smile, and lower lip function.
Cranial nerve examination is performed specifically looking for donor nerve activity, such as contralateral facial nerve function (examining each division) and activity of the muscles of mastication.
Palpate the cheek and feel for the presence and power of masseter and temporalis contraction to determine innervation.
Examination of the tongue is performed for deviation that will indicate hypoglossal nerve activity.
SURGICAL MANAGEMENT
General management of facial palsy has been published in detail elsewhere,13 but the principles of reanimation remain: the re-establishment of movement, for which the muscle is required with a nerve to control that motor function.
Soon after facial nerve injury, the muscle remains intact for a short time, and reinnervation of this can yield good results.
Once the native muscle has atrophied, new muscle will need to be imported to re-establish the muscle-specific functions outlined above.
The key points to evaluate are the presence of a functioning proximal nerve stump (mainly based on the history) and the time elapsed after the injury (that will indicate the likelihood of functioning facial musculature).
By definition, the requirement for a cranial nerve transfer (babysitter) intimates that a proximal nerve stump is unavailable (FIG 2).
Preoperative Planning
Preoperative planning is informed by clinical examination as outlined above.
Electrical conduction studies are useful if there is debate over the presence of viable facial musculature, but it is generally not used after 1 year because after 18 to 24 months after injury, the likelihood of adequate active muscle sufficient for reconstruction is low.
Positioning
The patient is positioned supine on the operating table with a shoulder roll to extend the neck and a head ring to support the head that is rotated to the opposite side (FIG 3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree