Axial Paramedian Forehead Flap
G. C. BURGET
EDITORIAL COMMENT
This chapter combines both the art and science of plastic surgery with very gratifying results.
A vertical, axial paramedian forehead flap is the donor tissue of choice for nasal reconstruction. However, in some situations it is not ideal. It is thicker than the normal skin of the nasal dorsum, and when it is used to resurface this subunit it produces a greater aquiline hump than the original nose possessed. Because it is somewhat rigid, forehead skin is not an ideal replacement for the alar lobule. The soft skin of a nasolabial flap more easily forms itself into a blob, which resembles the normal convexity of the alar subunit. In children, the upper half of the forehead is covered with fine lanugo hairs. These hairs become thick when they are denervated causing the forehead flap nose to be fuzzy during the first year following reconstruction. Nevertheless, the paramedian forehead skin is the ideal replacement for nasal tip skin, and may be used successfully to restore any part of the nose.
ANATOMY
As shown by McCarthy and associates (1), vertical branches of the angular and supratrochlear arteries cross the superior orbital rim in the region of the wrinkle line that lies perpendicular to the corrugator muscle. They cross the orbital rim deep to the frontalis and corrugator muscles and rapidly enter the subcutaneous layer as they ascend the forehead. In the upper half of the forehead, many fine branches of the arteries lie in the subcutaneous fat close to the dermis. The entire frontalis muscle and some of the subcutaneous fat may be removed from the distal end of a paramedian forehead flap without injuring its axial arteries.
FLAP DESIGN AND DIMENSIONS
The many modifications of the forehead flap have been designed to increase its length, so that columellar defects may be covered, or to enlarge its surface area, so that the total nose may be resurfaced. Nonvertical variations, such as New’s sickle flap or Gillies’ up-and-down flap, deprive the forehead flap of its axial quality. Converse’s scalping flap is large enough to cover the entire nose, but as the name implies, it increases the patient’s morbidity. In truth, the classical vertical paramedian forehead flap will cover the entire nose from radix to columellar base without the necessity for extravagant variations or mechanical forehead tissue expansion.
After millennia of experience, new principles continue to emerge:
The flap is designed vertically and axially. This makes it vascularly robust, so that it may be radically thinned and depilated.
The base of the flap is made no wider than 1.5 cm for easy mobility without strangulation.
The base of the flap is positioned to include a branch of the angular-supratrochlear arteries, which is located with the Doppler pulse amplifier.
Additional length is attained by extending the flap’s proximal end across the orbital rim or its distal end into the hair-bearing scalp.
The flap is not designed to fit the nasal defect, for the nasal defect, distorted by edema, scar contraction, and local injections, does not represent what is missing from the nose.
An exact three-dimensional pattern of nasal surface subunits taken from the contralateral normal side of the nose or from an ideal model is used as a template for the flap’s design.
No marginal excess of skin is included when the flap is incised. This minimizes centripetal flap contraction, which obliterates surface contour.
Distal portions of the flap are thinned to the thickness of nasal tip skin and are depilated where necessary.
The base of the flap is excised and discarded, not replaced on the forehead.
The upper half of the donor defect is allowed to close by biologic wound contraction and forehead skin autoexpansion. There is no necessity for skin grafts, local flaps, or mechanical tissue expansion to close this secondary defect.
It requires the talents of a tailor to fashion a forehead flap. A flap cut too small collapses the cartilage framework of the nose. A flap cut too full allows centripetal contraction to pull the excess skin into a blob, obscuring nasal surface contour. The pattern for a made-to-measure forehead flap may be fashioned from heavy aluminum foil such as that used to pack sutures.
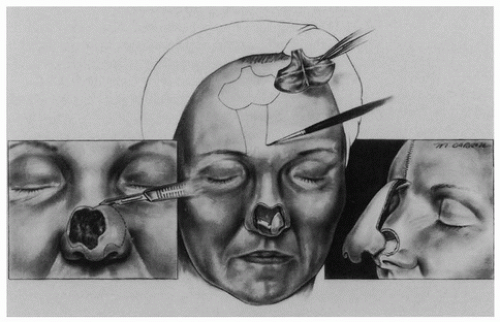
There is a strong impulse to make the flap fit the nasal defect, as Millard has said (2), “to fill the hole.” However, the defect that exists at the time of nasal reconstruction does not reflect the amount of skin missing from the nose. It has been enlarged by edema and distorted by wound contraction and intraoperative lidocaine injections. The shape of the defect is not the shape nor size of the missing part of the nose. Therefore, one should turn to the remaining normal contralateral parts of the nose for a pattern. The nasal defect is sketched in mirror image with methylene blue dye on the normal contralateral side of the nose, which is undistorted by inflammation or injections. If the entire nose is missing, then a model of an ideal nose may be used to create a pattern for the flap. The defect may be enlarged to cover entire topographic surface subunits of the nose (Fig. 55.1), especially when convex regions such as the alar lobule, dorsum, hemitip, or tip subunits are to be replaced. A trapdoor contraction occurs in the transplanted forehead tissue and the bulge of the entire subunit comes to resemble the normal bulge of an ala, dorsum, hemitip, or tip.
The forehead flap is designed vertically to preserve its axial quality. Branches of the supratrochlear and angular vessels are located with the Doppler pulse amplifier, and the base of the pedicle is then centered on these vessels. This allows the proximal two-thirds of the pedicle to be designed very narrow without compromising its blood supply. Assured of an axial blood supply, the flap may be thinned and depilated and thus may include up to 1.5 cm of hair-bearing scalp tissue for replacement of the columella. If the flap is designed on an angle as slight as 15° off the vertical, it will cut across branches of the axial vessels, in which case thinning and depilation become risky. It is better to maintain the vascular robustness of an axial flap and obtain the needed flap length from the hair-bearing scalp than to gain length with an eccentric flap design. A vertical forehead flap in a non-cigarette smoker will easily bear the rough treatment of thinning and depilation, while an oblique random forehead flap may not be thinned and must therefore be applied to the surface of the new nose with all its redundant layers of tissue.
The pattern of the missing surface subunits is designed in three dimensions from the remaining normal side of the nose (or from an ideal model). After the exact location of vascular branches has been confirmed with the Doppler pulse amplifier, the pattern is flattened to two dimensions and traced with methylene blue near the hairline in axis with the supratrochlear vessels on the side of the nasal defect. A 1.5 cm columellar extension of hair-bearing scalp may be included distally.
OPERATIVE TECHNIQUE
The base of the pedicle is traced 1.2 to 1.5 cm wide, and no wider, to allow axial rotation (twisting) without strangulation. The proximal two-thirds of the pedicle may be quite narrow and then expand suddenly to incorporate the pattern. When the flap is incised, the cuts are made on the inside of the blue lines so that not even a half millimeter of excess skin is included. In its distal 2 cm, the flap is elevated superficial to
the frontalis muscle. Proximally, the frontalis muscle is elevated off the periosteum with the pedicle to protect the axial vessels. If extra length is needed, corrugator muscle fibers are divided using magnifying loupes so that vascular branches are preserved while restricting bands of muscle are released. If the flap still proves short, then the pedicle is extended across the orbital rim, including a bit of the eyebrow if necessary. Again, it is helpful to mobilize the pedicle by dividing corrugator muscle fibers while preserving vascular branches.
the frontalis muscle. Proximally, the frontalis muscle is elevated off the periosteum with the pedicle to protect the axial vessels. If extra length is needed, corrugator muscle fibers are divided using magnifying loupes so that vascular branches are preserved while restricting bands of muscle are released. If the flap still proves short, then the pedicle is extended across the orbital rim, including a bit of the eyebrow if necessary. Again, it is helpful to mobilize the pedicle by dividing corrugator muscle fibers while preserving vascular branches.
After the flap is elevated, its borders and its distal 2 cm are thinned using curved Joseph’s scissors. Hair follicles remaining in the distal part of the flap are clipped off with fine scissors under 2.5× magnification. During the thinning, axial branches of the supratrochlear-angular arteries visible in the subcutaneous tissue very close to the dermis are preserved. During thinning close attention is given to the nasal defect, since some of its regions require more subcutaneous tissue than others, and the flap may be thinned accordingly. The thinned flap is transported to the nasal defect. Right-sided flaps rotate clockwise; left-sided flaps rotate counter-clockwise. Key sutures fix the flap in position. Fine sutures adjust its edges.
Suturing may be done in such a way as to enhance nasal contour. At the junction of the upper lip, the cheek, and the alar groove, the flap is pulled inferiorly before the key stitch is placed (3). This forces the alar tissues to bulge in a normal convexity and stretches the tissues of the lateral side wall so that they do not bulge. A no. 19 suction drain may be placed under the forehead flap and hooked to a vacuum tube. The negative pressure created pulls the various layers of the nose together during the postoperative phase.
The secondary forehead defect continues to vex surgeons. It has not been generally recognized that the forehead is a forgiving donor surface. Although frequently it cannot be closed with sutures, nevertheless, skin grafts, local flaps, or mechanical tissue expanders are not needed. In fact, they compound the deformity and increase patient morbidity. The forehead defect that remains after local advancement of tissues will close biologically by the process of wound contraction and forehead autoexpansion. These processes require neither further incisions, pain, hospitalization, inconvenience, nor expense. They are performed without compensation by the myofibroblasts. Any frontalis muscle remaining in the donor defect is removed. Then the forehead and scalp surrounding the donor site are elevated from the periosteum of the frontal bone for 7 cm bilaterally and superiorly. Two to four heavy simple sutures tied under moderate tension pull the limbs of the defect together. These key sutures are placed close to the wound edge to minimize their stitch marks, since they will remain in place for 10 days. Distal dog-ears are excised laterally and superiorly. The limbs of the defect are closed in layers. Exposed periosteum in the central open region of the donor wound is protected from desiccation with petrolatum gauze and ointment. No contraction occurs in the open defect for about 3 weeks. Then, during the fourth and fifth postoperative weeks, the wound rapidly contracts, autoexpanding the adjacent skin and producing a surprisingly forgiving result. Mechanical tissue expansion, local rotation or advancement flaps with their necessary scars, or the postage-stamp application of a skin graft is unnecessary. These adjunctive procedures actually increase patient discomfort, scarring, or contour deformities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree