8 Nasal Perforation and Septal Prosthesis
Summary
Surgical repair of a nasal septal perforation is a complex situation for which many different techniques have been described in this book. This suggests that there is no single ideal procedure. Nonsurgical closure of nasal perforation can be achieved with a simple technique inserting a preformed or a custom-made prosthesis. Not all patients tolerate the presence of a nasal foreign body; however, many find it more acceptable than their symptoms before insertion of the obturator.
8.1 Anatomy
The nasal septum divides the nose into two similar halves. The majority of the anterior septum is made up by the quadrangular cartilage. The posterior aspect of the septum is predominantly bony and includes the perpendicular plate of the ethmoid bone superiorly and the vomer inferiorly. The nasal septum might present deviation or other deformities that should be taken into account given that it could complicate the adaptation of a nasal prosthesis in a septal perforation.
8.2 Indications
Symptomatic small and large nasal septal perforations.
Patients with contraindication for surgical approach to repair the perforation.
Patients who refuse further surgical approaches.
The perforation must have a complete circumferential ridge of nasal septal tissue around the perforation to support the prosthesis.
8.3 Materials
Tolerance of nasal septal prosthesis may be influenced by the type of material. The initial nylon and Luxene prosthetics have been replaced by more biocompatible silicone elastomer and acrylic ones. 1 Silicone currently constitutes most prefabricated prosthetics—as seen in 20 (87%) of 23 of this systematic review’s case series—whereas acrylic prosthetic outcomes were presented in only one case study, involving a custom, two-piece, magnetized heat-processed acrylic resin. 2 It has been theorized that acrylic may be the preferred material as silicone’s porous structure may sorb comparably more mucus, leading to greater crusting, surrounding tissue irritation, and patient discomfort. It has been proposed that silicone may deteriorate more over time than acrylic due to its lesser inherent physical strength. 3
However, these speculations are unable to be assessed at the present time due to the paucity of data on acrylic prosthetics. Prosthetic construction may influence patient comfort and symptom improvement. There are prefabricated prosthetics models in one and two pieces. The two-piece models may facilitate insertion by the surgeon and regular cleaning by the patient. Though this cleaning offers the advantage of less crust accumulation on the prosthetic, there are reports of patients discontinuing their use due to difficult reinsertion after cleaning. 4
8.3.1 Prefabricated versus Custom Made
In a recent review no studies were found directly comparing prefabricated prosthetics with custom-made ones. 1 In general, custom-made prosthetics are the preferred choice for symptomatic perforations of large size (≥2 cm), posterior or basal location, or irregular edges. 4 , 5 , 6 The mentioned characteristics increase the likelihood of an imprecise fit, which may contribute to greater crusting, nasal obstruction, foreign-body sensation, mucosal necrosis, prosthetic migration, and prosthetic loss. 1 Septal defect can be outlined using aluminum foil, blotting paper, or measured by computed tomographic (CT) scan to design the custom-made prosthetic. With these techniques, personalized prosthetics can accommodate variations in septal thickness better than prefabricated prosthetics and are comparatively more fixed in place by their contour. These features theoretically minimize crust buildup, which can be further reduced by using removable custom prosthetics, such as those described by Blind et al or magnet-attached two-piece prosthetics. 7 The main limitation of custom prosthetics is that they require a prosthetist to construct them, leading to longer operative times and greater costs than prefabricated prosthetics.
8.4 Surgical Steps
Positioning of nasal prosthetics can be performed under local or general anesthesia, but generally local anesthesia is preferred. In this chapter we illustrate one of the possible methods to place a conventional one-piece Silastic button.
Topical nasal decongestion and anesthesia. Infiltration of the anterior septum, floor of the nose, and surroundings of the perforation with a solution of lidocaine and epinephrine (1:100.000) to achieve correct homeostasis and anesthesia.
Ensure to de-crust the edges of the perforation meticulously to expose it completely.
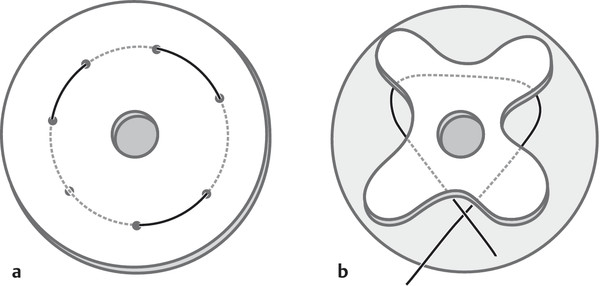
The perforation can be measured by placing a template (e.g., a piece of card or white paper) on the one side and marking the perforation from the other side. The template should be correctly placed against the nasal septum. A cotton swab dipped in methylene blue can be used to mark the shape and size of the perforation, so that a bespoke button can be shaped to the individual septal perforation 8 (Fig. 8‑1).
Carefully remove the card from the nasal cavity and cut the dyed part to assess the real size of the septal perforation. Then place it over the septal button as a template. Disks may be trimmed but must remain larger than the perforation, so cut the septal button (silicone Silastic button) around the marked perforation area leaving an appropriate margin (3–5 mm beyond the edge of the nasal perforation) (Fig. 8‑2).
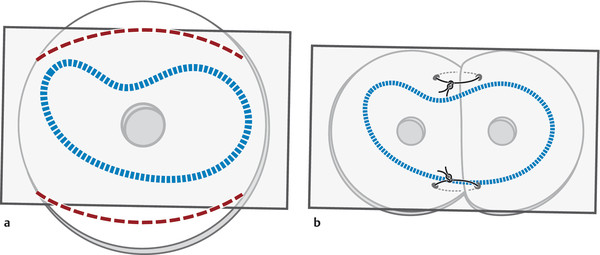
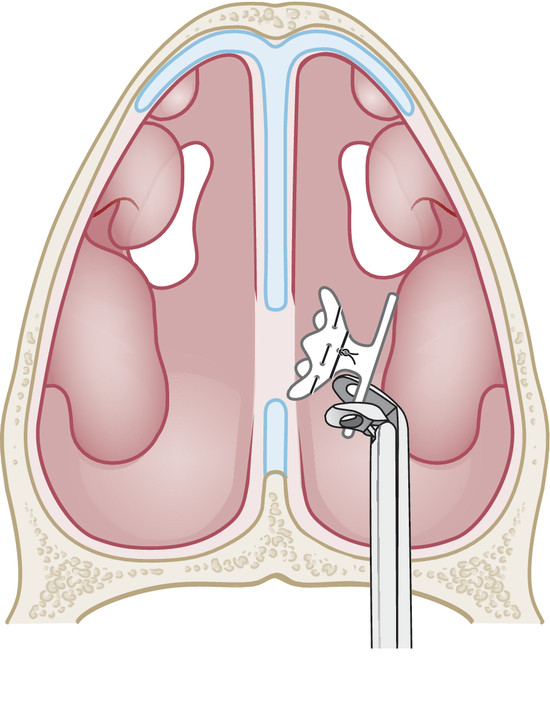
To make easier the insertion of the septal button, use a purse-string suture technique with 2–0 silk suture to collapse one disk of the Silastic obturator with approximately 8-mm spaces between each puncture site (Fig. 8‑3a), as described by Kelly and Lee. 9
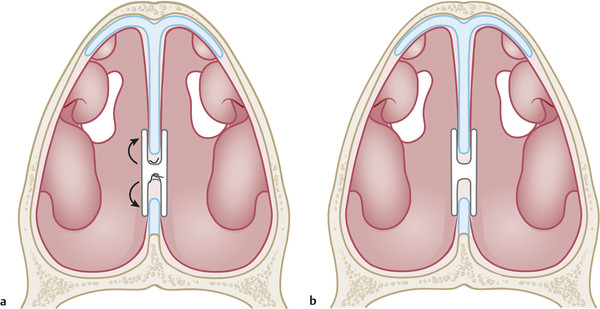
Tie the suture and the Silastic disc will fold over itself. The silk suture is then looped around the folded flange and a second knot is tied, which further collapses the disk (Fig. 8‑3b).
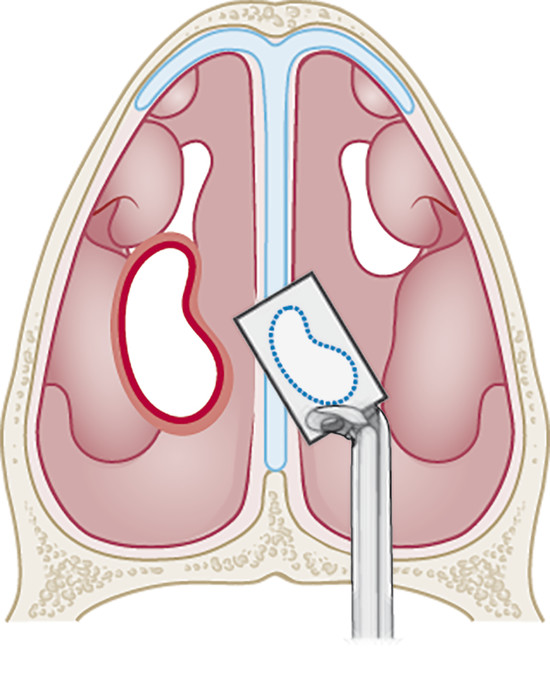
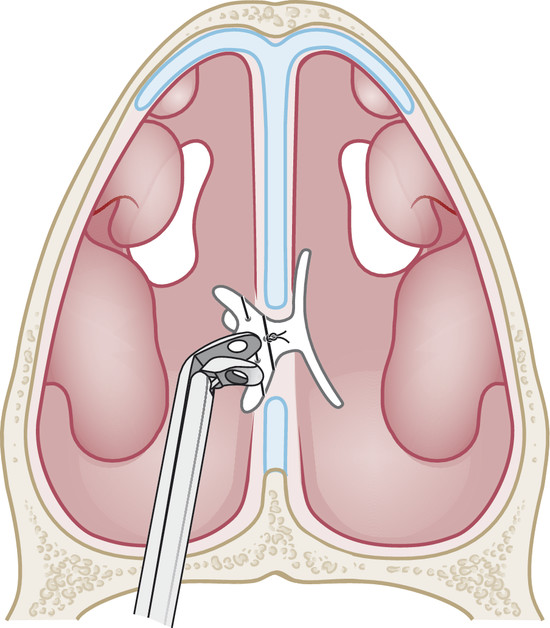
Lubricate the button. The other disk of the Silastic button is then grasped with forceps and introduced into one nasal cavity. The collapsed disk is advanced through the septal perforation under direct headlight illumination or endoscopic ally (Fig. 8‑4).
