13. Anatomy, Physiology, and Disorders of the Skin
Thornwell H. Parker III, Molly Burns Austin, Alton Jay Burns
ANATOMY1 (Fig. 13-1)
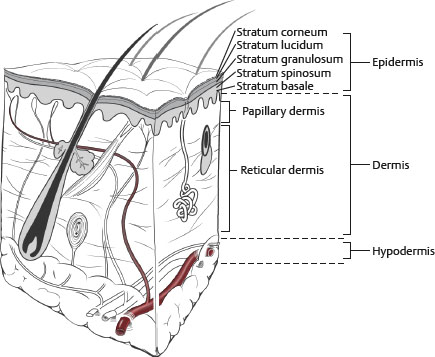
Fig. 13-1 Layers of the skin with adnexal structures.
EPIDERMIS
■ The epidermis comprises the following cells:
• Keratinocytes: 80% of epidermis
• Melanocytes: Mostly within basal layer, pigment-producing cell, pigment provides UV protection
• Merkel cells: Mostly within basal layer, mechanoreceptor, slow-adapting
• Langerhans cells: Antigen-presenting/T-cell activating cells of the epidermis
■ The epidermis has five layers, each approximately 100 μm thick:
• Stratum basale: Mitotically active layer providing cells for upper layer differentiation
• Stratum spinosum: Spinelike appearance of cell margins from intercellular bridging
• Stratum granulosum: Intracellular granules containing materials to create skin barrier
• Stratum lucidum: Clear layer of dead cells devoid of nuclei, prominent in palms/soles
• Stratum corneum: Cornified layer of cells following programmed cell death of the granular layer, providing skin barrier
DERMIS
■ Makes up most of skin
■ Responsible for the strength, elasticity, and pliability of the skin
■ Composed of primarily collagen (type I/III ratio 4:1) and elastic fibers
■ Maintained by fibroblasts
■ Also inhabited by macrophages and mast cells
■ The dermis has two layers:
• Papillary dermis: Superficial, similar thickness to epidermis, approximately 100 μm (thickness of all layers varies by location)
• Reticular dermis: Deep, makes up most of dermis (2000–2500 μm). Collagen and elastic fibers are thicker and more organized in deeper dermis.
VASCULATURE
■ Small vessels penetrate from the subcutaneous tissue and form a horizontal vascular plexus within the deep reticular dermis.
■ Arterioles extend vertically from the plexus toward the epidermis, forming the subpapillary plexus at the interface of the papillary and reticular dermis.
■ Individual capillary loops then extend from these end arterioles up into each papilla of the papillary dermis.
LYMPH
■ Lymph vessels are important to regulating interstitial fluid balance, collecting degraded substances, and sampling for immune function
NERVES
■ Nerves follow a distribution and pattern similar to those of the vasculature, with a deep reticular and subpapillary plexus.
SKIN APPENDAGES
■ Hair follicles, growth cycle variable by location
• Anagen: Growth phase, 2 years
• Catagen: Programmed cell death, hair loss, 2 weeks
• Telogen: No hair, no growth, 2 months
GLANDS
■ Sebaceous glands, eccrine glands, apocrine glands
■ Maintain skin hydration and assist with thermal regulation
■ Provide source for epidermal regeneration?increased density on face allows resurfacing procedures, but below the jawline, reduced density delays epidermal regeneration, and can lead to scarring
■ Affected by retinoids (impaired by isotretinoin, which reduces sebaceous units)
SKIN PHYSIOLOGY
NORMAL SKIN FUNCTION
■ Thermal: Provides insulation and regulation through blood flow and eccrine secretions
■ Mechanical and chemical: Protection against injury, infection, and water loss
■ Metabolism: Vitamin D conversion
■ Sensation: Sensation, temperature, pressure, and vibration
■ Aesthetics
NORMAL SKIN AGING (Fig. 13-2)
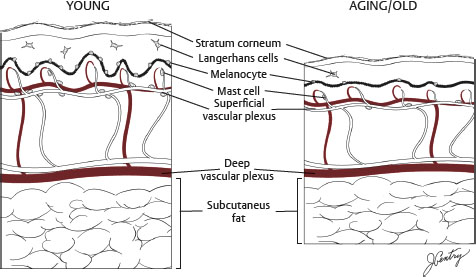
Fig. 13-2 Histology of aging skin. Aging skin is shown on the right.
HISTOLOGY
■ Thinning of epidermis
■ Flattening of the rete ridges
■ Thinning and degeneration of the dermis, collagen, and elastic fibers (solar elastosis)
■ Atrophy of subcutaneous tissue
CLINICAL PICTURE
■ Thinning skin
■ Lost elasticity
■ Facial laxity
■ Facial rhytids
■ Loss of facial volume
WOUND HEALING2,3
■ Inflammation (days 1 to 6)
• Vasoconstriction ➤ coagulation ➤ vasodilation/capillary leak ➤ chemotaxis ➤ cell migration
• Neutrophils ➤ macrophages ➤ lymphocytes
► Macrophage most important to regulate growth factors and wound healing
■ Proliferation (day 4 to week 3)
• Fibroblasts predominate, increased collagen synthesis, and angiogenesis
■ Maturation (week 3 to 1 year)
• Equilibrium between collagen deposition and breakdown
• Increased collagen organization and stronger cross-links
• Type I collagen replaces type III to restore 4:1 ratio
• Healing strength begins to plateau at approximately 60 days at 80% original strength.
■ Reepithelialization
• Mobilization: Loss of contact inhibition occurs for cells at edge of wound.
• Migration: Cells migrate across wound until they meet cells from other side.
• Mitosis: As edge cells migrate, cells farther back proliferate to support migration.
■ Contraction
• Myofibroblasts (specialized fibroblasts) appear by day 3 and are maximal by day 10 to 21, with greater numbers and contraction in full thickness/deeper wounds.
FACTORS AFFECTING WOUND HEALING
GENETIC SKIN DISORDERS
■ Cutis laxa
• Nonfunctioning elastase inhibitor leads to elastic fiber degeneration.
• Skin has coarse texture, droops over all of body, and is diagnosed during neonatal or early childhood.
• Congestive heart disease, emphysema, pneumothorax, aneurysms, and hernias may also occur.
• It slowly worsens over time, but surgical correction can be beneficial.
■ Pseudoxanthoma elasticum
• Similarities to cutis laxa, with loose skin secondary to elastic fiber degeneration
• May also benefit from surgery
■ Ehlers-Danlos
• Disorder of collagen cross-linking
• Leads to fragile, hyperelastic skin, hypermobile joints, and aortic aneurysms
• Surgery contraindicated because poor wound healing
■ Elastoderma
• Poorly understood cause
• Pendulous skin over trunk and extremities, eventually entire body
• Surgery contraindicated
■ Progeria (also known as Hutchinson-Gilford syndrome)
• Rapid progression and short lifespan, from childhood
• Laxity and irregular skin contouring, craniofacial malformations, cardiac disease, ear abnormalities, and poor wound healing
• Surgery contraindicated, poor wound healing
COMORBIDITIES
■ Diabetes
■ Atherosclerotic disease
■ Renal failure
■ Immunodeficiency
NUTRITIONAL DEFICIENCIES
■ Vitamins and minerals (vitamin C, zinc, iron)
■ Caloric
■ Protein (check albumin, prealbumin, transferrin, and haptoglobin)
DRUGS
■ Smoking: Vasoconstriction and decreased oxygen delivery
■ Steroids: Impair wound healing
■ Antineoplastic agents: Impair fibroblast proliferation and wound contraction
■ Antiinflammatory medicine: Decreases collagen synthesis 45%
■ Lathyrogens: Prevent collagen cross-linking
LOCAL WOUND FACTORS
■ Moisture: Speeds epithelialization
■ Warmth: Increased tensile strength
■ Unfavorable: Poor oxygen delivery, infection, chronic wound, denervation, radiotherapy, free radicals
SKIN ANALYSIS4
SKIN QUALITY
■ Skin type5 (Table 13-1)
Table 13-1 Fitzpatrick Skin Type Classification
| Skin Type | Characteristics | Sun Exposure History |
| I | Pale white, freckles, blue eyes, blond or red hair | Always burns, never tans |
| II | Fair white, blue/green/hazel eyes, blond or red hair | Usually burns, minimally tans |
| III | Cream white, any hair or eye color | Sometimes burns, tans uniformly |
| IV | Moderate brown (Mediterranean) | Rarely burns, always tans well |
| V | Dark brown (Middle Eastern) | Rarely burns, tans easily |
| VI | Dark brown to black | Never burns, tans easily |
■ Skin texture
■ Thickness
■ Pore size
■ Sebaceous quality
■ Discoloration: Hyperpigmentation, solar lentigo, rosacea, telangiectasias
■ Scarring: Acne, surgery, trauma
TIP: Patients with Fitzpatrick skin types V and VI are at higher risk for hyperpigmentation, but show fewer signs of photoaging.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




