Anatomy of the Skin
Introduction
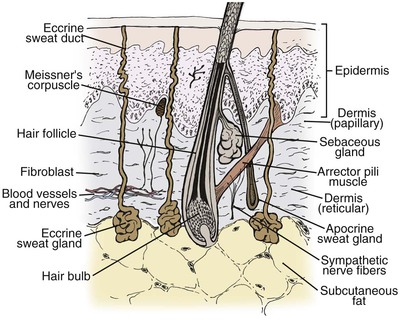
The skin is a complex organ system that is essential for all forms of mammalian life. It may be viewed as a double-layered sheath, cushioned by the underlying subcutaneous adipose tissue, that covers the entire surface of the body. The outer layer of skin, known as the epidermis, is separated from the inner layer, or dermis, by the basement membrane zone. The dermis is attached to the subcutaneous adipose tissue and underlying musculature by fibrous insertions. Important structures, such as epidermal appendages (hair follicles, sebaceous glands, and sweat glands), nerves, blood vessels, and immunologic cells, are present in the skin (Fig. 1-1). As an organ system, the skin has many important physiologic and immunologic properties: it provides a barrier to the environment, regulates body temperature, and serves as an important component of the immune system.1–3
General Characteristics
Skin is highly variable from one person to another and, within the same individual, from one anatomic region to another, with differences to be observed in color, texture, thickness, and content of hair follicles and sebaceous glands. Skin may be divided into smooth, non–hair-bearing (glabrous) and hair-bearing (nonglabrous) areas, although it is virtually always hair-bearing. Skin is the heaviest human organ, weighing approximately 3.8 kg. The largest organ in surface area, the lung, measures about 4.2 m2 on expiration; in comparison, the skin measures approximately 1.7 m2 in surface area. As a tissue, skin ranks fourth in weight behind muscle, adipose tissue, and bone.4
Considerable variation in skin thickness and content of appendages and elastic fibers exists with respect to anatomic region, age, and sex. An appreciation of these variations is clinically important for understanding wound healing and aesthetics. These variations play an integral role in the definition of facial aesthetic regions, boundaries, and junctions. The surgeon must apply knowledge of these factors to the task of determining the best reconstructive option during flap or graft surgery. Careful examination of the skin is essential for making the best tissue match for aesthetic reconstruction. Discrepancies in the thickness of skin edges should be observed before wound closure for exact reapproximation of the edges. The best donor site for a full-thickness skin graft is determined by an examination of all potential donor sites with respect to skin thickness, color, texture, and content of hair follicles and sebaceous glands. Careful examination of the skin before surgery may uncover several clues that could influence the outcome. Individuals with fair skin, light hair, and blue eyes may develop postoperative scars that remain pink for an extended period. Persons with dark skin, hair, and eyes may develop scars that remain pigmented for a prolonged period after surgery. An assessment of previous scars and keloids should be made. Individuals with hyperelastic skin features are characterized by hyperextensibility of the joints (elbows, wrists, and knees), anterior hooding of the navel, and lax skin (Figs. 1-2 to 1-4). These individuals are at higher risk for development of wide scars, permanent railroad tracking suture marks, hypertrophic scars, and prolonged erythema of the scars lasting up to 1 year, eventually resulting in a porcelain-colored white scar. Whereas it is also present in Ehlers-Danlos syndrome, hyperelastic skin is most often simply a relatively common normal variant within the population. Patients with common skin conditions, such as atopic dermatitis, psoriasis, and unusually dry skin, may have high counts of staphylococcal organisms on their skin and thereby increased risk of wound infections. In essence, basic knowledge of skin anatomy is something that is applied daily in reconstructive surgery.

FIGURE 1-2 Hyperextensibility of elbow in a healthy 28-year-old woman with hyperelastic skin features.

FIGURE 1-3 Hyperextensibility of wrist in a healthy 36-year-old woman with hyperelastic skin features.
Epidermis
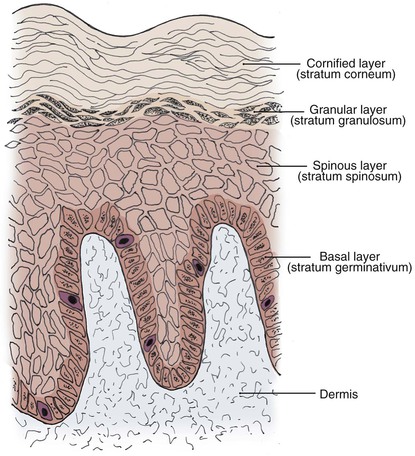
The epidermis, the outermost layer of the skin, is a continually renewing, keratinizing, stratified, squamous epithelium. All epidermal appendages, including hair follicles, sebaceous glands, and eccrine and apocrine sweat glands, derive from this layer. The epidermis consists of four distinct cell types: keratinocytes, melanocytes, Langerhans cells, and Merkel cells. The predominant cell type is the keratinocyte, which constitutes at least 80% of epidermal cells. Four clearly defined layers are identified in the epidermis (Fig. 1-5): basal layer (stratum germinativum), spinous layer (stratum spinosum), granular layer (stratum granulosum), and cornified layer (stratum corneum). The basal layer is the deepest layer in the epidermis. It is composed of a single germinative layer of columnar-shaped keratinocytes that attach to the basement membrane zone and give rise to the more superficial epidermal layers. The next layer, the spinous layer, is several cells thick and composed of polygonal cells with abundant eosinophilic cytoplasm. Small spiny desmosomal attachments between the spinous cells are evident under light microscopy. As the spinous cells migrate superficially and differentiate into granular cells, they become larger and flatter. The granular layer, usually one to four cells thick, is composed of cells with deeply basophilic keratohyalin granules. Further maturation occurs in the outermost stratum corneum, which is highly variable in thickness. In this layer, keratinocytes lose their nuclei and flatten to form plates of keratin, which are shed as “dead skin.” The stratum corneum is thickest on the palms and soles and thinnest on the eyelids and genitalia. Total epidermal turnover time from the basal layer to the stratum corneum is approximately 30 days. The thickness of the epidermis is generally about 0.075 to 0.15 mm. The epidermis is thin at birth, becomes thicker during puberty and early adulthood, and thins in the fifth and sixth decades of life.1,3
Melanocytes
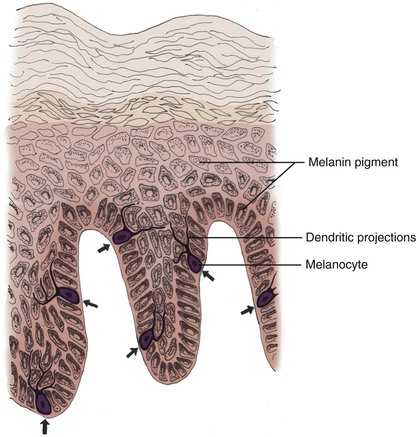
Melanocytes are dendritic, pigment-synthesizing cells of neural crest origin with clear cytoplasm confined to the basal layer. The ratio of melanocytes to basal cells ranges from 1 : 4 on the cheek to 1 : 10 on the limbs. The function of melanocytes is to produce protective melanin pigment. Melanin is packaged in the form of melanosomes, which are transported through stellate dendritic projections to a group of adjacent keratinocytes in the basal and spinous layers (epidermal melanin unit). The keratinocytes engulf the melanosomes and arrange the pigment in an umbrella-like distribution over the nuclei, protecting them from potentially harmful ultraviolet irradiation (Fig. 1-6). This partly explains why people with less pigmentation are at greater risk for development of cutaneous malignant neoplasms, such as basal cell carcinoma, squamous cell carcinoma, and melanoma.5,6 The number of melanocytes does not differ between races. The number and size of melanosomes is greater in pigmented skin and accounts for the darker skin color seen in pigmented persons. In vitiligo, melanocytes are completely absent. In albinism, melanocytes are present but lack the enzyme tyrosinase. Without tyrosinase, tyrosine cannot be transformed into melanin. Tyrosinase activity and melanocyte density decrease with age.7
Langerhans Cells
Langerhans cells are bone marrow–derived, antigen-processing, and antigen-presenting cells found mainly in the suprabasal epidermal layers. They are, however, not unique to the epidermis and are found in other squamous epithelia and in the normal dermis. In routine histologic preparations, Langerhans cells are pale-staining cells that are difficult to identify and more readily demonstrated with special stains or immunohistochemistry. Like melanocytes, Langerhans cells are characterized by dendritic processes. The cytoplasm, as seen by electron microscopy, contains small racket-shaped structures known as Birbeck or Langerhans cell granules. Langerhans cells are responsible for recognizing and presenting antigens to lymphocytes in the skin and are implicated in the pathologic mechanism underlying allergic contact dermatitis and skin allograft reactions. The number of Langerhans cells decreases after ultraviolet irradiation. This results in a diminished capacity for immune surveillance, which may play a role in cutaneous carcinogenesis. The number of Langerhans cells also decreases with age.8