CHAPTER 27 Anesthesia for Hip Surgery
GENERAL ANESTHESIA
General anesthesia allows for anesthesia, analgesia, akinesis, amnesia, and autonomic stability. Traditionally, it has been viewed by some as the “gold standard” for anesthesia for major hip procedures.1 General anesthesia can be induced and maintained either intravenously or by inhalation with a variety of compounds. In adults, the induction of general anesthesia is most typically performed by the intravenous administration of a barbiturate (e.g., sodium pentothal or methohexital) or a nonbarbiturate (e.g., propofol, etomidate, ketamine). The selection of an induction agent is often determined by the patient’s comorbidities and other parameters such as hemodynamics and intravascular volume status. In pediatric procedures or when adults are without intravenous access, general anesthesia can be induced by inhalation of a volatile anesthetic gas, but this is a slower process compared with intravenous induction. Many adults find this an unpleasant experience, and it may introduce unacceptable anesthetic risk in some patients.
Because medication is continuously administered in some form during the course of general anesthesia, the anesthesiologist is able to constantly adjust the depth of anesthesia to changing patient or surgical conditions and to better adapt to shorter or longer than anticipated durations of surgery. The relative risks of general anesthesia and its effect on the incidence of complications are discussed later. However, general anesthesia is unique from the other anesthetic modalities for major hip procedures in its need for definitive airway management and the unique risk of malignant hyperthermia, which is a rare but potentially life-threatening reaction to volatile anesthetic gases and depolarizing neuromuscular blockers. The incidence of malignant hyperthermia susceptibility is believed to be about 1 in 15,000 in pediatric populations and 1 in 50,000 among adults.2 Various forms of muscular dystrophy predispose to malignant hyperthermia, and the majority of individuals displaying this abnormal response to anesthesia have inheritable mutations of the skeletal muscle ryanodine type I receptor.3
NEURAXIAL ANESTHESIA
Neuraxial or major conductive anesthesia involves the injection of preservative-free local anesthetic (e.g., lidocaine, bupivacaine, tetracaine) and possibly an opioid into the intrathecal or epidural spaces. With a dense block, either technique can provide anesthesia without unconsciousness and also akinesis and muscle relaxation. Failure to achieve a dense block can occur with either technique, but inadequate block or muscle relaxation occurs more commonly with epidural anesthesia. Neuraxial block is often associated with hypotension, because venous pooling occurs, decreasing cardiac preload. Judicious use of vasopressors and hydration is usually effective in correcting significant hypotensive events. In addition, modest hypotension may be preferred by some surgeons as a method of reducing blood loss. If sedation or amnesia is desired, conscious sedation can be given as well. Each technique can be by either single injection or continuous infusion. Continuous techniques provide the benefit of controlled initial titration followed by continuation into the postoperative period to provide analgesia. Continuous spinal anesthetics are relatively uncommon in the United States because intrathecal catheters were withdrawn from the practice in 1992 by the U.S. Food and Drug Administration (FDA). However, in Europe, continuous spinal techniques have been shown to result in less overall hypotension (including profound hypotension) compared with single-injection spinal anesthetics among patients older than the age of 65 years undergoing operative repair of hip fracture.4 This is in part due to differences in dosing requirements between the two techniques. The ED50/ED95 of isobaric bupivacaine for total hip arthroplasty when administered in incremental fashion during continuous spinal anesthesia is substantially lower than the doses typically administered during single-injection techniques.5 Most clinicians will administer intravenous crystalloid or colloid before spinal anesthesia to limit the degree of hypotension.
Dextrose is commonly added to local anesthetic to increase the baricity. Hyperbaric solutions will tend to settle by gravity in the cerebrospinal fluid, hypobaric solutions will tend to rise, whereas isobaric solutions should migrate from the level of injection only minimally. In this manner, the spinal block can be made denser on one side of the patient than the other. A hyperbaric spinal block can be administered with the patient in the lateral decubitus position with the operative hip dependent; conversely, a hypobaric spinal block can be administered for similar effect with the operative hip up. When spinal anesthesia is injected with the patient in the lateral decubitus position with the operative hip up before total hip arthroplasty, the same dose of bupivacaine results in a block of longer duration with a delayed need for analgesics in the postoperative period if the injectate is delivered in a hypobaric, as opposed to an isobaric, suspension.6 Small quantities of opioid can be added to improve analgesia, but they must be utilized judiciously because of possible resulting pruritus, nausea, and ventilatory depression. Adding intrathecal morphine to the spinal anesthetic has been shown to reduce the need for patient-controlled analgesia with morphine after the procedure for total hip arthroplasty patients, a benefit that was not observed among total knee arthroplasty patients.7 In a series of 60 patients older than the age of 65 years undergoing elective total hip arthroplasty, 50 µg of intrathecal morphine added to hyperbaric bupivacaine failed to improve postoperative analgesia compared with placebo whereas 100 µg and 200 µg improved analgesia equally well, with the 200-µg dose being associated with significantly more postoperative pruritus.8
For major hip procedures, a lumbar epidural anesthetic is sufficient. Unlike spinal anesthesia, baricity of the injectate does not affect distribution. The key determinants of the block include the dose of local anesthetic and the volume in which it is delivered. Distribution of the anesthetic within the epidural space is less predictable than in the intrathecal space, and epidural blocks can be patchy or unilateral. Although technically more difficult with slightly less reliability than spinal anesthetics, epidural anesthesia offers the distinct advantage of an indwelling epidural catheter to deliver postoperative analgesia. Postoperative epidural analgesia, in all its various forms, has been demonstrated in large meta-analyses to supply superior analgesia to either parenteral opioids9 or more specifically parenteral opioids delivered in patient-controlled analgesic fashion.10
PRE-EMPTIVE ANALGESIA AND POSTOPERATIVE PAIN
A proper anesthetic plan needs to address the postoperative analgesic needs of the patient. Pre-emptive analgesia utilizes analgesics before painful stimuli to prevent central stimulation and thus lessen the subsequent pain experience. Local anesthetics utilized in peripheral nerve blocks or neuraxial anesthesia are an integral part of the multimodal approach to pre-emptive analgesia.11 Total hip arthroplasty patients receiving spinal anesthesia report lower pain scores and require less analgesic medication in the postanesthesia care unit and, as an added benefit, spinal anesthesia can be delivered more cost effectively than general anesthesia for this procedure.12 Combined spinal and epidural techniques have been used for major hip procedures, taking advantage of spinal anesthesia’s rapid and reliable onset and ability to deliver sustained postoperative analgesia through an epidural catheter. Although efficacious, traditional epidural analgesia introduces additional sources of complications and expense into the postoperative management of surgical patients. Problems with epidural catheters (e.g., kinking, occlusion, or catheter migration) or the infusion pumps (e.g., misprogramming or battery or electrical failure) are common and can lead to periods of disruption of analgesia therapy. Trained personnel need to be available to troubleshoot these problems, and indwelling epidural catheters may increase the risk of neuraxial hematoma formation when postoperative anticoagulation is used.
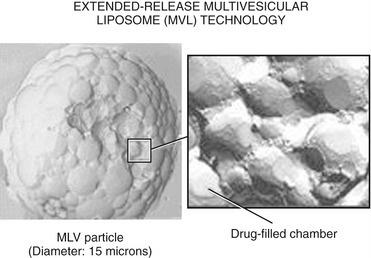
The duration of effective analgesia provided by preservative-free morphine injected into the epidural space is 24 hours or less. An extended-release epidural morphine (Depodur, Endo Pharmaceuticals, Inc, Chadds Ford, PA) preparation is currently available that delivers 48 hours of postoperative analgesia. Therefore, it is now possible to provide a combined spinal and epidural technique for hip surgery that provides extended postoperative analgesia without an indwelling epidural catheter. Depodur utilizes a multivesicular liposomal delivery system called DepoFoam (SkyPharma, Inc, San Diego, CA). DepoFoam consists of microscopic lipid-based particles with numerous morphine-containing internal vesicles that reorganize after injection into the epidural space causing the sustained release of morphine at a predictable rate. Depodur has been demonstrated to provide analgesia superior to patient-controlled analgesia with fentanyl alone both at rest and with activity to patients undergoing total hip arthroplasty without causing motor block or requiring an epidural catheter.13 Some patients receiving Depodur require little or no parenteral opioids postoperatively. A sustained-released formulation of epidural bupivacaine using DepoFoam technology is being developed (Fig. 27-1).
LUMBAR PLEXUS BLOCKADE
Lumbar plexus blockade achieves anesthesia in the distribution of the femoral, obturator, and lateral cutaneous nerves. A number of approaches to the lumbar plexus have been developed that utilize anatomic landmarks and an insulated stimulating needle to precisely locate the nerves. Blockade can be achieved with a single injection of local anesthetic, or a catheter can be placed for continuous infusion. Lumbar plexus blockade can be an effective modality of analgesia after total hip arthroplasty. If anesthesia of the posterior thigh is desired, the sciatic nerve must be blocked separately. When combined with a sciatic nerve block, lumbar plexus blockade can be used as the sole anesthetic for hip fracture surgery.14 The muscle relaxation achieved is generally inferior to that of other anesthetic modalities, and lumbar plexus blockade is generally reserved for postoperative analgesia. For analgesia in total hip arthroplasty, the block can be placed postoperatively after neurologic assessment of the operative leg has been achieved. By continuous infusion, analgesia has been maintained for up to 48 hours,15 or it can be placed before the procedure for its pre-emptive analgesia value, reducing both intraoperative and postoperative opioid requirements.16 Retroperitoneal hematoma from attempted lumbar plexus blockade has been reported in patients receiving anticoagulation after surgery.17
ANESTHETIC CONTRAINDICATIONS
There are no absolute contraindications to general anesthesia. Patients with a history of malignant hyperthermia require avoidance of triggering agents and total intravenous anesthesia. Unless prohibited by surgical urgency, patients with increased but reducible perioperative risk should be medically optimized preoperatively to minimize risk. Neuraxial anesthesia is contraindicated by infection at the site of needle insertion, thrombocytopenia, systemic anticoagulation or uncorrectable coagulopathy, sepsis, severe valvular cardiac disease (particularly aortic stenosis), and patient refusal. Prior spine surgery is not an absolute contraindication but may render the procedure technically difficult or impossible. Historically, preexisting neurologic disease has been considered a relative contraindication to neuraxial anesthesia, but at least one recent study has disputed this assumption.18