Fig. 1
A clinical photograph of a bilateral brachymetatarsia of the fourth (Reprinted with permission from the Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore)

Fig. 2
A clinical lateral photograph of a bilateral fourth brachymetatarsia. Note the dorsally displaced fourth toe (Reprinted with permission from the Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore)

Fig. 3
Anteroposterior pre-operative view left foot radiograph of a short fourth metatarsal. Note the abnormal fourth metatarsal length while the length of the distal, middle, and proximal phalanges of fourth toe are abnormally short compared to the fifth toe. This indicates that brachymetatarsia is a ray deficiency (Reprinted with permission from the Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore)

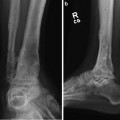
Fig. 4
Anteroposterior pre-operative view right foot radiograph of a short fourth metatarsal. Note the abnormal short fourth metatarsal length while the length of the distal, middle, and proximal phalanges of fourth toe are also abnormally short compared to the fifth toe. This indicates that the radiographic projection of a dorsally extended toe distorts the measurement of the true phalangeal length, which must be taken into consideration (Reprinted with permission from the Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore)
3 Preoperative Problem List
Short fourth metatarsal
Toe extension deformity
4 Treatment Strategy
The metatarsal-phalangeal joint (MTPJ) is at risk for subluxation and compression during gradual lengthening of a metatarsal. With greater amounts of lengthening, the joint is more susceptible to subluxation and post-operative stiffness. In addition, the closer the osteotomy is to the joint, the greater the forces; thus, a proximal metaphyseal-diaphyseal junction osteotomy is preferred. Although pinning the digit to the metatarsal head stabilizes the MTPJ during lengthening, pinning creates mild to severe post-operative MTPJ stiffness regardless of the length of time the pin is maintained. My technique was devised to prevent post-operative subluxation, stiffness, and chondrolysis of the metatarsal-phalangeal joint by applying a second external fixator to distract the MTPJ. I present a percutaneous metatarsal lengthening technique for correction of a short metatarsal deformity (brachymetatarsia ). In addition, I present a systematic technique to ensure the proper plane and vector of metatarsal lengthening to maintain anatomic sagittal and transverse plane metatarsal alignment, respectively.
5 Basic Principles
The goals of metatarsal lengthening are to decrease pain, restore the metatarsal parabola, improve foot function for gait and stance, allow for a greater selection of shoe gear, and improve the cosmetic appearance of the foot. Frequent follow-up visits are important until the patient understands the fixator, and utilizing a patient educator is extremely helpful. Be vigilant during the lengthening phase of treatment to avoid complications. Do not over lengthen beyond the metatarsal parabola (never sacrifice function for length). Lengthening 0.5 mm per day has been a successful rate of adult and adolescent metatarsal lengthening. Educate the patient pre-operatively about length of latency, distraction, and consolidation phases of treatment. Advise the patient about expectations of lengthening (lengthening may still result in a disproportioned length of the toe despite a longer toe, increased width of the foot post-operatively, stiffness or limited toe motion, interphalangeal joint contractures, and skin scarring due to pin drag) (Lamm 2007, 2010; Lamm and Gourdine-Shaw 2010; Davidson 2001; Fox 1998).
6 Images During Treatment
See Figs. 5, 6, 7, 8, 9, 10, 11, 12, 13, and 14.
Fig. 5
Anteroposterior view radiographic measurements provide pre-operative planning (Reprinted with permission from the Rubin Institute for Advanced Orthopedics, Sinai Hospital of Baltimore)