4 Surgery and anesthesia are uniquely interdependent. Each discipline cannot exist without the other. Improvements by each interact for the benefit of the patient, while the potential complications of each can negatively impact the patient. Surgeons and anesthesia professionals must cooperate and communicate to maximize patient safety through minimizing the likelihood of complications. In hospital settings, anesthesia is administered by personnel trained in anesthesia: a physician anesthesiologist, a nurse anesthetist, an anesthesia assistant, or a team of an anesthesiologist with either of the other two. However, this is not always the case in the setting of sedation and analgesia, particularly outside traditional hospital operating rooms. The surgeon will then have a role in supervising the care given by the individual administering the sedation. In some states, the surgeon will also supervise the nurse anesthetist if an anesthesiologist is not involved in the case. Regardless of the array of practitioners, proper avoidance and management of complications requires input from all participants. Understanding, appreciation, and anticipation of risks help to prevent untoward outcomes. Anesthesia complications are any adverse, undesired outcomes related to anesthesia care. As with all complications of medical care, the primary focus should be on prevention. Sometimes these outcomes cause direct morbidity or mortality to the patient. At other times, they affect the patient indirectly by impeding the surgical procedure, such as intraoperative hypertension that leads to excessive bleeding or inadequate relaxation leading to patient movement at a critical delicate point in the operation. Over all, anesthesia care is remarkably safe. Due to the lack of centralized statistics and consistent definitions, it is very difficult to determine an exact mortality rate related solely to anesthesia. However, the risk of anesthesia catastrophe (death, permanent brain damage, or intraoperative cardiac arrest) in healthy patients is vanishingly small, in the range of 1:150,000 to 1:300,000.1 When these catastrophes do occur, they usually involve the coincidence of two or more deviations from normal circumstances at the same time and often include unrecognized inadequate ventilation (from any of several causes—including simple inattention), failures of the oxygen supply, or, rarely, other equipment failures. This is not to say that other critical incidents (such as disconnection of the breathing circuit) are rare. These still occur with some frequency, but they usually do not cause adverse outcomes because the behaviors of the anesthesia professional, augmented by the alarms and warning signals from the safety monitoring equipment, catch such developments very early in the evolution of an event, allowing correct diagnosis and treatment long before there is any real danger to the patient. Insight about adverse outcomes unique to anesthesiology can be found from the American Society of Anesthesiologists Closed Claims Project. Starting in 1984, many medical malpractice insurance companies were persuaded to open their closed files and allow confidential examination of the litigation records. All these cases, by definition, involved adverse anesthesia outcomes. They were examined for patterns of causes and effects regarding untoward clinical events, which were usually severe and involved at least perceived damage that led to lawsuits against anesthesiologists. A summary of the positive impact of the project during its first 17 years2 reveals the extensive breadth of the findings. One important initial finding was that “respiratory system adverse events” accounted for a significant fraction of the claims, particularly lawsuits involving death or brain damage.3 The main focus of the study was not on the concept of preoperative predictors of adverse anesthesia outcome as much as it was on the causation of the adverse events. It was determined that failure to monitor adequately was the main reason for the adverse outcomes and that 93% of the preventable mishaps would have been avoided by the correct application of capnography and pulse oximetry together to help ensure appropriate ventilation and oxygenation.4 Traditional potential adverse outcomes that are caused largely by anesthesia care and manifest within 24 to 48 hours of surgery are listed in Table 4.1. Some authors might add severe bronchospasm, or airway burns, to this list of anesthesia complications. The practice of anesthesiology intimately involves the use of medications. An unfortunate reality is that most medications have some degree of side effect, adverse reactions, and unwanted interaction with other medications. One significant implication is that it is very important to understand and fully evaluate the patient’s chronic medications because of the possibility of interactions with anesthetic medications. Table 4.1 Traditional Potential Adverse Outcomes of Anesthesia Care
Anesthesia Complications in Facial Plastic Surgery
 Outcome of Anesthesia Care
Outcome of Anesthesia Care
 Complications of Anesthetic Medications
Complications of Anesthetic Medications
Broken teeth from laryngoscopy |
Corneal abrasion |
Allergy to anesthetic medications |
Unintended awareness during general anesthesia |
Unplanned admission to the hospital following outpatient surgery |
Unplanned postoperative admission to an intensive care unit |
Pneumonitis from aspiration of acid stomach contents |
Emergency reintubation in the immediate postop period |
Peripheral nerve injury |
Neuraxial nerve injury, including stroke, with deficit |
Unanticipated pulmonary edema |
Malignant hyperthermia |
Hypoxic brain injury |
Myocardial infarction |
Cardiac arrest |
Death |
Premedication Prior to Surgery
Most premedications given today are anxiolytics, analgesics, antiemetics, or medicines for prophylaxis against aspiration of stomach contents. Anxiolytics (such as midazolam) and especially narcotics (such as fentanyl) may lead to depression of consciousness or ventilation, which can lead to patient harm if it is not anticipated and recognized quickly. Monitoring of hemoglobin saturation with oxygen using pulse oximetry may help to detect problems, but hemoglobin desaturation is a late development in the downward spiral from excessive depressant medication, so direct visual monitoring by personnel trained to detect hypoventilation (whether from airway obstruction, CNS depression, or both) is likely to be more helpful. Patients are at higher risk for ventilatory depression if they take either anxiolytics or narcotics chronically at home, because there can be an additive effect with similar medications that may be given on the day of surgery. Extreme caution and hypervigilance should be exercised in this situation.
Metoclopramide is sometimes given for both antiemesis and (because it is a pro-motility agent intended to help empty the stomach) aspiration prophylaxis. Because it blocks post-synaptic dopaminergic receptors, dystonic and other extrapyramidal reactions can be seen, though occurring in less than 1% of patients.5 Patients may also experience feelings of anxiety and agitation, which occur more often when the drug is administered as a rapid IV bolus as opposed to the recommended slow infusion. Such adverse reactions can typically be treated with diphenhydramine (25 or 50 mg, IV) or benztropine. Other agents that have found some success in reducing postoperative nausea and vomiting (PONV) include ondansetron, aprepitant, and Decadron.
Aspiration of acid stomach contents can be one of the most serious complications of anesthesia care. A true acid aspiration pneumonitis carries significant morbidity and an appreciable mortality. Accordingly, it is critical that patients observe the prescribed pre-op NPO regime, the recommended precise details of which are debated and are evolving.6,7 Many efforts can be made to help minimize aspiration risks. Patients with known gastroesophageal reflux disease (GERD) and/or hiatus hernia, or even with a tendency to frequent “heartburn,” may benefit from an attempt at reduced preoperative stomach acid production with either an H-2 blocker (such as famotidine) or a proton pump inhibitor (such as omeprazole), metoclopromide as noted to promote gastric emptying, and PO sodium citrate (Bicitra) to neutralize any remaining stomach acid. Such a regime may apply equally or even more so to patients scheduled for sedation and analgesia who will not have a secured airway but who may become relaxed or nauseated enough to regurgitate residual stomach contents. The gravity of the potential complications is so great that this question must be considered for every patient.
Local Anesthetic Toxicity and Allergy
Local anesthetics are drugs that produce reversible blockade of the conduction of impulses along central and peripheral nerve pathways by inhibiting passage of sodium ions through ion-selective sodium channels in nerve membranes. Removal of the local anesthetic by redistribution or metabolism is followed by spontaneous and complete return of nerve conduction with no evidence of structural damage to nerve fibers.8 Thus, wary patients may be reassured that local anesthetics do not cause permanent dysesthesia.
Systemic toxicity from a local anesthetic occurs when there is an excess plasma concentration of the drug that may manifest in the central nervous system or cardiovascular system. Accidental direct intravascular injection is the most common mechanism for producing such an excess plasma concentration. Less often, excess plasma concentration results from absorption of significant amounts of the local anesthetic from the injection site.
Central Nervous System Toxicity
Nervous system toxicity manifests in a continuum, depending on the plasma concentration of local anesthetic. The initial symptoms of local anesthetic toxicity usually include numbness of the tongue and circumoral tissues. As the plasma concentration increases, restlessness, vertigo, and tinnitus may result from the local anesthetic crossing the blood-brain barrier. Very high plasma concentrations produce tonic-clonic seizures.
