Arm Skin Flap for Orbital Socket Reconstruction
M. R. WEXLER
I. PELED
EDITORIAL COMMENT
This procedure, particularly in an irradiated patient, could be more easily and safely accomplished using a microvascular transfer of the radial forearm skin, with anastomosis at a site distant from the irradiated area.
Reconstruction of a contracted or missing socket, even when the eyelids are present, is a difficult problem (1). In several patients who undergo exenteration and irradiation, the socket does not exist, and in others, it cannot be stretched because of fibrosis. Young patients generally resent the idea of an external prosthesis. An upper arm flap supplies a thin piece of skin that can be used for reconstruction of both the inner lining of the eyelids and the socket lining, so that it can accommodate a prosthetic eye (2).
INDICATIONS
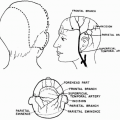
Bringing a distant flap into the orbit solves several problems. First, it lines the socket with good, durable skin that can hold a prosthesis and has no tendency to shrink. Second, the hollowness of the orbit is overcome by the introduction of the flap tissue. Third, there is the hypothetical possibility of movement if a temporalis muscle transfer can be carried out between the two layers of the reconstructed eyelids.
Although adults will generally prefer outer cosmetic prostheses, the opposite seems true in children. Although the end result is far from perfect, children seem to need the self-confidence of having restoration of the body image in order to lead more normal, active lives.
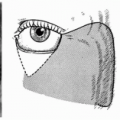
Patients who have had orbital irradiation present the problem of a contracted socket that is complicated by fibrosis, atrophy of the tarsal plate, loss of lashes, and obstructed canaliculi (3) (Fig. 31.1). The lack of tissue for intraocular prosthesis coverage, poor function of the eyelid remnants, higher susceptibility to trauma, and slower healing also escalate the risk of complications. Many patients who undergo orbital exenteration for tumor removal will have a temporalis muscle transfer for coverage of an intraocular prosthesis or for filling the hollow orbit. It seems more reasonable to preserve this precious muscle as a motor (4) in the case of diminished eyelid movement resulting from the operation, irradiation, or both. It is urged, therefore, that surgeons consider all possible alternatives before using this muscle.
FLAP DESIGN AND DIMENSIONS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree