CHAPTER 1 Anatomy
Introduction
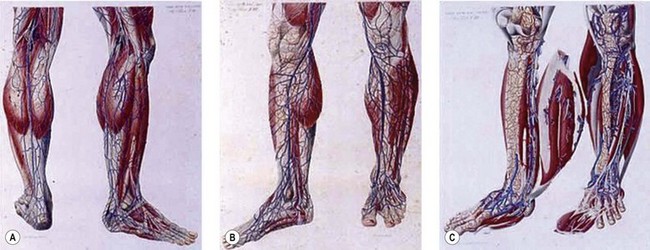
Dissection anatomy, indeed, had its fullest expression from the late eighteenth to the early twentieth century (Mascagni, Gray, Sobotha, Testut, etc.) when all the aspects of dissection anatomy where definitively studied (Fig. 1.1). In the past 50 years anatomical dissection has been little used to investigate venous anatomy, probably because of the assumption that there is nothing new to discover (but also because it is more and more difficult to find cadavers for this purpose). Meanwhile, most anatomical, clinical and surgical textbooks describe the superficial veins of the lower limb as a simple ‘tree’ formed by a few constant and recognizable veins, though clinical experience often shows anomalies and variations with respect to the classical anatomical description or even the complete absence of some of these veins. Furthermore, usually studies in the field of limb veins concern subjects with varicose pathology and rarely subjects with a normal venous system.
Confirming this, the official Anatomical Terminology (Nomina Anatomica)1 includes only a limited number of veins and does not take into account their numerous variations. Inadequacy of official anatomy has caused many authors to name single veins independently or even after the author’s name, which, in the absence of an accepted interpretation frame has added some confusion. The nomenclature consensus statement of 2001 at the Rome UIP World Congress was organized with the purpose of solving this problem (see Table 1.1).2
Table 1.1 Summary of important changes in nomenclature of lower extremity veins
| Old Terminology | New Terminology |
|---|---|
| Femoral vein | Common femoral vein |
| Superficial femoral vein | Femoral vein |
| Sural veins | Sural veins Soleal veins Gastrocnemius veins (medial and lateral) |
| Hunterian perforator | Midthigh perforator |
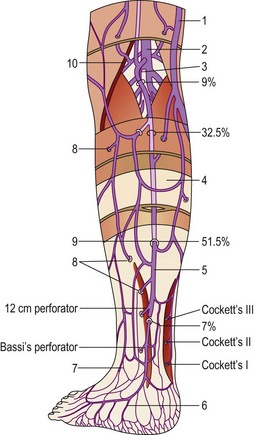
| Cockett’s perforators | Paratibial perforator Posterior tibial perforators |
| May’s perforator | Ankle lateral and medial perforators |
| Gastrocnemius point | Intergemellar perforator |
Modified from Sherman RS: Ann Surg 130:218, 1949.
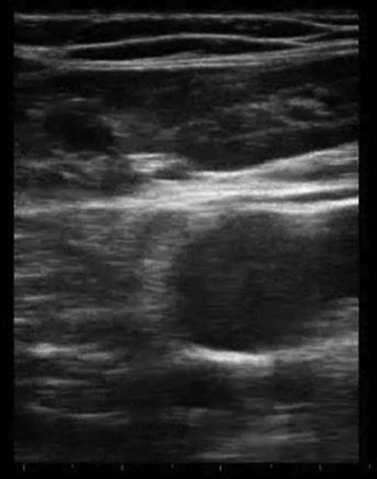
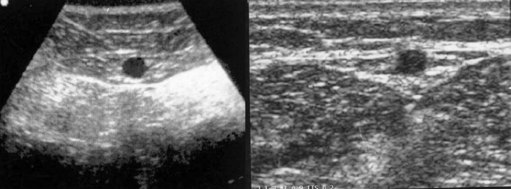
Ultrasound imaging makes it easy to observe the veins of the lower limb, unlike anatomical dissection and phlebography. Examination is non-invasive, repeatable and relatively low in cost. Veins can be observed at full distension, with the patient in a standing position, so that, unlike with anatomical dissection, their real volumetric relationship with the surrounding tissue is readily appreciated. Ultrasound images show not only the veins (as contrast phlebography does), but their relation to surrounding anatomical structures, in particular muscle and fascial layers. This allows precise anatomical identification of the observed veins (Fig. 1.2). Therefore, USI is a unique tool for the study of vein anatomy (US dissection) and makes it possible to verify data obtained from anatomical dissections. In addition, DS allows the detection of blood flow in the observed veins with assessment of their function and involvement in venous pathology. Interestingly, USI was first employed for the clinical identification of pathologically changed veins. Later it was used for collecting data on normal vein anatomy.3
Nomenclature
Nomenclature used throughout the textbook conforms to that developed at the Venous Consensus Conference Classification in 1994.4 In addition, the newest revisions of nomenclature and definitions are used, which were developed at the Nomenclature Congress in Rome in 2001 (Table 1.1).2,5 The long saphenous vein is referred to by the English-Latin term great (GSV). The short saphenous vein is referred to using the English-Latin translation small (SSV), avoiding the term ‘lesser’ as the L could be confused with the term ‘long’. Veins that ‘perforate’ the fascia are termed perforator veins. Veins that connect to other veins within a fascial plane are referred to as communicating veins. The principal deep vein of the thigh is termed the superficial femoral vein, now properly called the femoral vein. The superficial femoral vein actually has turned out to be a potentially lethal misnomer. It has been found that the use of this term is hazardous to patients suspected of having deep venous thrombosis. Many primary care physicians have not been taught and are not aware of the fact that the superficial femoral vein is actually a deep vein of the thigh and that acute thrombosis in this vessel is potentially life threatening.6
General Considerations
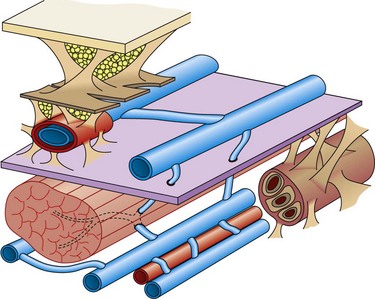
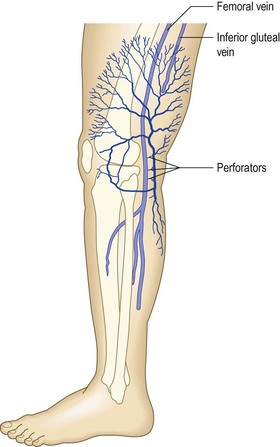
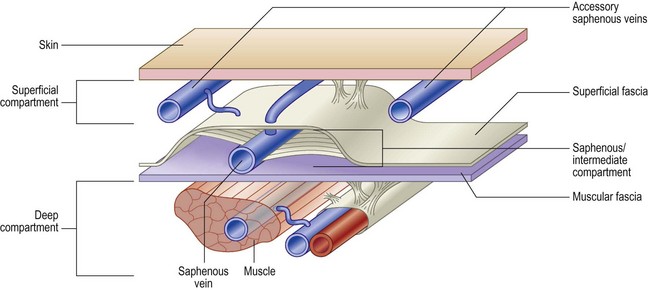
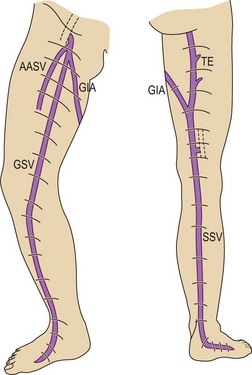
The veins of the lower limbs are traditionally described as consisting of two systems: one within the muscular compartment and its fascia, the deep system, and one superficial to the deep fascia, the superficial compartment (Fig. 1.3).
The lower limb deep venous system is found inside the muscles within the muscular fascia. This allows it to feel the effects of the tonus variations during contraction–relaxation, being the only structure able to vary its volume.7 The superficial veins are in an extrafascial position with respect to the muscles, although the most important (i.e. saphenous veins) are found with superficial fascia duplication.
The lower legs’ deep venous system cannot be seen as an independent entity, separated from the superficial veins. The venous function’s first purpose is to organize the anti-gravity blood backflow to the right heart, taking advantage of it’s volume capacity (three times as much as in arteries), it’s low pressure and it’s compliance, so that the reservoir (the interstitium, depending on lymphatics) may not be involved.7 Other primary important functions, although more localized, are tissue drainage and thermoregulation. These three functions are assured in all different body positions and activity, otherwise ‘venous insufficiency’ occurs.8
Tissue drainage and the maintenance of volume flow are based on valvular and, more importantly, muscle function. Both systems strictly integrate with the venous reservoir function, the respiratory function and the filling ‘vis-a-tergo’ due to the capillary network.7
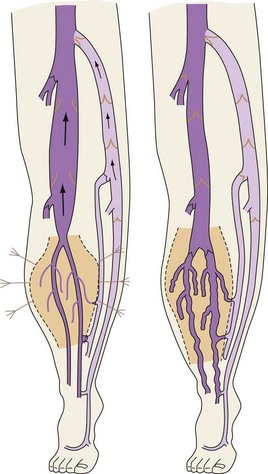
Venous backflow represents about 10% of the total flow at rest, but increases heavily during dynamic conditions due to the physiologic alternate contraction–relaxation of the flexor–extensor muscles. These act as a peristaltic pump and as a dynamic reservoir, conditioning either the squeezing (contraction) or the distension (relaxation) of the deep veins (with action on the venous sole of the foot and, above all, ankle joint movement of particular amplitude conditioning the most important calf pump (Fig. 1.4).
Deep vein communications, mutual or with superficial veins, are extremely frequent so that the postural and the rest phases may address the venous backflow through less resistant pathways, typically the deep veins in the physiologic situation.7
Deep Venous System
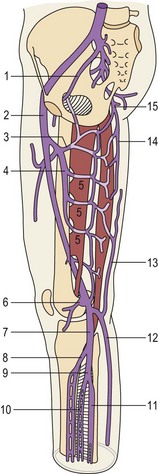
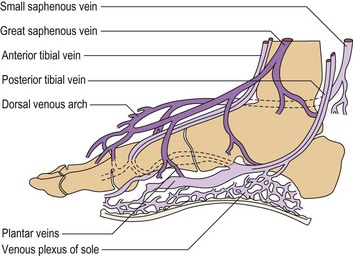
The structure of the deep venous system is shown in Figure 1.5.9 There are at least two deep veins for each of the three arteries (anterior and posterior tibial arteries and peroneal artery), mutually communicating by transverse bridges (like a ladder). The extremely rich muscular plexus (also connected to the superficial veins) drains into these axial veins placed parallel to arteries. At the foot, axial veins are prevalent in the plantar region, where the first pump mechanism is present (Léjars sole) (Fig. 1.6).10–12
At the soleus and gastrocnemius sites the veins are even larger in number and arranged in a spiral shape, due to the longitudinal excursion amplitude of the muscles between contraction and relaxation. This creates a volume reservoir (pump chamber), and the relative muscles (soleus and gastrocnemius) are responsible for both movement/standing position as well as pump function (the second and most important pump). This system is correctly termed the calf muscle pump or peripheral heart (see Fig. 1.4).12
In contrast, posterior deep compartment veins (posterior tibial and peroneal) and anteroexternal compartment veins (anterior tibial) are rectilinear, as the surrounding muscles lean against the bones and have a limited shortening during contraction.7
At the knee and thigh, deep leg veins flow into the collecting system (popliteal-femoral veins). They run in the popliteal crease and adductors canal, and are not enwrapped by a muscular layer as the blood flow to the abdominal cavity has not been held back by compression.7 The other thigh veins (profunda femoris and circumflex) are still deep intramuscular veins. The popliteal vein is also connected by anonymous muscular veins to the profunda femoris and the sciatic nerve vein, creating a natural bypass when obstruction occurs to the femoral vein (thrombosis, extrinsic compression, bone fracture).13 Thanks to this autonomy, the femoral vein is used as an alternative conduit when other more accessible superficial veins are unavailable (see Fig. 1.5).9
The common femoral vein collects the backflow of the lower limb and sends it to the pelvis (iliac veins and inferior vena cava), where aspiration pleurodiaphragmatic forces prevail, together with vis-a-tergo of the renal veins. The common femoral vein in particular receives the GSV below the inguinal ligament where it becomes the external iliac vein. A potential alternative way of discharge in this area is due to the obturator vein (normally draining part of the muscles of the medial thigh) and the sciatic vein, often not macroscopically evident (first embryonic vein, secondarily replaced by the femoropopliteal axis, which can be activated in certain conditions). Together with the superficial veins they can contribute to limb drainage in case of femoral thrombosis by their connection to the hypogastric vein (see Fig. 1.5). However, the same system may be the cause of varices when endopelvic hypertension is transmitted to the superficial limb veins. The sciatic vein may also be involved in congenital venous malformations, typically Klippel-Trenaunay syndrome.13
Anatomy of the Superficial Veins
The most important superficial veins are the GSV and the SSV. It is generally thought that the term saphenous is derived from the Greek word saphenes, meaning evident, but it could also come from the Arabic words el safin, which mean hidden or concealed.14 Of course, these terms were important in the practice of blood letting.
Great saphenous vein
This vein begins on the dorsum of the foot as a dorsal venous arch and internal marginal vein. It passes anterior (10–15 mm) to the medial malleolus, crosses the tibia at the distal third and runs along the tibial internal edge. At the knee the vein it bends posteriorly, running around the condilus femoralis, in contact with the anterior edge of the sartorius muscle, then ascends in the anteromedial thigh, crosses the sartorius and adductor brevis and enters the Scarpa triangle to empty into the common femoral vein (Fig. 1.7).9,15 This termination point is referred to as the saphenofemoral junction (SFJ) but is also known as the crosse, which is the French description for its appearance as a shepherd’s crook. The average diameter of a normal GSV is 3.5–4.5 mm (range 1–7 mm).16
Two large tributaries in the upper third of the thigh – the posteromedial and anterolateral tributaries – join the GSV proximally. These veins usually enter the GSV before it dives posteriorly to penetrate the deep fascia at the fossa ovalis. Both the medial and lateral superficial thigh veins may be so large that they are mistaken for the GSV itself.17 A variable number of perforators connect the GSV to the femoral, posterior tibial, gastrocnemius and soleal veins.18
Small saphenous vein
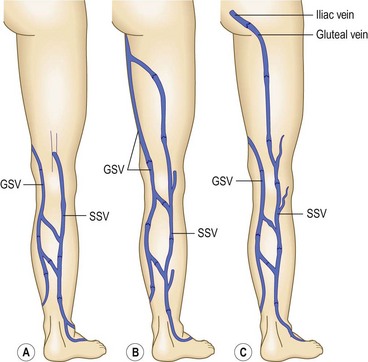
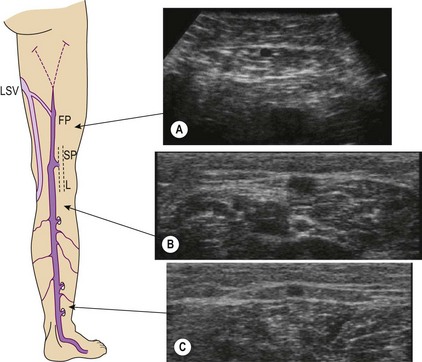
The SSV is the most prominent and physiologically important superficial vein below the knee (Fig. 1.8).9 Like the GSV, the SSV has a thick wall and usually measures 3 mm in diameter when normal.19 It begins at the lateral aspect of the foot and ascends posterior to the lateral malleolus as a continuation of the dorsal venous arch. It continues up the calf between the gastrocnemius heads to the popliteal fossa, where it usually enters the popliteal vein.
The termination of the SSV is quite variable, usually occurring in the popliteal vein, as stated above. However, in 27% to 33% of the population, it terminates above the level of the popliteal fossae, either directly into the GSV or into other deep veins. In 15.3% of patients, the SSV communicates with the popliteal vein, then continues terminating in the GSV. In 9% to 10%, the SSV empties into the GSV or the deep veins below the popliteal fossae.9,20 The SSV may also join the GSV in the thigh through an oblique epifascial vein (the Giacomini vein), or it may continue up under the membranous fascia of the thigh as the femoropopliteal vein, joining the deep veins in the thigh at various locations (Fig. 1.9).21–23
Like the GSV, the SSV runs on or within the deep fascia, usually piercing the deep fascia just below the flexor crease of the knee as it passes into the popliteal fossa.24 Gross incompetence of the SSV usually occurs only in areas where the SSV and its tributaries are superficial to the deep fascia, on the lateral calf and lower third of the leg behind the lateral malleolus. The SSV often receives substantial tributaries from the medial aspect of the ankle, thereby communicating with the medial ankle perforators. The SSV may also receive a lateral arch vein that courses along the lateral calf to terminate in the SSV distal to the popliteal fossa. It may also connect directly with the GSV.
Other superficial veins and collateral veins
The superficial collateral or communicating venous network consists of many longitudinally, transversely and obliquely oriented veins. These originate in the superficial dermis, where they drain cuticular venules. These veins are normally of lesser diameter, but when varicose they can dilate to more than 1 cm. They are thin walled and are more superficial than the superficial fascia that covers the saphenous trunks. They drain into deep veins through the saphenous veins, directly through perforating veins or through anastomotic veins in the abdominal, perineal and gluteal areas.25 Therefore, collateral veins may become varicose either in combination with truncal varicose veins or independently (Fig. 1.10).15
Although many collateral veins are unnamed, some prominent or consistent superficial veins are, for example, the Giacomini vein, which connects the proximal GSV to the SSV. This vein has been found by duplex examination in 70% of limbs with chronic venous insufficiency.26 Other examples include the lateral anterior accessory saphenous vein (AASV), which runs from the lateral knee to the SFJ, the anterior crural veins, which run from the lower lateral calf to the medial knee, and the infragenicular vein, which drains the skin around the knee. Geniculate perforators, although small, may contribute significant reflux (see Figs 1.7, 1.8).
A lateral subdermal plexus of reticular veins, first described by Albanese et al,27 has its origin through perforating veins at the lateral epicondyle of the knee (Fig. 1.11). It has been speculated that it represents a remnant of the embryonic superficial venous system that fails to involute. This system of veins has its importance in the development of telangiectasia. These veins may become varicose even in the absence of truncal varicosities.
Duplex ultrasound anatomy
The most striking progress in the knowledge of venous anatomy for phlebologists is related to the easy visibility of the fascial sheets by DUS imaging. This DUS anatomical ‘dissection’ has offered the key for interpretation of these variations providing a simple universal language for the easy identification of veins (Fig. 1.12).28,29
The result is that leg veins are not just ‘deep’ or ‘superficial’, but are arranged in three levels: deep (beneath the aponeurotic fascia), intermediate (between the aponeurotic fascia and the superficial fascia) and subcutaneous (between the superficial fascia and the skin) (Fig. 1.13).8,28
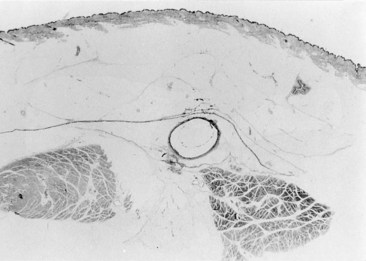
In the early nineteenth century two French anatomists, Cruveilhier30 and Bayle,31 described for the first time that both saphenous veins lie in the deeper compartment of the subcutaneous space and are covered, for their entire length, by the superficial fascia. All other superficial veins (tributaries or collaterals of the saphenous) run into the superficial compartment, between the superficial fascia and the skin, in what is a true subcutaneous position. Despite evidence from anatomical dissection (Fig. 1.14),32 the importance of the superficial fascia as an anatomical classification marker had been largely ignored until DUS became an established tool for venous investigation of leg vein anatomy.29
It was proposed to name the interfascial compartment in which the GSV runs the ‘saphenous compartment’, and the superficial fascia that covers it, ‘saphenous fascia’ (Fig. 1.15).28 The superficial fascia is a marker for distinguishing the two levels of superficial veins. A few constant, and named, superficial veins run through specific intrafascial compartments (intermediated veins), covered by fascial sheet, and belong to the intermediate level. These intrafascial veins are (Fig. 1.16):3,33
These veins are longitudinal ‘blood transfer’ vessels of major importance in understanding varicose hemodynamics. Their position inside the close fibroelastic ensheathing and adventitial anchoring may explain the absence of varicosity in these veins (they enlarge but do not become varicose).34 A pump mechanism during muscular contraction can also be another explanation with caliber reduction due to the fascial compression effect enhancing blood flow8 (Fig. 1.17); similar, but less efficient to what happens in the deep compartment.
Every vein running superficially to the fascial sheet should be considered a collateral or tributary vein (Fig. 1.18). Its identification is consequently of paramount importance when treatment must be provided in a varicose condition. Varicose veins typically belong to this superficial layer.3,8
With a thorough understanding of this scheme, all possible venous anatomical variations may be correctly understood.35
Duplex Ultrasound Markers for Vein Identification
The veins of the intermediate level have constant relationships with the surrounding anatomical structures – fascial sheets, muscles, bones, deep vessels – which are easily recognized by DUS and are therefore ultrasound ‘markers’ for vein identification.3,33 It is from these markers that the following ultrasound identification signs derive.
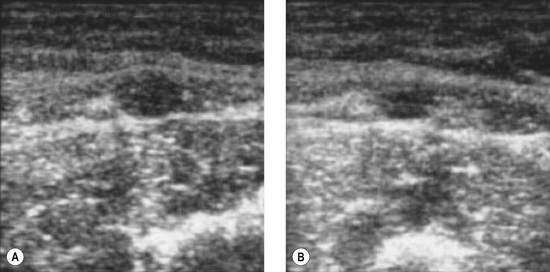
The ‘eye’ sign
Bailly first described, in 1993, the ‘eye’ sign as the ultrasound marker for identification of the GSV in the thigh.29 This sign is due to the fact that the superficial fascia is echo-lucent and easily observed by USI. In transverse scan the compartment in which the GSV runs resembles an Egyptian eye, where the saphenous lumen is the iris, the superficial fasci, the superior eyelid and the aponeurotic fascia the inferior eyelid (see Fig. 1.15). The description of the ‘saphenous eye’ could well be considered the beginning of ultrasound vein anatomy. The eye sign is always present and allows immediate and certain identification of the saphenous vein and its separation from parallel running subcutaneous collaterals.
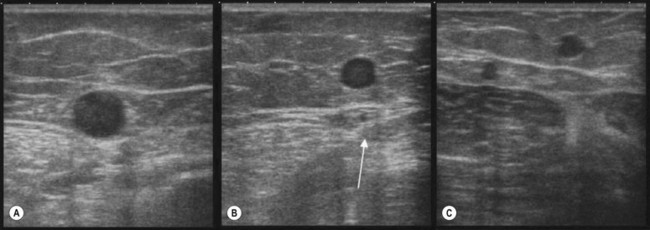
The ‘alignment’ sign
This sign, also suggested by Bailly,37 helps recognize and distinguish the AASV from the GSV.36,38 In the upper third of the thigh on transverse scan into the ‘eye’ there are often two veins instead of one: the GSV and the AASV. The latter lies anterior (lateral) to the GSV39–41 and is identified by its subfascial position and by the fact that in transverse scan it lies over (is aligned with) the common femoral vessels (artery and vein) (Fig. 1.19A). In addition to the alignment sign, in some cases the AASV has, in transverse scan, its own ‘eye’8 (Fig. 1.19B). However, it is the alignment sign that shows that in some cases the only vein visible in the ‘eye’ is the ASV, while the GSV is not visible (absent or hypoplastic) (Fig. 1.19C).38
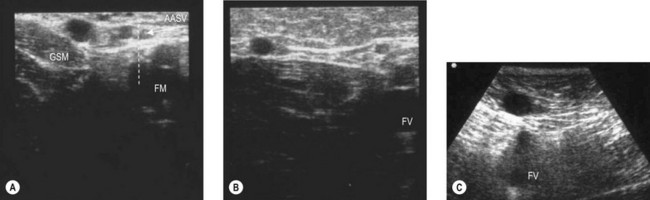
The tibia-gastrocnemius angle sign
This sign allows one to recognize the GSV below the knee, where fascial sheets are often so close to each other that the intrafascial compartment in which the GSV runs may be difficult to recognize.36,42 In such cases the GSV is distinguished from other closely running veins by its position, on a transverse scan, in the angle formed by tibial and medial gastrocnemius muscle (Fig. 1.20A, B). This sign allows one to demonstrate, when the angle is empty, that in this area the GSV is absent or hypoplastic (Fig. 1.20C).
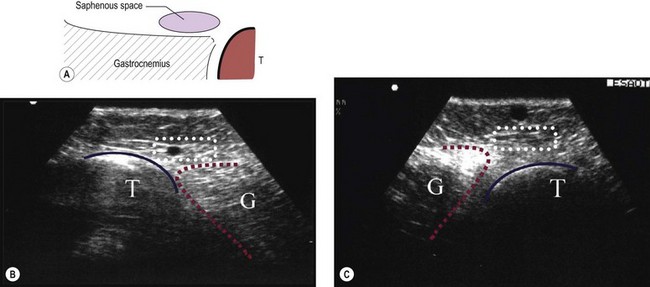
The small saphenous compartment sign
The proximal portion of the SSV lies between the medial and lateral heads of gastrocnemius muscle, while its frequent thigh extension (TE) lies between the semitendinous muscle (medially) and long head of the biceps muscle (laterally). The intermuscular grooves, along which these two veins run, are covered by a thick fascial sheet and appears as a characteristic triangle-shaped compartment on a transverse scan (Fig. 1.21A, B).43,44 This triangle-shaped compartment is always present and allows immediate and certain identification of the SSV/TE and distinguishes it from parallel subcutaneous and deep collaterals. Distal to the gastrocnemius muscle the fascial sheet is still present (Fig. 1.21C), albeit less evident as it is thinner as it approaches the ankle and the marginal vein over the foot indicating that it is the SSV. As for the GSV, it courses inside a specific compartment for its entire length.3
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree