9 Alveolar Bone Grafting
Introduction and Historical Perspective
Alveolar cleft repair is a critical step in the comprehensive management of complete cleft lip and palate. The first descriptions of alveolar cleft grafting likely occurred in the beginning of the 20th century.1 Subsequently, the procedure was described in the early 1960s.2,3 One decade later, Boyne and Sands described the technique used most commonly today.4 Over the past half century, modifications of early alveolar cleft repair techniques have evolved into a well-tolerated and predictable operative procedure.
Several specific problems are associated with the unrepaired alveolar cleft in association with repaired complete cleft lip and palate. These include the following:
Nasolabial and palatal oronasal fistulae
Collapsed alveolar segments
Mobile premaxilla in bilateral cleft lip and palate
Deficient bony support under the nasal ala
Loss of periodontal support for permanent teeth adjacent to the cleft site
Missing, malpositioned, malformed, and supernumerary teeth
The goals of alveolar cleft repair include the following:
Close nasolabial/palatal fistula(e) using local mucoperiosteal flaps
Restore maxillary arch continuity, including stabilization of premaxilla in bilateral cleft with cleft bone grafting
Provide bone and periodontal support for teeth in and adjacent to cleft site
Support nasal ala
Provide bone stock for dental implant replacement of missing teeth (e.g., lateral incisor)
Timing of Alveolar Cleft Repair
Although timing of alveolar cleft repair must be determined on a case-by-case basis, the timing of repair should be guided by, at one extreme (age < 5 to 6 years), minimizing the possible adverse effect that early repair may have on maxillary growth and, at the other extreme (age > 10 to 12 years), avoiding a delay of grafting until the canine is erupted or erupting. Historically, alveolar cleft repair has been performed over a wide range of ages, as reflected in published descriptions of repair timing.1 These include primary, early secondary, secondary, and late alveolar bone grafting.
Primary alveolar grafting is performed prior to age 2 years, usually in conjunction with primary lip repair, and is discussed in detail in Chapter 6. Potential advantages of primary grafting include early stabilization of alveolar segments and improved arch form. Early techniques for primary grafting involved extensive palatal dissection at the premaxillary–vomerine suture for placement of an inlay bone graft. Resultant midfacial growth disturbances led to abandonment of primary grafting in many cleft centers.5,6 Current proponents of primary alveolar repair advocate split-rib grafting with subperiosteal dissection limited to the labial alveolus, thereby avoiding the midfacial growth centers. Primary alveolar repair can achieve maxillary arch stabilization and closure of oronasal fistula with comparable success to secondary grafting.7 However, current techniques do not always obviate secondary grafting, as the quantity of alveolar bone is often insufficient for tooth eruption.8
Early secondary alveolar grafting is performed at 2 to 5 years of age. The potential for maxillary growth disturbance is similar to that found with primary alveolar grafting. However, when maxillary growth is evaluated cephalometrically, 75 to 90% of adult dimensions are achieved by age 5, suggesting that maxillary growth would not be significantly inhibited by grafting performed in the latter years of this age range.9
Secondary alveolar grafting, which is performed between 5 and 13 years of age, can be inititated at several time points, mostly based on the timing of dental eruption. Many cleft centers repair the alveolar cleft at 6 to 10 years of age, after orthodontic preparation and maxillary expansion. This is based on the historical recommendation to proceed with alveolar cleft repair when the permanent canine root is radiographically one-half to two-thirds formed. If this radiographic reference is followed, the canine crown will likely be encountered in the cleft site at the time of the operation, effectively occupying space within the cleft that should be grafted, possibly compromising access to nasal mucosa closure, and potentially compromising primary oral closure.
Timing alveolar cleft repair to canine root development also fails to consider the development and position of the permanent incisor, which is usually fully erupted by 7 to 8 years of age. Erupted permanent incisors adjacent to the unrepaired cleft site are prone to crestal bone loss and compromised periodontal support. Vertical alveolar bone height following grafting is determined by the alveolar bone height of the adjacent incisor. If grafting is performed before eruption of the incisor is complete, crestal bone height is optimized. Conversely, in the older child, if vertical bone loss has already occurred adjacent to a fully erupted incisor, alveolar height augmentation will be limited to the adjacent teeth alveolar height at the time of grafting. Preservation of alveolar bone height improves function and the periodontal health of future teeth and dental implants, as well providing an improved overall cosmetic result.10 To preserve the lateral incisor, Boyne and Sands4 advocated alveolar cleft repair at 5 to 6 years of age—much earlier than their initial recommendation of 9 to 11 years of age.11 Hall and Werther also advocated alveolar cleft repair at age 5 to 6 years to optimize bone support for the erupting or erupted central incisor well in advance of eruption of the permanent canine.12
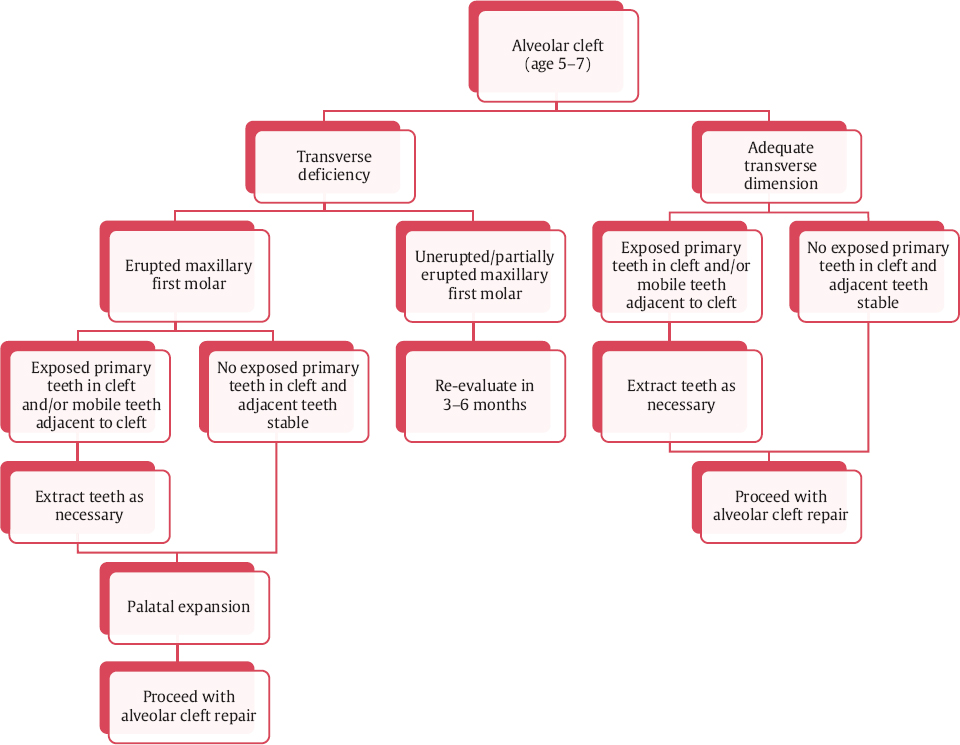
Timing of alveolar bone grafting may also be influenced by the status of maxillary permanent first molar eruption. As will be seen, many alveolar clefts require palatal expansion prior to repair. The presence of the maxillary permanent first molar allows the orthodontist to place a tooth-borne palatal expansion device. Therefore, it is often helpful to time expansion with the eruption of the maxillary permanent first molars, occurring at approximately age 6 to 7 years. Apart from the status of first molar eruption, children at this age have typically started school and are much more cooperative with orthodontic care than preschool-age children. For children with adequate transverse maxillary dimension, the eruption status of the maxillary permanent first molar has no bearing on timing of repair. In this situation, one may consider grafting as early as age 5.
Finally, children in the 5 to 7 years age range tolerate alveolar cleft repair very well, particularly with regard to iliac donor site morbidity.12
Late alveolar grafting, performed after age 13 years, is occasionally necessary in the teenager or young adult whose alveolar cleft has not been repaired at an optimal age or if earlier repair has been inadequate or failed. Late repair is associated with greater risk of complications such as infection, wound breakdown, and graft loss.13,14 Certainly young adults tolerate less well the temporary morbidity associated with the iliac donor site.13,15 Therefore, for a number of reasons, alveolar cleft repair at age 5 to 7 years is considered the optimal time for cleft repair.
Evidence-based Support for Timing of Alveolar Cleft Repair
The authors’ recommend timing of repair is 5 to 7 years of age, which attempts to mitigate the limitation of insufficient alveolar bone volume in many primarily grafted patients and the higher risk of complications in older patients. Primary alveolar bone grafting performed using a split-rib technique with limited maxillary dissection predictably restores maxillary continuity in up to 90% of patients without maxillary growth restriction seen in early primary grafting techniques (level IV evidence).7 However, this technique does not obviate the need for additional alveolar bone grafting in at least 10% of patients. Bone grafting prior to eruption of the canine results in improved marginal bone height, alveolar esthetics, and function (level II evidence).10 With level II evidence, repair after age 13 years is associated with an increased failure rate.14 Only level IV data exists in support of late secondary alveolar bone grafting,11,12,16 and we are not aware of any studies demonstrating improved outcomes over secondary grafting. Finally, younger patients recover quickly from alveolar cleft repair, with low donor site morbidity (level IV evidence).12
Patient Evaluation
Evaluation of the child with an alveolar cleft begins with a history of previous cleft surgeries and a detailed clinical examination. It is imperative to properly evaluate the dentition adjacent to and within the cleft. Imaging of the dentition adjacent to the cleft is an important adjunct to the clinical examination, and typically a panoramic radiograph is adequate. Imaging must be carefully correlated with physical examination to help differentiate primary, permanent, and supernumerary teeth. Cone beam computed tomography (CT) imaging provides three-dimensional visualization of the cleft site and the developing dentition with a trivial increase in radiation exposure versus panoramic radiographs. Although this information can be beneficial, a medical-grade CT, with associated higher radiation exposure, is not recommended in children at the optimal age for alveolar cleft repair.
Mobile primary teeth, exposed supernumerary teeth, and/or exposed permanent lateral incisors within the cleft should be extracted 6 to 8 weeks prior to alveolar cleft repair. Discovery of erupting teeth on the palatal aspect of the cleft site at the time of surgery can make palatal soft tissue closure challenging, if not impossible. Unexposed supernumerary teeth and/or malformed permanent lateral incisors in the cleft site may be extracted at the time of alveolar cleft repair. Dental arch form, degree of arch collapse, crossbite malocclusion, and position of the premaxilla in a bilateral cleft should be noted. The size of the cleft and fistula should also be noted. It is not unusual to see residual palatal fistulae in the area of previous palate repair that should be addressed at the time of the alveolar cleft repair. Such residual palatal fistulae in bilateral cleft can be challenging to repair and the challenge is proportionate to the size of the palatal fistula.
The periodontal health in the region of the cleft is an important factor in fistula repair and successful alveolar bone grafting. Friable and inflamed mucosa is prone to dehiscence in the postoperative period. Such friable mucosa is much more common in the older child with eruption of the central incisor and alveolar bone loss on the cleft side of the tooth.16 Measures to improve oral hygiene and gingival health must be initiated in the weeks preceding cleft repair. Further, if a palatal expansion device has been in contact with palatal mucosa prior to alveolar cleft repair, the mucosa will be extremely friable and unreliable in repair of the palatal fistula. Such appliances should be removed 3 to 4 weeks prior to surgery to permit resolution of any palatal inflammation. In these situations, the expansion can be maintained with an appliance that can be removed for cleaning and oral hygiene. Completely tooth-borne appliances can be removed at the time of the cleft repair with assurance that underlying palatal mucosa will be unaffected by the presence of the appliance. Such appliances can be replaced at the completion of the alveolar cleft repair to maintain palatal expansion as the alveolar graft is consolidating.
Orthodontic Preparation
Presurgical orthodontic preparation is indicated in the majority of cases prior to alveolar cleft repair. The principle goal of orthodontic therapy at this stage is palatal expansion, which improves the dental arch relationships prior to grafting and improves surgical access to the alveolar cleft. In unilateral cleft alveolar deformities, the lesser segment is typically collapsed medially, as is the anterior portion of the greater segment, but to a lesser extent. Maxillary expansion can reduce or eliminate crossbite while enhancing surgical access for the closure of the nasal floor. Caution should be exercised to limit the amount of expansion in the subset of patients with bilateral cleft with a large palatal fistula. Excessive palatal expansion in these cases will make closure of the palatal component of the fistula with standard palatal mucosal flaps very difficult, if not impossible. Palatal closure will be particularly challenging if, in addition to excessive palatal expansion, the premaxilla is simultaneously flared labially to correct an incisor crossbite. Expansion typically occurs over 4 to 6 months.17 Following grafting, the palatal expansion appliance should remain in place for an additional 3 months during graft consolidation.
Although most orthodontists and surgeons prefer preoperative orthodontic palatal expansion, postoperative expansion is an acceptable alternative. In such instances, the grafted site is allowed to consolidate for 8 weeks prior to placement of the expansion appliance. Proponents contend that postoperative expansion places the grafted site under a dynamic load during healing, which may improve bone consolidation.18 Additionally, there is a narrower defect at the time of surgery, which requires less bone graft volume, and more importantly, in the case of bilateral cleft, greater ease in closure of the palatal mucosa. If postgrafting orthodontics is preferred, the expansion appliance can be made prior to surgery, eliminating the need for postoperative dental impressions. The grafted and unexpanded cleft that is allowed to completely consolidate will be more difficult to expand, and therefore expansion should be initiated prior to graft consolidation, or prior to 3 months postgrafting.
As has been described, alveolar clefting is associated with a number of dental abnormalities. These include hypodontia, delayed eruption, supernumerary teeth, and tooth malposition. Rotation and tipping of the permanent central incisor into the cleft is very common and can compromise access to the cleft. Malposed teeth adjacent to the cleft should be managed conservatively as there is usually very little bone on the cleft side of the incisor and orthodontic tooth movement may compromise the limited bone support. Loss of this thin but critical bone will lead to root exposure, loss of alveolar height, and even tooth loss. Therefore, necessary orthodontic manipulation of the permanent incisor should be limited prior to grafting. Integration of orthodontic treatment and tooth extraction(s) in preparation for cleft repair is summarized in Fig. 9.1 .
Surgical Technique
Alveolar cleft repair involves both closure of the oronasal fistula and reconstruction of the alveolus with bone graft interposed between the nasal and oral mucosal layers. Successful alveolar cleft repair requires mobilization and tension-free closure of nasal and oral mucosal flaps. Complete graft coverage is critical to the success of the graft and is accomplished by the advancement of a keratinized buccal mucoperiosteal flap from the lesser (cleft side) maxillary segment. Advancement of unkeratinized mucosa, although possibly an expedient measure, is strongly discouraged. In particular, the so-called mucosal finger flap brings bulky, poorly keratinized mucosa into the crest of the alveolus. Finally, as noted previously, the anticipated crestal bone height will only be as high as the alveolar bone level of adjacent teeth. Placing bone graft beyond this level will not result in additional alveolar bone height; rather, it will lead only to unnecessary tension with closure of the mucosal flaps.
The gold standard for alveolar grafting remains particulate autogenous bone, usually harvested from the anterior iliac crest. Alternative graft sources are available and are described later in this chapter.
Patient Preparation
Following induction of general anesthesia, nasoendotracheal intubation is preferred. Care must be taken to avoid trauma to pharyngeal flaps as a number of children at the age of alveolar cleft repair will have undergone some form of secondary speech surgery procedures for velopharyngeal insufficiency. The authors prefer to place a small red rubber catheter over the end of the endotracheal tube in order that the soft catheter tip may be navigated atraumatically through the pharyngeal port with the endotracheal tube following. It is preferable to intubate the noncleft naris as the endotracheal tube will depress the nasal floor into the cleft and limit the volume of graft placed. In bilateral cases, either nasal or oral intubation may be used, although oral intubation will often compromise access to the palatal component of the cleft. In anticipation of grafting in a nonsterile environment, contaminated by nasal flora, prophylactic antibiotics are administered and continued for 3 to 5 days postoperatively. A single preoperative dose of dexamethasone is given to minimize postoperative swelling.
In anticipation of an anterior iliac crest harvest, the donor site is marked, prepped, and draped. A second sterile drape is applied that will be removed when the surgical team is ready to harvest the bone graft. If a second surgical team is available, the iliac crest graft may be harvested concomitantly with preparation of the cleft site. If there is any question regarding the ability to achieve primary closure and the volume of graft needed, it is preferable to complete the cleft exposure and nasal mucosa closure prior to harvesting the graft.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








