36. Asian Blepharoplasty
Jerome H. Liu, Richard Y. Ha, Lily Daniali, William Pai-Dei Chen
BACKGROUND
■ Mikamo performed first reported double-eyelid operation in 1896.1
• Nonincision method using three sutures of silk thread removed postoperatively
■ Sayoc,2 Millard,3 and Fernandez4 first reported on it in Western literature in 1950s.
■ Operation gained popularity in Asia after World War II following the influx of whites.
• Upper lid blepharoplasty is now the most common plastic surgery procedure in Asia.
■ Approximately 30%-50% of Asians have a natural supratarsal crease.5
■ Not a “Westernizing” of the eyelid
• Patients typically request a natural look that opens the eye, while respecting their Asian identity.6
DIFFERENCES BETWEEN WHITE AND ASIAN EYELIDS7
■ Characteristics of “single fold” eyelid (Fig. 36-1)
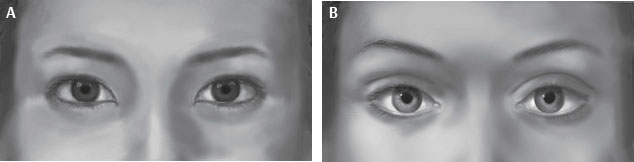
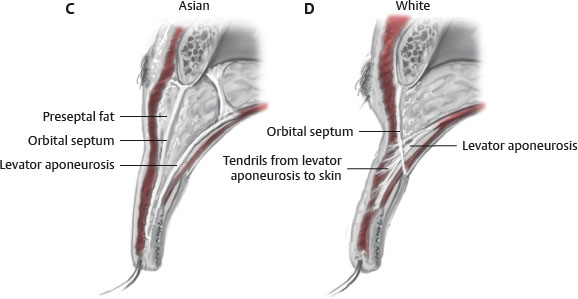
Fig. 36-1 Corresponding cross sectional fascial anatomy of A, an Asian eyelid and B, a white eyelid. Note the low fusion of the septum and levator in the C, Asian eyelid versus the high fusion in the D, white eyelid. Also note the presence of abundant preseptal fat and the lack of fascial attachments from the levator to the orbicularis and skin.
• Absent or short superior palpebral crease
• Preseptal fibroadipose tissue or orbicularis muscle thickening
• Diffuse, poorly defined and variable insertion of septum into levator aponeurosis
► Can insert as low as 2 mm below superior tarsal border
• Inferior descent of preaponeurotic (prelevator) fat
• Short tarsal height (Asians 6.5 ± 8.0 mm; whites 11.3 ± 1.7 mm)8
■ Two theories of superior palpebral crease formation
• Levator-dermal expansion2,9–13
► Traditional theory describes fibrous extensions of the levator inserting into dermis to create the palpebral crease in whites.
► Expansions from levator aponeurosis pierce orbicularis and insert into dermis or subcutaneous tissue of pretarsal skin.
► Anchoring produces characteristic fold in upper eyelid.
► Asians lack a palpebral fold, because the levator does not penetrate the septum. Therefore there are no fibrous extensions of the levator into the skin or subcutaneous tissue.
SENIOR AUTHOR TIP: I support the view of levator-dermal extension. Since Collins’ paper in the 1980s, electron microscopy (EM) studies have confirmed the presence of microtubules (microfibrils) that extend to the undersurface of skin, in addition to wraparound intermuscular fascia of the orbicularis oculi.
• Levator-septal variable union13–17
► There are no clearly defined dermal expansions from the levator; there are expansions from the levator to the orbicularis muscle.14
► The formation of the crease is based on the level of union between the levator aponeurosis and orbital septum, creating a conjoined fascia.
► Crease formation is a result of the fusion of the levator and septum with adherence of the orbicularis muscle and the overlying skin.
► Whites have a high union between the levator and the orbital septum at or above the superior border of the tarsal plate, allowing a well-defined palpebral crease.
► Asians have a low or variable union between the levator and orbital septum below the superior border of the tarsal plate.
► The low attachment allows descent of preaponeurotic orbital fat between the levator and the septum to extend inferiorly.
► Abundance of preseptal fat creates a glide plane and prevents adherence between levator-septal complex and orbicularis muscle.
► Primary insertion of levator aponeurosis into orbicularis muscle occurs closer to the eyelid margin.
■ Soft tissue differences between Asian and white eyelids7,13,18
• Asian skin has thicker dermis with higher collagen content.
• Asian upper lid has more prominent preseptal fibroadipose tissue.
► Submuscular fibroadipose layer is directly continuous with eyebrow fat pad.
► Brow fat can inferiorly extend to lash line.
► Preseptal fat adds thickness and fullness to upper lid.
► Can be continuous or intimately associated with retroorbicularis oculi fat (ROOF).
• Asians have thicker pretarsal subcutaneous tissue.
► Presence of pretarsal fibroadipose tissue
• Asians have thicker and bulkier orbicularis oculi muscle.
• Abundance of bulky soft tissue contributes to poorly defined palpebral crease.
■ Epicanthal fold
• Appears as a skin web that overlies portion of the medial canthus and obscures the lacrimal caruncle, and possibly the medial portion of the sclera.
SENIOR AUTHOR TIP: The term epicanthal fold has been overapplied even to normal Asian individuals who do not have clinically significant epicanthal folds (as seen in patients with congenital syndromes like Down syndrome and blepharophimosis syndrome). The treatment, epicanthoplasty, has been overprescribed as a surgical solution when the finding is merely a medial upper lid fold (a term which I prefer), in which half of the exposed caruncle is easily seen. Because the finding of medial upper lid fold is common and easily corrected as part of tissue removal in a double-eyelid crease procedure through incisional approach, the myriad methods of epicanthoplasty all seem to work since the findings are quite mild and often not pathological enough to be called a true epicanthal fold.19
• Johnson20 first described the four types of epicanthus (Fig. 36-2). At the time they were described as pathological entities, although the epicanthus tarsalis in its mildest form seems to overlap with what one should consider a normal finding in Asians who have no upper lid crease, or even in those who are born with a natural crease.

Fig. 36-2 Types of epicanthus. A, Tarsalis. B, Superciliaris. C, Palpebralis. D, Inversus.
► Type 1. Epicanthus tarsalis: Fold is seen along medial upper eyelid, and covers part of the medial pretarsal region. May block view of the dermal portion of the caruncle, which is normally seen as opposed to the deeper conjunctival portion at its base.
SENIOR AUTHOR TIP: Many Asians have a medial upper lid fold without it blocking any of the medial portion of the pretarsal region, and the caruncle can still be seen. I do not consider these patients as having epicanthus tarsalis.
► Type 2. Epicanthus superciliaris: Fold originates from the brow and follows down to the lacrimal sac in an inferonasal oblique fashion, may block portion of the superonasal iris, and covers caruncle from view.
► Type 3. Epicanthus palpebralis: Bridges both upper and lower eyelids; covers the caruncle from view.
► Type 4. Epicanthus inversus: Main portion of this fold sits along medial portion of lower eyelid, and arches up superonasally to cover medial canthal angle as well as caruncle view.
• Epicanthal folds, especially the last three types, are usually seen associated with rare conditions like blepharophimosis, congenital ptosis, Down syndrome, or as an isolated finding.
SENIOR AUTHOR TIP: In patients being considered for Asian upper blepharoplasty (with construction of upper lid crease), the reduction or excision of any medial upper lid fold should be considered as part of the upper blepharoplasty, rather than labeled as a mild form of pathological epicanthus tarsalis necessitating the creation of a special “epicanthoplasty” to be added to the surgical procedure.
AESTHETICS
■ Skin evaluation
• Thickness
• Fitzpatrick classification
■ Brow relationship
• Need accurate evaluation of brow position
► Asian skin can camouflage frontalis function or activation.
► Asian blepharoplasty can be followed by “brow drop,” especially in those with borderline brow position or reflex frontalis activation.
• Evaluation of crease/brow ratio
■ Classification of crease
• Taper: Crease and pretarsal show tapers from lateral to medial.
► Nasal crease tapers to or into fold medially.
• Parallel: Crease is parallel to the lid margin along its entire course; no tapering occurs down into an epicanthal fold.
■ Determine pretarsal show
• Pretarsal show is different between whites and Asians.
• Patient decision
• Based on aesthetics
• Ideally, approximately 1-4 mm of pretarsal show13,21,22
■ Evaluate for aging eyelid and senile changes
• Upper eyelid margin is normally 1-1.5 mm below superior corneal limbus.
• Distance from central upper eyelid margin to pupillary light reflex is margin-reflex distance (MRD).
• Ptosis is present when MRD <3 mm.
• Asymmetry is present with MRD difference of ≥0.5 mm between the two upper eyelids.
■ Evaluate for crease symmetry and presence of multiple folds/creases.
PREOPERATIVE EVALUATION AND SURGICAL PLANNING
STANDARD HISTORY AND PHYSICAL EXAMINATION
■ Blepharoplasty workup
■ History of dry eyes
MARKINGS (Fig. 36-3)
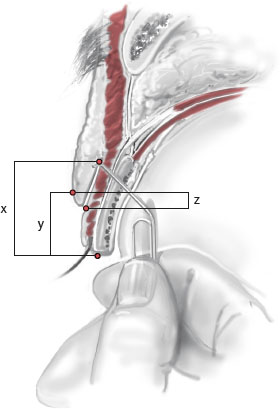
Fig. 36-3 Measure how much skin overhang to remove (z) to obtain the desired amount of visible pretarsal skin (y). Double the length of z, and add 1.5 mm for the caudal bend, depending on skin thickness, to calculate the amount of skin to be removed at that point on the lid. This exercise may be repeated at two or more points along the lid. Pretarsal height is shown (x). If a frontal lift will be performed, assess the skin in this same way, but with the measured lid’s corresponding eyebrow held at the level of “best guess” estimate of where the “postlift” brow will reside in 6 months.