Treatment of local anesthetic-induced seizures consists of ventilation with supplemental oxygen and, if indicated, IV benzodiazepines (midazolam or diazepam). Hyperventilation lowers the PaCO2, which decreases cerebral blood flow, thus resulting in a decreased delivery of drug to the brain. This maneuver may be helpful in reducing the plasma concentration in the face of a seizure. Refractory seizures may require induction of general anesthesia with a barbiturate.
Cardiovascular Toxicity
The reversible blockade of sodium channels from local anesthetics can also block sodium channels in the heart, which can lead to cardiac toxicity. Myocardial conduction and automaticity may become depressed when enough of these channels become blocked. Increases in local anesthetic blood levels may lead to varying degrees of heart block, the appearance of multi-focal ectopic beats, re-entrant arrhythmias, tachycardia, and, ultimately, ventricular fibrillation. Treatment is supportive and includes oxygen, vasopressors, inotropes, and anti-dysrhythmics if needed.9 Evidence is building that infusing a 20% lipid emulsion may be helpful when there is cardiac arrest due to bupivacaine toxicity.10
Among local anesthetics, there appears to be a difference in their propensity to cause cardiac toxicity. Experience has shown that bupivicaine (Marcaine) toxicity is the most likely to lead to cardiovascular collapse, which is particularly difficult to treat. This finding led to the search for a safer long-acting local anesthetic.11 Analysis of laboratory data suggests that cardiac toxicity is associated with the dextro (R-) enantiomer of bupivacaine and that the S-enantiomer is less troublesome. Ropivacaine, which was released for use in 1996, is a pure S-isomer that has less cardiotoxicity than bupivacaine. It is more expensive than bupivacaine, but when large volumes of local anesthetic are used with a high likelihood of intravascular injection or significant absorption, its greater safety justifies the increased cost.12
Maximum Dose of Local Anesthetics
Even when local anesthetics are administered by infiltration into soft tissues, some is absorbed into the bloodstream, and this absorption can, in excess quantity, be toxic. Table 4.2 shows maximum recommended infiltration doses of various local anesthetics.13
Local Anesthetic Allergy
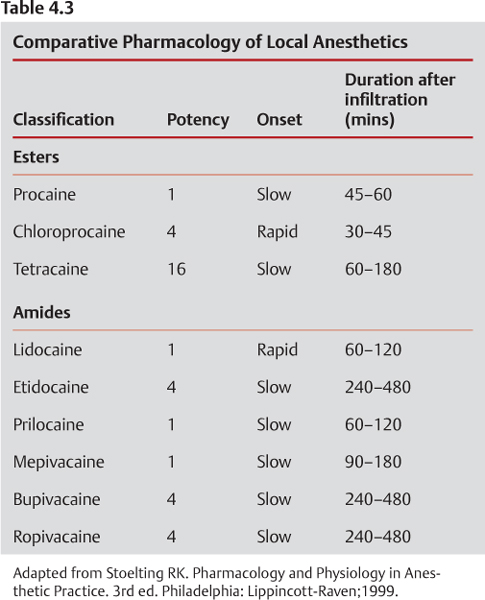
Patients occasionally report “allergy” to local anesthetic agents, but true allergy to local anesthetics is quite rare. Ester local anesthetics, which produce metabolites related to para-aminobenzoic acid (PABA), are significantly more likely to lead to allergic reactions than amide local anesthetics, which do not produce these metabolites.8 Table 4.3 shows the ester and amide classification of local anesthetics, as well as other items of comparative pharmacology. Because PABA is usually the culprit in true allergy, there is often cross-sensitivity within the ester classification. (For example, a patient allergic to tetracaine will also likely have an allergic reaction to procaine.)
Table 4.2 Clinical Properties of Local Anesthetic Agents
Local Anesthetic Agent | Duration of Action (h) | Maximum Safe Dosage (mg/kg) |
Lidocaine (plain) | 1.5–2 | 4 |
Lidocaine (with epinephrine) | 2–2.5 | 7 |
Bupivacaine (plain) | 3–6 | 1–2 |
Bupivacaine (with epinephrine) | 6–10 | 2–3 |
Mepivacaine | 2.5–3 | 7 |
Ropivacaine | 6–10 | 1–2.5 |
Tetracaine | 1–3 | 1–2 |
Cocaine | 0.75–3 | 3–4 |
Adapted from Ahlstrom KK, Frodel JL. Local Anesthetics for Facial Plastic Procedures. Otolaryngologic Clinics of North America; 2002;35(1):29–53.
Another common reason for “allergy” to local anesthetics is a normal response to epinephrine. Epinephrine is often added to local anesthetics to provide vasoconstriction, which slows the systemic absorption of the local anesthetic and therefore prolongs the action of the drug. Intravascular absorption of epinephrine can lead to tachycardia, palpitations, flushing, and hypertension, all of which the patient may incorrectly interpret as an allergic reaction, usually during dental work. Therefore, when a patient reports a drug allergy, it is important to obtain a detailed history in an attempt to determine exactly what took place during the incident and guide subsequent therapy accordingly. It is extremely unlikely that a patient is truly allergic to an amide local anesthetic. If the reaction did not include any rash, hives, swelling, or bronchospasm but does describe a typical response to epinephrine, it may be reasonable simply to proceed slowly with an amide local anesthetic (knowing that appropriate anaphylaxis treatment is available, as it always must be for every case). On the other hand, if there is genuine doubt, it is reasonable to postpone any use of local anesthetic and refer the patient to an allergist for testing.
Intravenous Sedation
Sedation is typically produced through the use of any number of intravenous medications, either alone or in combination. The classic combination is a benzodiazepine, such as midazolam, and a narcotic, such as fentanyl (which has replaced meperidine in many practices because repeated doses of meperidine are associated with the potential for seizures). Though midazolam is used commonly as the benzodiazepine of choice, several different narcotics are often used, including the ultra-potent synthetic narcotics fentanyl and remifentanil. In the past 20 years, the hypnotic drug propofol has been introduced into practice, either alone or in combination with other medications. Ketamine, a dissociative hypnotic drug, has also been used as a non-narcotic sedative.
The desired effect of IV sedation varies with the particular situation, and this drives the choice of drugs. Benzodiazepines produce anxiolysis and amnesia, but no analgesia and relatively little ventilatory or cardiovascular depression in truly conservative doses. Narcotics are analgesics that cause respiratory and cardiovascular depression, but only small amounts of anxiolysis and no appreciable amnesia. Propofol has very little analgesic effect, but produces anxiolysis and unconsciousness. Therefore, if the patient is having a procedure where excellent analgesia can reliably be achieved with local anesthesia but the patient is anxious, then sedation with only a benzodiazepine would be adequate and a narcotic would be unnecessary.
The definition of therapeutic index is the ratio between the toxic dose and the effective therapeutic dose of a drug, and it is used as a measure of the relative safety of the drug. Drugs with a small, or narrow, therapeutic index have a very little difference between the plasma concentrations that produce the desired effect and toxicity. The same concept can be applied in situations when the concern is not overt toxicity, but undesired side effects. This is the case with medications used for IV sedation. Many of these drugs, most notably propofol and remifentanil, have a very narrow therapeutic index related to ventilatory depression. This requires that these specific medications be titrated very carefully and that patients are monitored very closely for adequate ventilation and oxygenation.
Propofol is an extreme example of this quandary because the same drug can produce both excellent conscious sedation and deep general anesthesia with an electrically silent EEG, just by varying the dose. The availability and use of this drug by non-anesthesiologists was one of the primary motivators for the American Society of Anesthesiologists to produce practice guidelines for sedation and analgesia for non-anesthesiologists.14 This document reviews the continuum between minimal sedation, moderate sedation, deep sedation, and general anesthesia and provides definitions. Recommendations in the guidelines include items related to patient preparation, patient monitoring, training of personnel, availability of emergency equipment, use of supplemental oxygen, titration of medications, and recovery care. Facial plastic surgeons directing the administration of propofol for sedation should review and actively apply these guidelines.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree