This article explores surgical adjustments to the maxillofacial skeleton to enhance facial harmony. It begins with an overview of the anatomy and its critical role in supporting soft tissues, influencing proportions, and maintaining balance. Principles of facial esthetics, incisor show, and lip length are discussed as guidelines for achieving optimal outcomes. Key surgical techniques are detailed. Advancements in virtual surgical planning, patient-specific hardware, and custom facial implants are highlighted. Functional considerations underscore the interplay between esthetics and functionality. Real-world case studies illustrate the transformative impact of these interventions. The article concludes with future directions.
Key points
- •
Maxillofacial skeletal adjustments enhance facial harmony by refining proportions, improving symmetry, and achieving esthetically balanced outcomes.
- •
Virtual surgical planning for corrective jaw surgery and custom implants allow precise modifications tailored to each patient’s unique esthetic needs.
- •
Techniques like LeFort I osteotomies, mandibular adjustments, and genioplasty optimize facial contours and incisor display for improved esthetic appeal.
- •
Addressing facial proportions, including thirds and fifths, and correcting asymmetry significantly impact overall attractiveness and patient satisfaction.
| CPAP | continuous positive airway pressure |
| DOME | distraction osteogenesis maxillary expansion |
| EASE | endoscopically assisted surgical expansion |
| HA | hydroxyapatite |
| MARPE | miniscrew-assisted rapid palatal expansion |
| MIND | minimally invasive nasomaxillary distraction |
| MMA | maxillomandibular advancement y6 |
| OSA | obstructive sleep apnea |
| SARPE | surgically assisted rapid palatal expansion |
| TMJ | temporomandibular joint |
| UARS | upper airway resistance syndrome |
| VSP | virtual surgical planning |
Introduction
Facial harmony and balance are foundational to esthetic appeal. Subtle variations in the proportions of facial structures can make a significant impact on perceived attractiveness. The maxillofacial skeleton—the maxilla, mandible, zygomatic arches, and surrounding structures—plays a central role in defining these proportions and supporting the overlying soft tissues. Adjustments to the maxillofacial skeleton can significantly enhance facial balance, improving esthetics and functionality.
This article explores surgical modifications aimed at optimizing facial harmony by adjusting the maxillofacial skeleton. These adjustments cater to a range of patient needs, from correcting congenital asymmetries to addressing age-related changes and enhancing natural features. Specialists across cosmetic surgery disciplines—including plastic surgeons, facial plastic surgeons, oculoplastic surgeons, and cosmetic dermatologists—will find these insights valuable for understanding how targeted skeletal changes can elevate surgical outcomes.
The article outlines key anatomic structures, principles of facial proportions, and surgical techniques used for skeletal adjustments. It will also cover advancements in custom orthognathic surgery, virtual surgical planning, custom facial implants, and minimally invasive midface expansion options that support facial enhancement. Practical case studies illustrate the application of these concepts, emphasizing the balance between esthetics and functional health. The aim is to provide a comprehensive overview that integrates current best practices and future directions in maxillofacial surgery.
Anatomy of the maxillofacial skeleton
A thorough understanding of the maxillofacial skeleton is fundamental for making precise surgical adjustments that enhance facial harmony. This section outlines the key skeletal structures, their relationships with soft tissues, and the importance of their interactions in achieving aesthetic and functional outcomes.
Key Structures
The maxillofacial skeleton comprises several critical components that shape the face [ ].
Maxilla
The upper jawbone forms much of the midface and supports the upper teeth. The maxilla plays a critical role in the projection and width of the midface, influencing incisor show, the smile arc, and the relationship between the nose and lips. Moreover, the nasal cavity volume and width of the nasal floor are determined by transverse maxillary development. Abnormal positioning or growth of the maxilla can lead to issues with occlusion, nasal obstruction, insufficient tongue space, and aesthetic imbalances in the midface.
Mandible
The lower jawbone defines most of the lower third of the face and contributes to jawline definition and facial symmetry. Variations in mandibular position, shape, and size can impact occlusion, pharyngeal airway size, chin projection, and overall facial harmony.
Zygomatic arch
The zygomatic bones form the cheekbones, creating lateral projection in the midface and contributing significantly to facial width and contour. The prominence of the zygomatic arches influences midface balance and can be a focal point in achieving facial harmony, in anterior and lateral projection.
Nasal and orbital bone
Nasal and orbital bone plays a central role in facial symmetry, nasal projection, periorbital esthetics, and overall facial balance. However, alterations to these structures are not discussed in this article.
Relationship of Soft Tissues to the Facial Skeleton
The overlying soft tissues of the face are significantly influenced by the underlying skeletal framework. The bone structure serves as the foundation for facial contours, determining the positioning of the skin, muscles, and fat [ ].
Soft tissue support
The maxillofacial skeleton shapes soft tissue draping, affecting youthfulness and proportion. Inadequate skeletal support, such as insufficient maxillary projection, can reduce incisor show and prematurely age the face [ ].
Response to skeletal changes
Adjusting bone structures affects soft tissue support. Maxillary advancements improve midface projection and the nasolabial angle, while mandibular changes can reduce jowls and marionette lines. A retruded jawline contributes to sagging skin and deepened lines, but surgical skeletal expansion enhances support and minimizes aging signs.
Principles of facial proportions and incisor show
Jaw deformities can impact the shape, size, position, orientation, and symmetry of the maxilla and mandible [ ]. Facial harmony requires aligning skeletal and soft tissue elements based on established proportions. Although influenced by cultural and personal aesthetics, these ratios guide balance. This section explores key concepts, including the golden ratio, symmetry, skeletal positioning, and the role of incisor display and lip length in achieving esthetic outcomes.
Ideal Facial Proportions
Facial proportions are typically divided into distinct regions, providing a reference for surgical adjustments [ ].
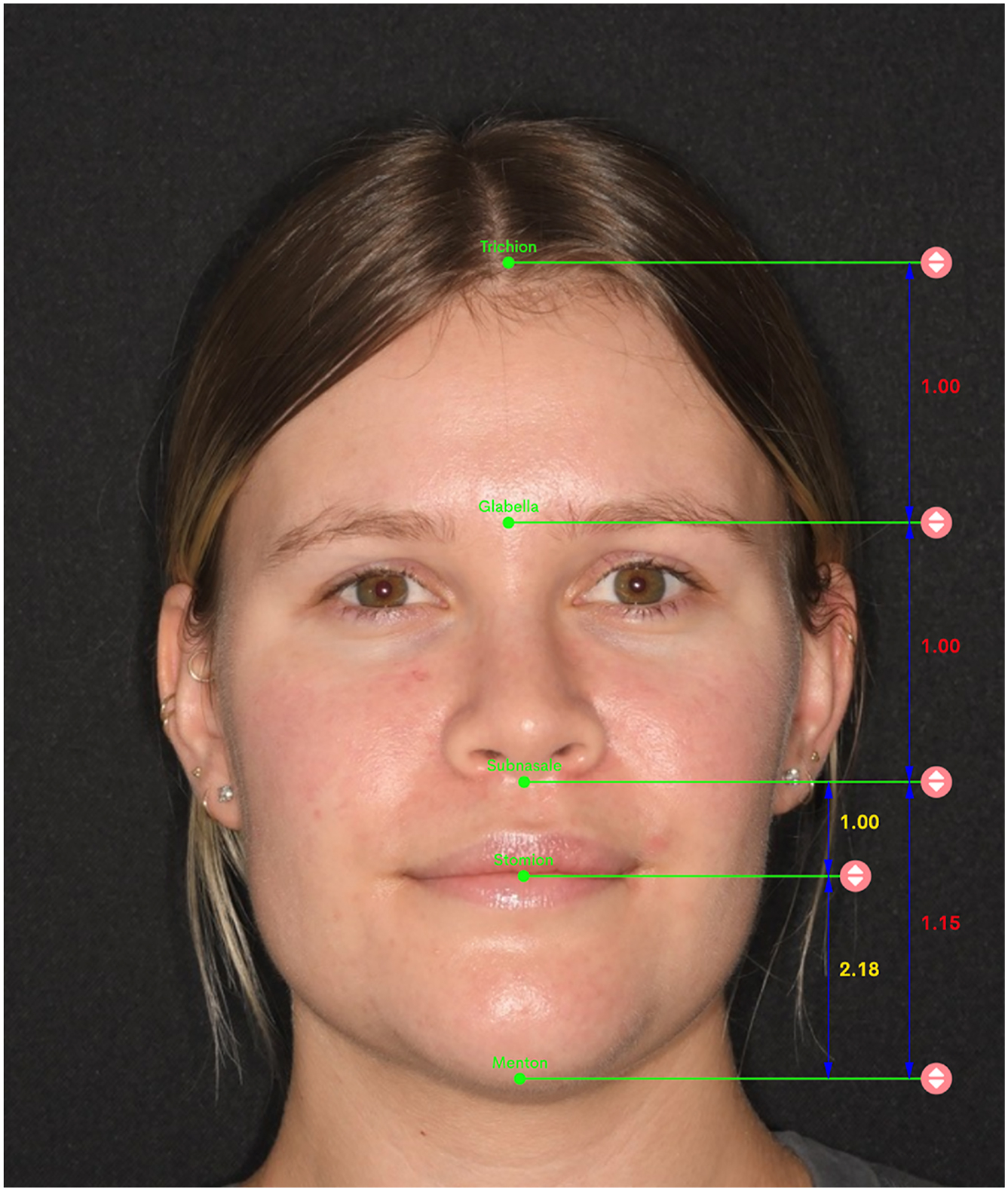
Facial thirds
The face is divided horizontally into 3 equal sections ( Fig. 1 ): upper third (trichion to glabella), middle third (glabella to subnasale), and lower third (subnasale to menton). Within the lower third, the ideal ratio between the upper lip and lower lip-to-chin distance is approximately 1:2. Deviations in this ratio can disrupt harmony in the lower face, impacting aesthetic and functional outcomes.
Facial fifths
The face is divided vertically into 5 equal sections, establishing ideal spacing between the eyes, nose, and lateral facial edges. Proper alignment in these regions contributes to lateral symmetry and overall width ( Fig. 2 ).

Golden ratio
The golden ratio (1.618:1) is a classic guide in facial aesthetics, applied to dimensions like face width to height, eye spacing, nose width, and mouth. Alignment with this ratio is often associated with perceived attractiveness [ ].
Facial Symmetry
Symmetry is a fundamental aspect of facial attractiveness, with balanced, mirror-like halves contributing to a harmonious appearance. Skeletal adjustments in maxillofacial surgery are often guided by the goal of enhancing symmetry, especially in the midface and jawline. Surgical plans frequently aim to correct asymmetries that may exist in bone structure, providing a more cohesive foundation for soft tissue draping and overall facial aesthetics [ ].
Skeletal Proportions
Skeletal proportions play a critical role in defining forward maxillary position, chin positioning, and overall skeletal harmony. Certain reference lines and landmarks are used to assess these positions.
Andrews’ six elements of orofacial harmony and the GALL line
This analysis outlines the ideal positioning of maxillary and mandibular structures for facial balance, with particular emphasis on maxillary projection relative to the forehead [ ]. The ideal maxillary position is when the midpoint of the upper incisor aligns with goal anterior-limit line (GALL), which is parallel to the head’s frontal plane and passes through a line connecting the foreheads anterior-limit line and the glabellar vertical line.
Chin positioning and holdaway analysis
Ideal chin prominence can be assessed through the holdaway analysis, which measures the relationship between the most forward point on the chin (pogonion) and the NB line (a line drawn from the nasion to the B point). In a balanced profile, the pogonion should be approximately 2 mm behind the NB line, matching the ideal distance of the lower incisor’s most forward point (L1) from the NB line [ ].
Control of Incisor Show
A key component in achieving an aesthetically pleasing smile is controlling the amount of maxillary incisor display. Proper incisor show contributes to facial vibrancy and youthfulness, while excessive or insufficient display may distort facial balance [ ]. Surgical adjustments to the maxilla can control incisor display include
- •
Vertical maxillary impaction, which reduces maxillary height to correct excessive incisor show and a gummy smile, improving smile aesthetics and facial proportions
- •
Downgrafting, which increases incisor display in cases of inadequate visibility, enhancing balance and facial aesthetics
- •
Cant or roll correction, which addresses maxillary asymmetry to improve uneven incisor display, enhancing facial harmony and smile aesthetics
Lip Length Considerations
The relationship between lip length and incisor display is critical for balanced facial proportions [ ]. When lip length is excessive, incisor show may be minimized, resulting in an aged or less vibrant appearance. Conversely, normal lip length allows for optimal control of incisor display through skeletal adjustments alone.
Excessive lip coverage
In cases where lip length conceals the maxillary incisors excessively, surgical interventions such as lip lifts may be considered to adjust the balance between lip and incisor display [ ].
Normal lip length
For patients with standard lip length, precisely controlled maxillary adjustments, such as those listed previously, can optimize incisor display without altering the lips themselves [ ].
Ethnic and Gender Variations
Perceptions of ideal facial proportions and incisor display vary across different ethnicities and genders [ , ]. These variations influence surgical planning, as patient expectations and anatomic baselines vary. Recognizing these factors allows practitioners to tailor adjustments to align with individual and cultural aesthetic preferences. The principles outlined here emphasize the role of facial proportions in achieving balanced, personalized outcomes, forming a foundation for maxillofacial surgery that enhances aesthetics and function.
Surgical adjustments to the maxillofacial skeleton
Surgical adjustments to the maxillofacial skeleton are essential for enhancing facial harmony, correcting translation discrepancies, addressing orientation issues, and achieving symmetry. By modifying key structures such as the maxilla, mandible, chin, and zygomas, surgeons can significantly impact facial proportions and balance. This section outlines the primary surgical techniques used to adjust these structures.
Maxillary Adjustments
Maxillary adjustments are performed to correct vertical, horizontal, transverse, or orientational discrepancies, impacting everything from incisor display to midface projection. The primary surgery performed on the maxilla is the LeFort 1 osteotomy.
LeFort I osteotomy
This transoral procedure involves horizontal sectioning of the maxilla at the LeFort I level (just above the roots of the teeth and a few millimeters above the floor of the nose) [ ]. This osteotomy separates the maxilla from the surrounding facial bones, allowing it to be mobilized. Using virtual surgical planning (VSP) and titanium hardware for fixation, this technique provides nearly full 3-dimensional control over the positioning of the maxilla.
High LeFort I osteotomy
A variation of the standard LeFort I osteotomy, this approach raises the osteotomy level to sometimes include the lower part of the zygoma [ ]. This modification enables enhanced midface projection, which can be beneficial for patients with midface hypoplasia.
Transverse Maxillary Expansion Techniques
All methods of transverse maxillary expansion widen the dental arch, reducing negative spaces and enhancing the patient’s smile. Additionally, these techniques broaden the palate, increasing tongue space to improve airway function and expanding the volume of alveolar bone, which facilitates better orthodontic alignment.
Segmental LeFort expansion
Performed during orthognathic surgery, this technique broadens the maxilla and nasal floor to increase transverse width. It primarily addresses occlusal issues and increases tongue space with minimal impact on nasal breathing. A key advantage is the completion of expansion during surgery, although it is limited to approximately 6 mm [ ].
Traditional two-piece LeFort I osteotomy
Also called surgically assisted rapid palatal expansion (SARPE) [ ] or distraction osteogenesis maxillary expansion (DOME) [ ], this technique combines a midline maxillary split with a LeFort I osteotomy to achieve significant transverse expansion. It addresses occlusal issues, increases tongue space, and moderately improves nasal breathing, with expansion limited by the palatal distractor.
Minimally invasive midface expansion techniques
Recent minimally invasive methods, such as MARPE (miniscrew-assisted rapid palatal expansion), allow expansion not only at the LeFort I level but across the entire midface [ , ]. Additionally, techniques like MIND (minimally invasive nasomaxillary distraction) [ ]and EASE (endoscopically-assisted surgical expansion) [ ] enable controlled midface expansion in complex cases. The benefits of midface expansion include 3-dimensional widening of the entire nasal cavity, significantly reducing nasal obstruction and airway resistance, and enhancing zygomatic (cheekbone) projection, which can also be cosmetically beneficial.
Mandibular Adjustments
Mandibular surgeries correct chin prominence, jaw asymmetry, and occlusion, enhancing the lower facial third and jawline definition. These procedures often improve oropharyngeal airway size, benefiting patients with sleep-breathing disorders.
Bilateral sagittal split osteotomy
This commonly performed intraoral procedure enables forward, backward, and orientational adjustments of the distal mandible to correct prognathism or retrognathism, enhancing jaw alignment and facial balance. However, it is less suitable for patients with reduced mandibular ramus height [ ].
Inverted-L osteotomy
This is used for vertical elongation, large advancements, and orientational adjustments of the mandible. Traditionally performed extraorally, it can now be completed intraorally with VSP and custom hardware. Bone grafting is required to fill the gap created by the osteotomy [ ].
Additional Mandibular Procedures
Genioplasty
Genioplasty reshapes the chin to enhance lower facial balance, allowing precise control over chin position, height, width, and projection. By advancing or setting back the chin, surgeons can influence profile harmony [ ]. Additionally, a wedge resection can be used to narrow or widen the chin, while vertical modifications allow for control over lower facial height [ ].
Mandibular contouring and angle reduction
Cosmetic contouring of the mandibular body and angles can soften overly prominent structures, refining the jawline for a more harmonious and aesthetically pleasing appearance [ ].
Mandibular angle and chin implants
These are available in stock or custom-made designs, and they improve jawline definition and chin prominence. Custom implants precisely match the patient’s anatomy for optimal symmetry and contour, while stock implants provide a cost-effective option. These implants enhance lower facial width, projection, and overall aesthetic harmony [ , ].
Zygomatic (Malar) Adjustments
Zygomatic, or malar, adjustments impact midface width, cheekbone prominence, and facial symmetry. Techniques include augmentation and reduction to achieve balanced contours.
Zygomatic (malar) augmentation
Stock implants, custom implants, and hydroxyapatite (HA) are used to enhance cheekbone projection [ ]. Custom implants are tailored to the patient’s anatomy for precise control over symmetry, projection, and contour, while HA and stock implants offer more economical options. This approach is ideal for adding volume and definition to flat or underprojected cheekbones.
Zygomatic reduction
For overly prominent or wide cheekbones, zygomatic reduction narrows midface width, softening lateral projection to create a balanced appearance. This procedure is particularly popular in Asia [ ].
The combination of these surgical techniques allows practitioners to customize facial adjustments based on each patient’s unique anatomy and aesthetic goals. Each intervention is planned to address a patient’s specific needs, creating a harmonious, individualized result.
Virtual surgical planning and patient-specific hardware
Advancements in VSP and custom 3-dimensional printed titanium (patient-specific) hardware have revolutionized maxillofacial surgery by enabling unparalleled facial skeletal analysis, surgical planning, precision, and customization. These technologies allow surgeons to preoperatively simulate procedures, predict outcomes, and develop tailored solutions that enhance functional and aesthetic results [ , ].The integration of custom facial implants further expands the potential for achieving optimal outcomes, especially in complex cases.
Virtual Surgical Planning
VSP involves the use of advanced 3-dimensional imaging and modeling software to map the patient’s anatomy and design a surgical plan with pinpoint accuracy. Key benefits of VSP include diagnosis, mapping, and preoperative simulation.
Diagnosis and mapping
VSP employs 3-dimensional cephalometry and skeletal measurements to diagnose dentofacial issues. By analyzing proportions in 3 dimensions, it identifies discrepancies that may not be apparent in traditional imaging or clinical examinations, improving diagnosis and treatment planning.
Preoperative simulation
VSP enables simulation of osteotomies, adjustments, and hardware placement, minimizing intraoperative guesswork and enhancing accuracy. Visualizing outcomes allows surgeons to refine approaches, achieving functional and aesthetic goals with greater predictability.
Traditional corrective jaw surgery uses VSP in conjunction with prefabricated occlusal splints that aid in jaw positioning before fixation.
Patient-Specific Hardware
Patient-specific hardware refers to custom-designed plates and surgical guides created using the patient’s unique anatomy. These components, designed in conjunction with VSP, improve the accuracy and efficiency of maxillofacial procedures [ , ]. Key features include surgical guides and custom plates.
Prefabricated surgical guides allow for accurate osteotomies, bone reduction, and predrilling of screw holes, ensuring precise execution of the surgical plan.
Designed to match the patient’s bone contours, custom plates minimize intraoperative adjustments, reducing surgical time. When paired with surgical guides, they ensure precise plan execution. Their 3-dimensional printed rigidity also enhances postoperative stability compared with traditional hardware.
Integration of Custom Facial Implants
Custom facial implants designed through the VSP process expand the possibilities for achieving optimal aesthetic and functional outcomes. These implants address deficiencies in midface projection, jawline definition, and areas not fully correctable with skeletal osteotomies. They can also be precisely designed to integrate with 3-dimensional printed titanium plates, ensuring accurate placement during surgery.
Functional considerations
Functional considerations are paramount in maxillofacial surgery, as skeletal adjustments traditionally address both aesthetic goals with improvements in critical functions such as breathing, chewing, swallowing, and speaking [ ]. Functional improvements often align with aesthetic goals, as proper skeletal alignment enhances appearance and mechanical performance. Addressing these issues not only enhances the patient’s quality of life, but also ensures long-term health and stability.
Airway Obstruction and Sleep Apnea
Skeletal adjustments can significantly impact airway size and function, making breathing optimization a primary focus of maxillofacial surgery. Documented cases of obstructive sleep apnea (OSA) unresponsive to conservative measures, such as continuous positive airway pressure (CPAP) or oral appliances, often require surgical intervention.
- •
Maxillomandibular advancement (MMA): Bimaxillary advancement surgery is one of the most effective treatments for sleep-disordered breathing, such as OSA. This procedure expands the oropharyngeal airway, reducing airway resistance and improving breathing [ ].
- •
Maxillary/midface expansion: Techniques that expand the maxilla or midface help reduce nasal obstructions and airway resistance, leading to improved breathing.
Chewing and Swallowing Difficulties
Impairments in chewing and swallowing caused by skeletal discrepancies can significantly affect a patient’s ability to process food effectively. Surgical interventions aim to align the jaws and teeth properly, enabling efficient mastication.
Speech Disorders
Speech articulation problems can arise because of jaw misalignment. These issues often require surgical correction to improve the positioning of the jaws.
Temporomandibular Joint Disorders
Temporomandibular joint (TMJ) disorders are frequently linked to jaw misalignment. Maxillofacial surgery can relieve TMJ stress by achieving proper jaw alignment and dental occlusion.
By addressing airway management, chewing, swallowing, speech, and TMJ health, maxillofacial surgery not only enhances facial esthetics but also significantly improves functional outcomes and quality of life.
Case studies and examples
Case Study 1: Comprehensive Orthognathic Surgery for Functional and Aesthetic Improvement
Patient overview
A 23-year-old woman presented with jaw tension, difficulty chewing, and speech articulation.
Clinical and radiographic findings included class III skeletal underbite, macrogenia with a wide chin, broad mandibular bodies, and insufficient incisor display despite normal lip length.
Surgical intervention included
- 1.
LeFort I osteotomy, 3-pieces: the maxilla was advanced, downgrafted, and expanded horizontally to improve incisor display and enhance midface projection
- 2.
Bilateral sagittal split osteotomies (BSSOs)
- 3.
T-genioplasty, which narrowed the chin with a wedge resection
- 4.
Mandibular contouring, which reduced the width of the mandibular body to create a more harmonious jawline
The surgical outcomes demonstrated significant functional and aesthetic improvements. Functional outcomes included jaw alignment relieved tension that allowed for proper chewing, improved articulation, and improved sleep quality. Aesthetic outcomes included more proportional facial appearance with enhanced balance in frontal and lateral views, narrower chin and softened jawline created a more refined lower face, and appropriate incisor display enhanced the patient’s natural beauty.
Discussion
The coordinated approach using maxillary and mandibular adjustments, combined with chin narrowing and mandibular contouring, addressed skeletal discrepancies and soft tissue harmony. The result was a comprehensive improvement in the patient’s quality of life and facial appearance ( Figs. 3–5 ).