■ Determine level of palpebral crease fixation.
■ Determine degree of pretarsal show and thus amount of skin resection (if needed).
■ Determine need for debulking of preaponeurotic fat.
BROWLIFT OPTIONS
■ Endobrow
■ Temporal brow
■ Coronal brow
INCISIONAL VERSUS NONINCISIONAL
■ Nonincisional technique (also known as suture, minimal incision, or closed)
• Higher incidence of relapse
• Best reserved for eyelids requiring minimal change
• Relative indications
► Patient is young with thin upper lids.
► Patient has no redundant upper lid skin or requirements for debulking.
► Patient does not want a visible scar.
• Relative contraindications
► Excessive amount or thickness of subcutaneous fat
► Dermatochalasis or excess fat and skin
■ Incisional technique
• More common technique
• Lower incidence of relapse
• Relative indications
► Need concomitant removal of skin or fat
► Thick eyelids that require debulking
• Relative contraindications
► Patient does not want a visible scar.
SENIOR AUTHOR TIP: The buried suture methods were the first to be used in the early twentieth century when understanding of anatomy was rudimentary. During the period from 1930-1960 there was greater integration of awareness of anatomy of the face and eyelids with advances in techniques that are selectively targeted. External incision methods and suture methods became more common. The great rivalry between the proponents of the two schools of Asian eyelid crease surgery fueled greater evolution of simple and complex methods in each school.
Eventually, every practitioner needs a greater understanding of the physiology and biodynamic of the complex layers of the upper lid, as well as techniques that suit his or her technical capability. It would be simplistic and foolhardy to think that the upper lid is a homogeneous layer of flesh 1.5-4.0 mm thick that can withstand indiscriminate incision and excision in external incision methods, along with multiple needle passes in buried suture methods in which permanent sutures are placed at various distances above the superior tarsal border without affecting the excursion, contractility, and function of the levator muscle and Müller muscle.
Patients are often surprised to find that after “nonincisional” methods, permanent nondissolvable suture material was placed within their upper eyelid layers, or that opening or closing their eyelids does not occur quite as naturally. They often describe a strained feeling or tightness.
EPICANTHOPLASTY
■ Clinical evaluation of epicanthal fold severity
• Mild: Fold is present without local distortion.
• Moderate: Fold extends to level of lower limbus.
• Severe: Fold extends (a) >1 mm below level of lower limbus and creates appearance of telecanthus or internal strabismus or (b) to lower lid and reflects laterally (epicanthus inversus).
• Epicanthoplasty is considered for moderate or severe epicanthal folds.
■ Indications for epicanthoplasty21
• Patient preference
► If patient desires a parallel crease, epicanthal fold will need to be addressed.
• Prominent folds that give appearance of telecanthus or strabismus
• Epicanthus inversus with fold turning laterally onto lower eyelid
• Lid crease diving beneath the epicanthal canopy
TECHNIQUE
INCISIONAL TECHNIQUES WITH LEVATOR-DERMAL FIXATION
■ Many authors have described the levator release technique.2,17,23–25
■ Basic concept
• Supratarsal incision with excision of a strip of orbicularis muscle
• Removal of excessive fat and soft tissue
• Anchoring of muscle/skin flap to the levator aponeurosis at the upper tarsal edge
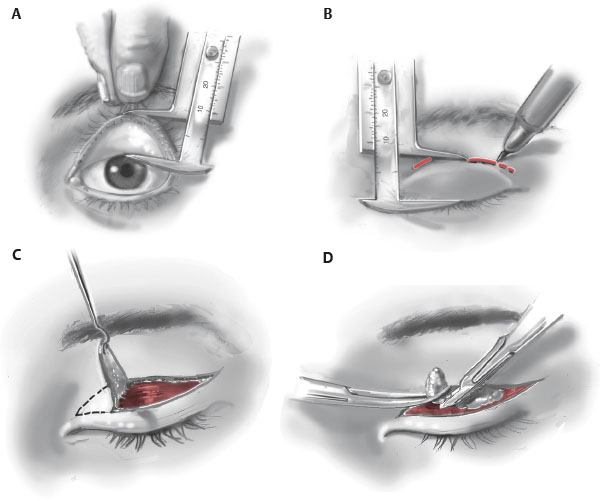
■ Technique
• Skin incision marked with fine-tipped pen (Fig. 36-4, A through D)