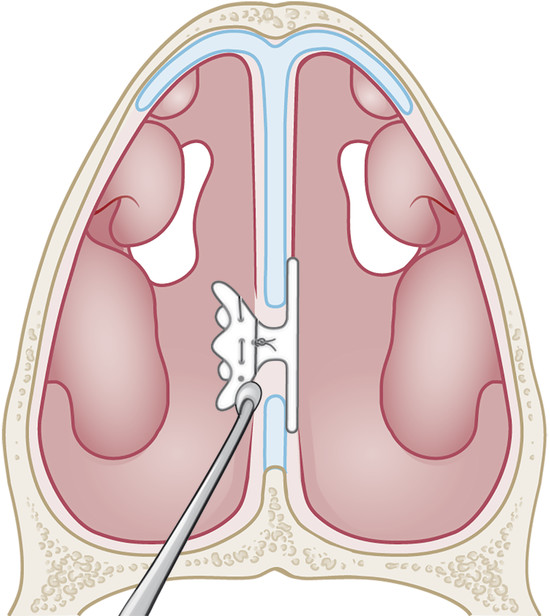
Grasp the folded flange of the septal button with a clamp through the contralateral side and pull to fit it into the septal perforation (Fig. 8‑5). Once in place, the suture is cut allowing the Silastic disk to fold out and return to its original shape (Fig. 8‑6, Fig. 8‑7a, b).
Ensure the flanges fit against the upper lateral cartilage–septum junction, and avoid pressure against the septal floor.
Thomas et al 10 described a different insertion technique: performing a circular slit starting from the outer edge of one of the flanges of the one-piece septal button. The slit goes in toward the hub covering 300 degrees of the circle of the flange. Then split end of the flange is pulled through the perforation into the other nasal cavity. By rotating the button, all of the flange will be in the other nostril, and thus the button will be positioned accurately.
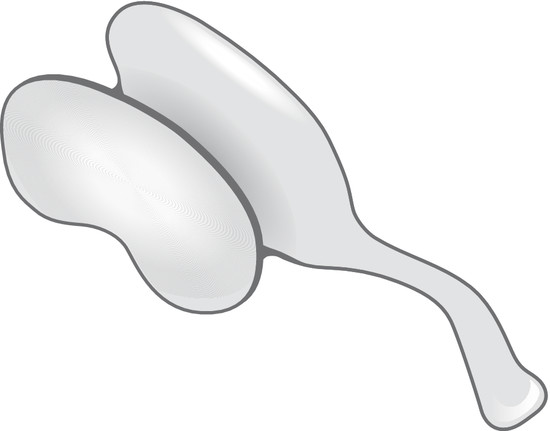
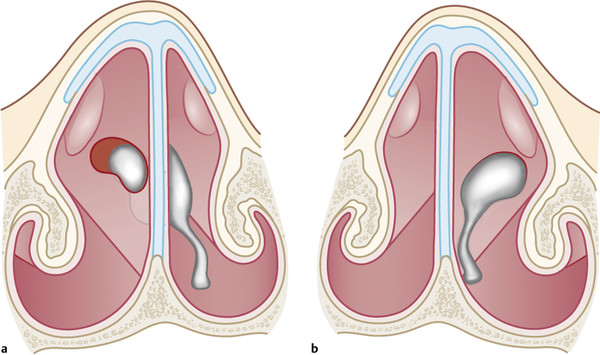
Blind et al 4 described this custom-made nasal septal silicone prosthesis. The shape of the prosthesis is made from an alginate mold, an adequate material to give a very detailed template and delicate with the sensitive nasal mucosa (Fig. 8‑8). The prosthesis is grasped from the handle and introduced from one side and fit into the nasal septal perforation with little discomfort because of the soft and elastic material. The central part of the button is thinned down to maximize breathing through the nose. When in place, the handle will be hidden under the alar dome (Fig. 8‑9a, b). This system allows the patient and the physician to remove and reinsert the prosthesis easily. The main disadvantage is the technical difficulty of molding the prosthesis, as it usually requires cooperation of a dental prosthetist and specialized materials.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree