Anterolateral Thigh Flap for Pharyngoesophageal Reconstruction
Edward I. Chang
Matthew M. Hanasono
DEFINITION
Pharyngeal defects can commonly result after resection of laryngeal malignancy or, less commonly, a pharyngeal or esophageal primary tumor.1,2
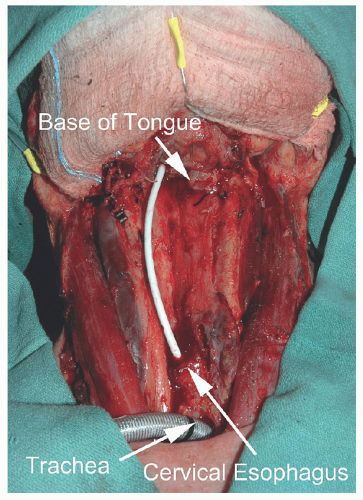
Pharyngeal defects, either partial or circumferential, can be reconstructed with anterolateral thigh (ALT) free flaps to restore swallowing and potential for voice rehabilitation (FIG 1).1,2,3,4,5
Given the high incidence of preoperative radiation in this patient population, reconstruction of the pharyngeal defect using a free flap should also facilitate simultaneous neck wound reconstruction if necessary.
Complications following pharyngeal reconstruction must be considered and include flap loss, infection, fistula, stricture, and neck wound dehiscence.
ANATOMY
The arterial supply to the ALT flap is derived from branches of the lateral descending circumflex femoral artery arising from the profunda femoris artery.
The lateral descending circumflex vessels are located between the rectus femoris and vastus lateralis muscles and have a variable intramuscular course.
The ALT flap can be harvested as a perforator-based fasciocutaneous flap, a myocutaneous flap including some or all of the vastus lateralis muscle, or as a chimeric flap by including portions of the vastus lateralis muscle supplied by a separate branch of the main pedicle.
One or more perforators are usually found along an imaginary line connecting the anterior superior iliac spine (ASIS) to the lateral patella.
The perforators are typically located at the midpoint of this line and 5 cm proximally and distally, the so-called A, B, and C perforators named in a proximal to distal orientation.9
The perforators typically arise from the main pedicle and can pass through the vastus lateralis muscle (musculocutaneous) or pass through the septum between the vastus lateralis and rectus femoris (septocutaneous).
Occasionally, the perforators may originate from either the transverse branch or an oblique branch of the lateral circumflex artery.
If multiple perforators are present, the flap can be divided into separate skin paddles to reconstruct the primary pharyngeal defect and to resurface the neck.
PATIENT HISTORY AND PHYSICAL FINDINGS
The quality of the neck skin and soft tissues should be carefully examined to determine the need for external coverage following tumor resection and reconstruction.
This is particularly important in patients with a prior history of surgery and/or radiation.
Neck dissection and severe radiation fibrosis may limit the availability of recipient blood vessels.
In addition, many patients with head and neck cancer and those with a history of prior neck radiation have carotid vascular disease further challenging reconstruction in this setting. In these cases, preoperative imaging may be useful in select cases, and reconstructive surgeons should be prepared to use alternate recipient vessels with or without vein grafting. Patients should be counseled of this possibility as well as the potential for additional surgical incisions for recipient vessel exposure.
The donor site should be examined also for prior surgical scars as well as the thickness of the soft tissue.
Patients with excessive adipose tissue thickness in the thighs may not be good candidates for an ALT flap. In obese patients with thick thigh tissue, reconstruction of a circumferential defect is best performed with a jejunum flap or a thinner flap that can be tubed more easily.
Harvesting the flap and sacrificing the lateral descending circumflex femoral artery have not been found to exacerbate
peripheral vascular disease or precipitate limb ischemia; however, signs of vascular insufficiency should alert the surgeon to potentially calcified vessels that may make the microvascular anastomosis more challenging.
IMAGING
Head and neck computed tomography (CT) with intravascular contrast is critical for evaluating the extent of the disease and planning the resection.
The preoperative imaging can often decipher whether partial pharyngectomy will be performed or whether a segment involving the entire circumference of the pharynx will be resected.
CT angiography can also guide recipient vessel selection. In the previously operated and/or irradiated neck, identification of alternate recipient vessels such as the transverse cervical vessels may be necessary.3,10
In certain circumstances, even more distant recipient vessels, such as the internal mammary vessels, are needed.
No specific imaging studies are needed for the donor site. Although a CT angiogram can be performed in anticipation that a second skin paddle is needed, we do not routinely obtain them.
SURGICAL MANAGEMENT
Preoperative Planning
Optimizing the patient to undergo a lengthy operation is critical and includes adequate nutrition via tube feeding, if necessary because many patients may have had difficulty swallowing and subsequent weight loss.
Smoking cessation should be encouraged although, realistically, this is challenging to achieve in a short period of time.
Preoperative consultation and medical clearance are also important in at-risk patients.
Many patients with head and neck malignancies have a history of smoking and alcohol use and are therefore at risk for cardiovascular or hepatic complications.
Preoperative imaging and optimization of cardiac function are important to prevent postoperative medical complications.
Positioning
The patient is prepped in the supine position with the neck extended to facilitate neck dissection and recipient vessel exposure.
The bed is typically turned 180 degrees with the foot of the bed facing the anesthetist, allowing the surgical teams complete access to the head and neck region.
Both thighs should be prepped into the field to access harvesting the flap from either thigh.
This is because in a small percentage of cases, there is a paucity of skin perforators in one thigh, in which case the other thigh can be used instead.
The entire head and neck as well as the chest to the level of the xiphoid should also be prepped into the field, in case a pectoralis major myocutaneous flap is needed for neck wound coverage.
Approach
The approach to reconstructing a pharyngeal defect should also take into account alternate flaps to reconstruct the defect.
In general, free tissue transfer results in the most optimal outcomes, and other flaps such as the radial or ulnar forearm flap are also useful for partial pharyngectomy defects when the thigh flap is not available or in obese patients with thick thigh tissues.
The lateral arm flap as well as other thigh-based flaps such as the profunda artery perforator (PAP) flap may also be good options.
Our preference is to reconstruct circumferential defects with a thigh-based flap whenever possible; however, a free jejunal flap can also be considered.11
In patients who are not candidates for a free tissue transfer (ie, major comorbidities that preclude a long operation or lack of recipient vessels), pedicled flaps such as the pectoralis major myocutaneous flap, supraclavicular flap, or an internal mammary artery perforator flap can be considered.1
TECHNIQUES
ALT Flap Harvest
The ASIS and lateral patella are marked, and a line is drawn connecting these two points.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree