Aging rhinoplasty requires deep anatomic understanding of the effects of aging on the skin, subcutaneous tissue, cartilaginous framework, and bony structure. Elderly patients with realistic expectations should be sought after. A complete medical history should be obtained to determine fitness for surgery. The primary surgical maneuvers performed correct tip ptosis and address obstructive airway concerns. Care should be taken to avoid over-dissecting the underlying nasal framework owing to age-related attenuation of the bony and cartilaginous structure. When surgery is undertaken in a safe manner on properly selected patients, high satisfaction rates can be obtained.
Key points
- •
Rhinoplasty in the aging population requires deep understanding of the attenuation of the underlying anatomic framework with time.
- •
Careful patient selection is of utmost importance, which can be parsed out in the initial patient interview.
- •
Primary surgical maneuvers address tip ptosis, the main aesthetic concern in this patient population.
- •
Nasal airway obstruction is common, which may be addressed by some combination of septoplasty, inferior turbinate reduction, internal and external nasal valve stabilization, and tip support.
Introduction: nature of the problem
The aging nose presents a particularly difficult challenge to the rhinoplasty surgeon. In 2023, there were over 40,000 rhinoplasties performed in the United States according to the Aesthetic Society Procedural Statistics [ ]. Of those, 14.9% and 4.2% were performed on patients in the 51 to 64 and 65+ age range, respectively, an increase in both overall volume and proportion from 2019. The nasal infrastructure undergoes well-described anatomic changes as the face ages, and these must be addressed with particular surgical techniques.
The structural framework of the nose is composed of paired nasal bones, upper lateral cartilages, and lower lateral cartilages. The lower lateral cartilages form the nasal tip, which can be divided into the medial, middle, and lateral crural cartilages. The integrity of the nasal tip relies on the ligamentous attachments of the scroll area, connecting the caudal border of the upper lateral cartilages to the cephalic border of the lower lateral cartilages.
The main aesthetic concerns specific to this population include tip ptosis and gradual nasal lengthening due to changes in skin quality, weakening of the cartilaginous structures, and remodeling of the underlying bony framework [ ]. In the younger patient, the face can be divided into thirds by drawing horizontal lines at the menton, nasal base, and brow. The aging face undergoes subcutaneous fatty resorption, orbicularis oculi atrophy, midface volume loss, and maxillary alveolar hypoplasia resulting in shortening of the lower third and relative lengthening of the upper and middle third of the face [ ]. These aesthetic changes can be corrected with tip rotation and projection [ ]. Elderly patients may also present with functional concerns, including nasal airway obstruction due to either long-standing internal valve collapse, or newly developed external valve collapse secondary to lateral nasal wall collapse [ ]. Nasal tip ptosis may simply cause nasal airway obstruction over time that patients will note on their own. These patients may require extra intervention to stabilize the lower lateral cartilages to improve their functional and aesthetic concerns or nasal tip rotation.
Skin and Subcutaneous Tissue
With time, the epidermis and dermis thin, dermal collagen levels decrease, and elastin and fibrillin become more disorganized [ ]. Lifelong sun exposure further compounds the effects of aging, resulting in decreased skin elasticity and rhytid formation [ , ]. Aging of the skin of the nose, specifically, exhibits increased density of sebaceous glands, most notably in males [ , ]. At its most extreme, this can lead to rhinophyma. However, even a slight increase in sebaceous glands can result in the appearance of increased thickness of the nasal alae and tip. This increases the weight of the nasal tip and contributes to tip ptosis. The combination of decreased skin elasticity, midface volume loss, and increased density of sebaceous glands require more pronounced change to the nasal framework to change the nasal appearance.
Cartilage Changes
Many elderly patients complain of tip deprojection and underrotation largely as a result of structural changes to the cartilaginous nasal tip complex and the effects of aging/gravity. Tip rotation is defined as the movement of the nasal tip in reference to the upper lip. The ideal angle varies with societal norms and gender, but is typically within 95 to 115° for women and 90 to 95° for men [ ]. Tip projection is defined as the horizontal distance from the alar crease to the nasal tip on lateral view. Several metrics have sought to define the ideal tip projection: the Goode ratio defines the ideal ratio of tip projection to nasal length as 0.55:1; Simon’s method states tip projection should be equivalent to the length of the upper lip; and Lanser’s ratio describes the nose as a right triangle with the proportion of projection: height: length equivalent to 3:4:5 [ ].
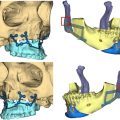
There is weakening of the intracrural ligament resulting in loss of medial crura tip support and derotation over time, a major contributor to tip ptosis [ , , , ]. Age-related maxillary alveolar hypoplasia leads to spreading of the medial crural foot plates and columellar shortening, further destabilizing the nasal tip [ , ]. Additionally, attenuation of the ligamentous attachments of the scroll area, connecting the upper and lower lateral cartilages, contributes to the changes associated with the aging nose [ ]. This results in downward migration of the lower lateral cartilages, contributing to loss of tip support and external nasal valve collapse.
Nasal Dorsum
One must assess whether a dorsal hump is a long-standing nasal characteristic or newly developed aesthetic concern [ , ]. As a result of age-related tip ptosis and nasal lengthening, the illusion of a prominent dorsal hump may present due to the appearance of nasal convexity. In many cases, this is resolved by addressing tip ptosis. Therefore, one should start with surgical maneuvers to rotate and project the nasal tip before pursuing dorsal hump reduction. This can be assessed preoperatively by holding the tip in desirable location and visualizing whether dorsal hump persists [ ].
Airway Concerns
In addition to nasal aesthetics, many elderly patients have a combination of functional complaints as well. Patients may present with long-standing nasal airway obstruction due to internal or external nasal valve collapse, septal abnormalities, or inferior turbinate hypertrophy. Additionally, aging itself affects nasal airway mechanics. Tip ptosis alters airflow within the nasal vault and produces obstructive symptoms by shunting air flow superiorly [ , , ]. Internal nasal valve collapse may worsen secondary to age-related separation of upper and lower lateral cartilages [ ]. External nasal valve collapse may result due to a combination of tip ptosis and lateral nasal wall collapse [ , , ]. Many of the age-specific airway concerns can be addressed with tip rotation and projection, which will be discussed in a later section.
Skeletal Remodeling
The facial skeleton undergoes well-defined differential craniofacial growth throughout adulthood. The horizontal position between the sella nasion line to the pyriform on lateral view has shown to increase with age, indicating midface retrusion [ ]. This leads to alar base recession and tip support attenuation. The pyriform also remodels cephalad, causing the alar base to be pulled superiorly and nasal tip to rotate inferiorly. The effect is an elderly appearing nose with an alar base that lies above the columella and nasal tip. Age-related maxillary alveolar hypoplasia results in spreading of the medial crural footplates and columellar shortening, further attenuating tip support mechanisms [ ]. Lastly, the nasal bones become increasingly fragile with age. Therefore, osteotomies should be done with extreme care, or avoided altogether [ ].
Surgical technique
Preoperative Planning
Patients should be evaluated preoperatively with a complete medical history and focused physical examination. In the patient interview, one should tease out motivation for pursuing rhinoplasty. The ideal patient is realistic and secure, understands the limitations of rhinoplasty in the aging person, and lists specific concerns about their nasal appearance. In our practice, we ask patients to verbalize their concerns about their nose, in order of importance. If they are unable to verbalize specific complaints, surgical intervention should be avoided. Patients may present with aesthetic or functional chief complaints. If the patient has long-standing aesthetic concerns, expectations should be tempered, as these issues are more difficult to address due to age-related changes to the nasal framework. Recent changes in financial status are common in this cohort, such as career change or promotion, retirement, or inheritance. These patients tend to be good candidates for surgery, demonstrating high postoperative satisfaction rates [ ]. Patients in this age group may pursue surgery because of a recent life stressor, such as divorce or death of a loved one. This should be recognized, and aesthetic surgery delayed until any grief or stress has completely resolved.
Medical comorbidities are more common in the elderly population and should be carefully assessed to determine if a patient is a surgical candidate. Hypertension should be properly medically managed to prevent risk of postoperative bleeding. Ideally, diabetic patients should be well controlled to decrease wound healing complications and infection risk. Patients with a history of cardiovascular disease or stroke need to obtain surgical clearance from their cardiologist and primary care physician. A complete list of medications should be assessed. Any anticoagulants should be stopped before surgery after receiving medical clearance. Patients unable to stop anticoagulation therapy in the perioperative period should not be considered a surgical candidate. Lastly, specific nasal history should be obtained, including any previous nasal trauma, allergies or sinus pathology, or nasal surgeries.
The physical examination should include a complete head and neck examination, as head and neck malignancies are more common in the elderly population. A complete external aesthetic nasal analysis is then performed to define nasal deformities, paying close attention to the patient’s specific aesthetic complaints. An internal examination is performed to evaluate the integrity of the internal nasal valve, inferior turbinate hypertrophy, or septal deviation. Standard photographs should be taken and reviewed with the patient, permitting a genuine discussion of any surgical limitations to their concerns. If jointly realistic results are defined and agreed upon between patient and surgeon, an operative plan can be devised.
Preparation and Patient Positioning
The patient is positioned supine on the operating table. Following endotracheal intubation, the table is turned either 90 or 180° with the endotracheal tube extended off the foot of the bed. The skin is prepped with povidone-iodine solution before draping. Surgical techniques are detailed in Table 1 .
| Surgical Maneuver | Technique | Result |
|---|---|---|
| Medial crura-septal fixation suture |
|
|
| Septal extension graft |
|
|
| Columellar strut graft |
|
|
| Premaxillary graft |
|
|
| Lateral crural steal |
|
|
| Lateral crural overlay |
|
|
| Alar cephalic trim |
|
|
| Onlay Tip raft |
|
|
| Dorsal Hump Reduction |
|
|
| Nasal bone osteotomies |
| |
| Lateral Crural Strut Grafts |
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree