29
Acne Vulgaris
• A tendency to develop moderate to severe acne can run in families.
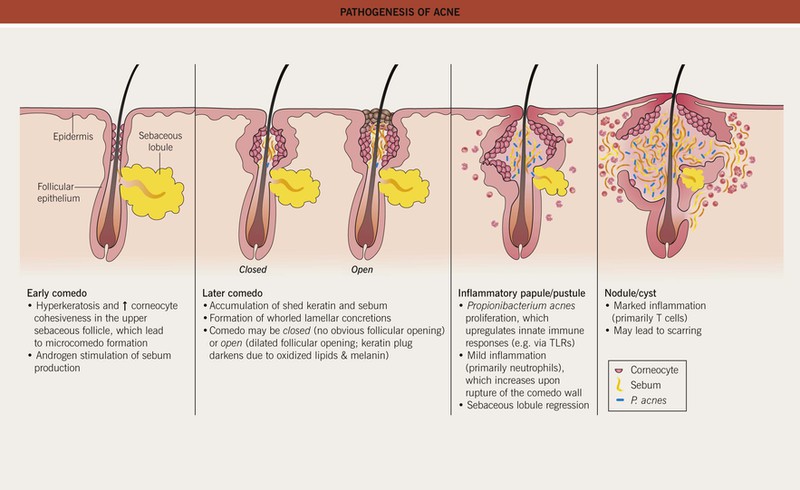
• Multiple factors affecting the pilosebaceous unit contribute to acne pathogenesis (Fig. 29.1), a process that typically begins when androgen production increases at adrenarche.
Clinical Features and Variants of Acne
• Favors the face and upper trunk, sites with well-developed sebaceous glands.
– Closed comedones (whiteheads) are small (~1 mm), skin-colored papules without an obvious follicular opening (Fig. 29.2A,B).
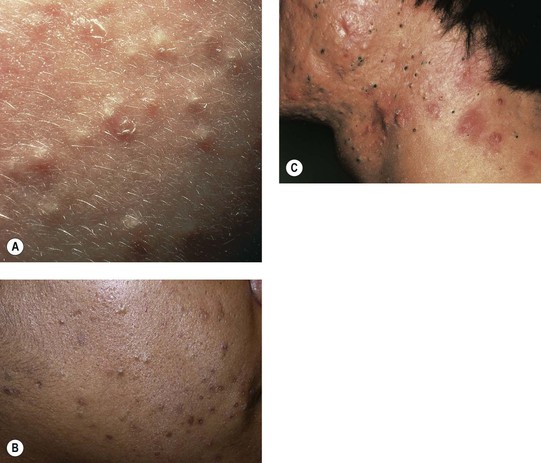
Fig. 29.2 Comedonal acne vulgaris. A Closed comedones highlighted by side lighting. B Open and closed comedones as well as post-inflammatory hyperpigmentation on the cheek. C Prominent open comedones in a patient with scarring cystic acne. A, Courtesy, Ronald P. Rapini, MD; B, Courtesy, Andrew Zaenglein, MD, and Diane Thiboutot, MD.
– Open comedones (blackheads) have a dilated follicular opening filled with a keratin plug, which has a black color due to oxidized lipids and melanin (Fig. 29.2B,C).
– Erythematous papules and pustules (Fig. 29.3A).


Fig. 29.3 Inflammatory acne vulgaris. A Papules, obvious pustules, and atrophic scars are present. B Severe nodulocystic acne. This form is best treated with low doses of isotretinoin initially (± a preceding course of oral antibiotics) to avoid precipitating a flare. A, Courtesy, Andrew Zaenglein, MD, and Diane Thiboutot, MD.
– Nodules and cysts filled with pus or serosanguinous fluid; may coalesce and form sinus tracts (Fig. 29.3B).
– Acne conglobata (severe nodulocystic acne) is classified in the follicular occlusion tetrad along with dissecting cellulitis of the scalp, hidradenitis suppurativa, and pilonidal cysts (see Chapter 31); it is also a part of pyogenic arthritis, pyoderma gangrenosum, and acne conglobata (PAPA) and pyoderma gangrenosum, acne, and suppurative hidradenitis (PASH) syndromes.
• Inflammatory acne commonly results in post-inflammatory hyperpigmentation, especially in patients with darker skin, which fades slowly over time (Fig. 29.4A); nodulocystic acne (and less frequently other inflammatory > comedonal forms) often leads to pitted (Fig. 29.4B) or hypertrophic scars (the latter especially on the trunk; see Fig. 81.4).
Acne Fulminans
• Favors boys 13 to 16 years of age.
• Coalescence into painful, oozing, friable plaques with hemorrhagic crusting, erosion/ulceration, and eventual scarring (Fig. 29.5).

Fig. 29.5 Acne fulminans. Inflamed, friable papulopustules and plaques with erosions, oozing, and formation of granulation tissue. Courtesy, Julie V. Schaffer, MD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree