6 Primary Cleft Rhinoplasty and Gingivoperiosteoplasty
Introduction and Historical Perspective
The goal of all cleft surgeons is to create normal form and function of the lip, nose, and palate while minimizing the amount of morbidity, negative psychosocial impact, and the number of surgical procedures. Two controversial surgical interventions in many cleft protocols include primary cleft rhinoplasty and gingivoperiosteoplasty (GPP). Debate over the utility of these procedures includes dentoskeletal growth and development, potential complications, potential cost savings, and, ultimately, appropriate best practices for addressing the cleft nasal deformity and alveolar clefts. Advocates for these procedures believe early restoration of symmetry and function minimizes deformity during the formative years and decreases the need for secondary procedures.1
Primary Cleft Rhinoplasty
Primary cleft rhinoplasty, although present in many forms, is the surgical manipulation of the soft tissue and nasal cartilages with or without skin incision, often using suture suspension, nasal bolsters, or nasal stents at the time of cleft lip repair. This allows for early repositioning of the dysmorphic lower lateral cartilages to create a symmetric nasal tip and nasal base. Although there have been many primary cleft rhinoplasty techniques described over the years, McComb and Coghlan2 were among the pioneers of the field.3,4 Early techniques often led to significant scarring, nasal stenosis, and unstable results.5 Over the years, however, reconstructive strategies have evolved to optimize outcomes. Opponents of primary rhinoplasty are concerned by the potential for nasal growth restriction and scarring, making revision cleft rhinoplasty more difficult.1 Many surgeons advocate that despite these risk factors, primary rhinoplasty lessens the secondary cleft nasal deformity and can avoid the negative psychosocial impact of the untreated cleft lip nasal deformity as the child matures.1,6,7 McComb and Coghlan followed their first 10 patients who received a primary cleft rhinoplasty for 18 years and found no significant difference in nasal or midfacial growth compared to normal controls. They also noted that the symmetry produced during primary rhinoplasty was maintained into adulthood.2 Definitive rhinoplasty is often required after skeletal maturity has been reached. However, primary rhinoplasty reduces the number of revision procedures required, if any at all.1 Presurgical nasoalveolar molding (NAM) can aid in successful primary rhinoplasty, as covered in Chapter 2.8
Gingivoperiosteoplasty
GPP is the surgical repositioning of the mucosal edges of the two sides of an alveolar cleft, promoting bone formation in the cleft. Alveolar clefts involve deficiency or the absence of bone in the primary palate, extending from the nasal sill to the incisive foramen. Alveolar clefts can range from mild notches to complete absence of bone, and may occur with or without a cleft of the secondary palate ( Fig. 6.1 ). Failure to repair the alveolar cleft can allow collapse of the maxillary arch, inhibit dental eruption, and negatively affect facial growth and symmetry. Alveolar clefts can be repaired with GPP or alveolar bone grafting (the latter is discussed further in Chapter 9). The goals of GPP are as follows9:
Bony continuity of alveolar arch
Alignment and stabilization of the anterior maxilla
Good alar base support with nasal symmetry
Elimination of oronasal fistula and mucosal recesses
Spontaneous eruption and maintenance of permanent dentition into and adjacent to the cleft alveolus
Prevent the need for secondary alveolar bone grafting and associated morbidity
GPP has been described as a “boneless bone graft” as it does not require autologous bone from a donor site ( Fig. 6.2 ).10 This technique relies on the osteogenic potential of periosteum to generate osseous continuity across the alveolar cleft in young patients. A mucoperiosteal bridge is created across the alveolar cleft with bone generation occurring inside the subperiosteal tunnel.10,11 Skoog10 was the first to describe indirect GPP in 1965. The lingual and labial sides of the wide alveolar cleft defect are approximated with a large transposition flap taken from a widely undermined maxillary periosteum. Although he was able to produce bony continuity and stabilization of the maxillary arch, there were significant concerns about adverse effects on facial growth from extensive subperiosteal dissection at the flap donor site.
With multidisciplinary collaboration, presurgical infant orthopedics (PSIO) were introduced and popularized, allowing for alignment of the alveolar segments and narrowing of the alveolar cleft prior to surgical repair. There are two types of PSIO: active and passive. Active devices are attached to the maxillary skeleton and require daily turning of a screw to adjust the tension, thereby retracting the premaxilla and expanding the alveolar segments to move the maxillary arch into proper alignment. Passive appliances modulate external forces to mold the alveolar arch into alignment.3,12,13
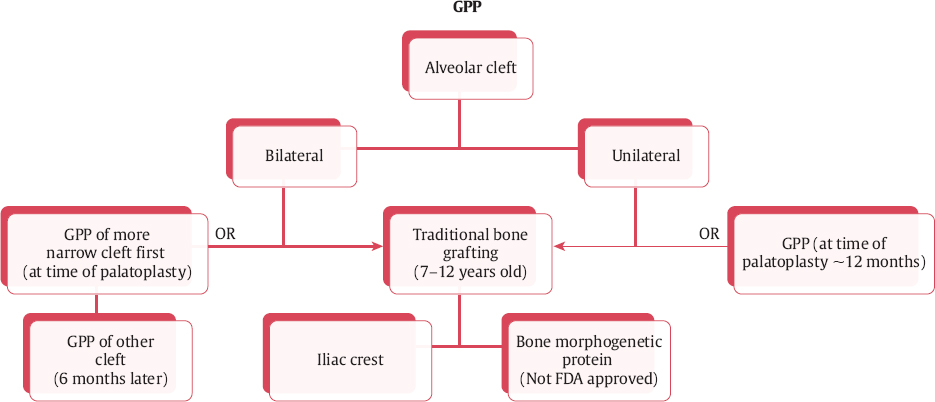
In 1978, Millard14 introduced the presurgical orthopedics, gingivoperiosteoplasty, and lip adhesion (POPLA) protocol in which an active PSIO, the Latham device, was utilized to narrow and align the alveolar cleft segments. In comparison to Skoog′s indirect GPP for a wide alveolar cleft, Millard was then able to perform a more conservative direct GPP and lip adhesion at 3 to 4 months of age. By narrowing the alveolar cleft with PSIO, Millard′s technique of direct GPP required less subperiosteal dissection to close the defect, resulting in increased viability of the mucoperiosteal flaps and presumably less risk to facial growth.15 Success of Millard and Latham′s POPLA protocol varied with the requirement of a secondary alveolar bone graft (SABG) ranging from 3 to 72% of patients.14,16,17 Over the years, multiple studies have suggested that the POPLA protocol results in maxillary growth restriction as well as anterior crossbite.14,17–20 It is unclear if the Latham device or the GPP caused the reported growth restriction.
In response to this and a desire to reduce primary nasal surgery, Grayson and Cutting21 introduced a new protocol utilizing NAM. This protocol employs passive PSIO to narrow and align the alveolar segments prior to GPP and lip repair, rather than the active PSIO of Millard′s POPLA protocol. Additionally, the nasal tip is elevated and the columella is lengthened. Subsequent studies have shown no restriction of maxillary growth and excellent bone production with maximum follow-up to 11.5 years of age.22–25 Sato et al.26 found that 73% of patients had adequate bone growth after GPP, avoiding a SABG and the associated donor site morbidity. Even when GPP fails to produce sufficient bone for stable dental eruption, multiple authors have reported subsequent SABG to be technically easier6 and more successful due to the favorable environment with intact periosteum, which is completely isolated from the oral and nasal cavities.17,27
Surgical Techniques
Primary Cleft Rhinoplasty
In order to properly repair a cleft lip nasal deformity, one must understand the anatomic abnormalities associated with both the unilateral cleft lip nasal deformity and the bilateral cleft lip nasal deformity (BCLND). These are presented in Table 6.1 .
Primary cleft rhinoplasty is performed at the time of primary lip repair ( Fig. 6.3 ). Goals of the procedure include repositioning of the lower lateral cartilage (LLC) to create a symmetric nasal tip and nostrils, repositioning of the alar base, and closure of the nasal floor and sill.28 Preoperatively, NAM can be employed to create symmetry, as well as lengthen the columella and vestibular lining. The senior author′s method for primary cleft rhinoplasty is described.29 No additional nasal incisions are required as the entire procedure is performed through the lip incisions created during the primary cleft lip repair (see Chapters 4 and 5).
Unilateral Cleft Lip Nasal Deformity
A triangular “field block” is performed from the nasal radix to the oral commissures with 0.5% lidocaine and 1:200,000 epinephrine. This allows for increased hemostasis but avoids distortion of the anatomic landmarks of the nose and lip. The lip incisions are then marked and tattooed. With the anatomic landmarks clearly defined, the areas being dissected are then further injected with local anesthetic for maximal hemostasis. After the lip incisions have been performed, mobilization of the lip and perinasal soft tissues is performed to allow for proper positioning of nasal ala. The lateral lip segment is completely released from the underlying piriform aperture by dissecting in the supraperiosteal plane from the vestibular sulcus incision up to the root of the inferior turbinate. Blunt dissection of the lateral lip segment off the maxilla allows for further release of the soft tissue and adequate repositioning of both the lip and alar base. The lateral lip segment skin is dissected from the orbicularis muscle out to the junction of the alar and melolabial creases. The medial lip segment skin is elevated from the orbicularis oris muscle.
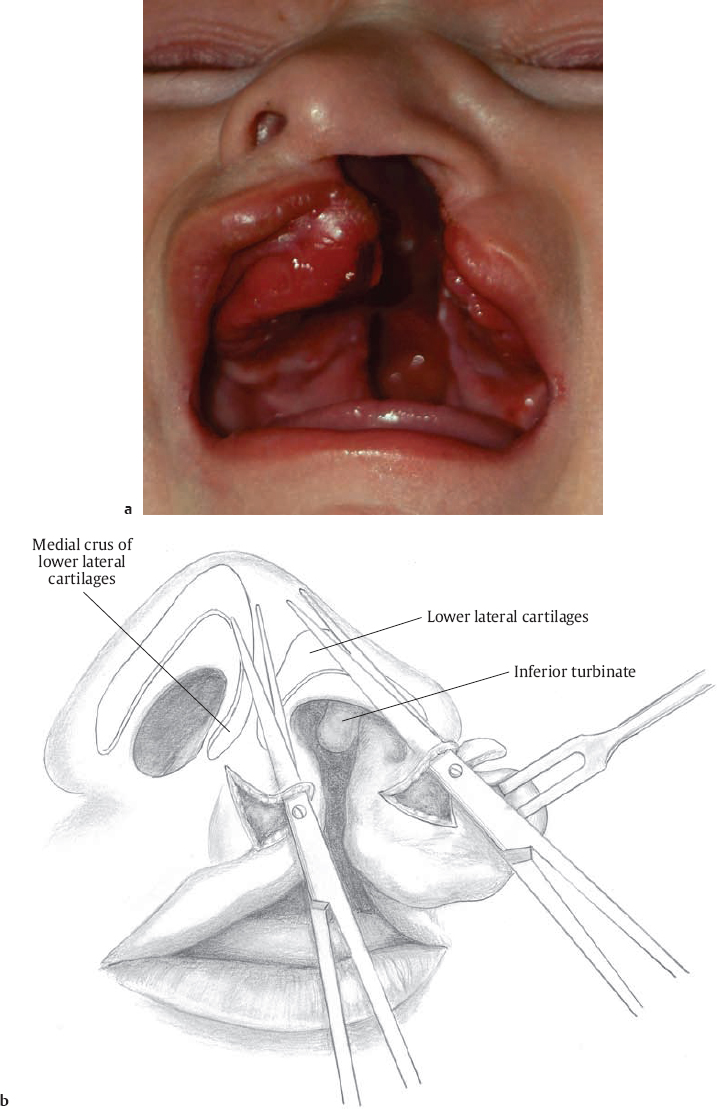
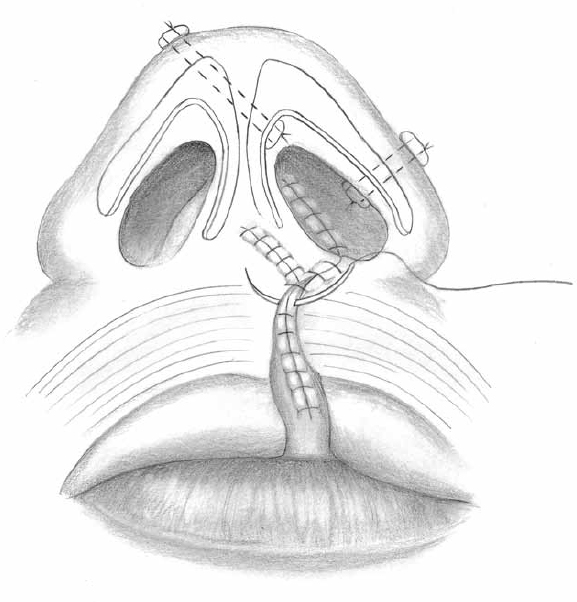
Mobilization of the cleft-side LLC from the overlying nasal skin–soft tissue envelope is then performed. Tenotomy scissors are advanced through the medial cleft margin incision into the columella ( Fig. 6.1 ). Dissection occurs between the medial crura and is carried superiorly to the nasal tip. The scissors are then repositioned laterally through the lateral lip incision and dissection is continued in the soft tissue of the nasal ala until the LLC is encountered. Using palpation and visualizing the skin of the nasal tip, the external nasal skin is elevated off the dorsal surface of the cleft-side LLC and upper lateral cartilage, then carried medially to join with the intracolumellar dissection area. At this point, the malpositioned LLC is freed from the overlying skin envelope. To prevent a narrow nostril size on the cleft side, excess fibrofatty tissue is removed from the lateral ala, taken from the same dissection as the scissors above (see Fig. 6.1 ). This excess tissue bulk otherwise causes intrusion of the lateral crus into the vestibule. The cleft-side nasal dome is then repositioned using a lateral crural steal technique—elongating the medial crus by stealing from the lateral crus of the LLC—to improve symmetry and projection of the nasal tip (see Fig. 10.9).
Nasal bolsters are used to suspend the cartilages into the new position. (At this point, some surgeons attempt to use an intracartilaginous incision to approach the cartilages, and place suture between the cartilages.) The newly positioned cleft-side nasal dome is fixated with a transcutaneous mattress suture over a bolster ( Fig. 6.4 ). A 4-0 nylon suture is passed through a Teflon (DuPont, Wilmington, DE) cardiac valve pledget, and then the needle is passed transcutaneously from the noncleft-side nasal tip, through the newly positioned cleft-side nasal dome, and into the nasal vestibule. The needle is passed through a second Teflon pledget on the vestibular surface and passed back through the cleft-side nasal dome to the contralateral nasal tip and tied over the bolster, pulling the cleft-side tip anteromedially. After this first suture is placed, a second transcutaneous bolstered suture is placed laterally along the alar-facial groove to correctly contour the lateral ala and to promote effacement of the vestibular lining to prevent narrowing.
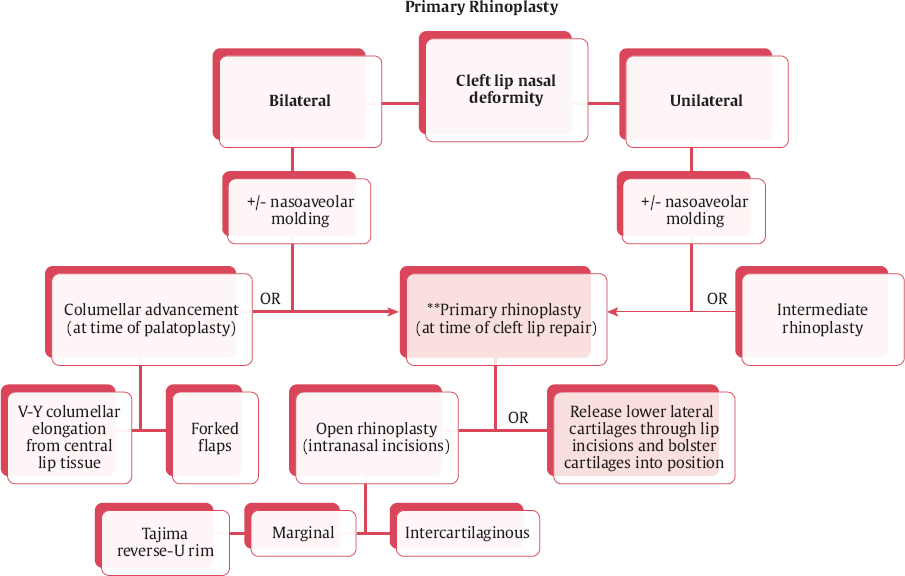
The cleft-side alar base is repositioned symmetrically with the noncleft alar base by closure of the lip mucosa and muscle layer. The nasal floor is created by precise alignment of the medial and lateral edges of the nasal sill and placement of interrupted absorbable sutures (6-0 fast absorbing gut) as far posterior as possible. Mupirocin ointment is applied to the nasal pledgets. Prophylactic postoperative oral antibiotics are utilized until the pledgets are removed in 5 to 6 days. This technique often produces a slightly larger cleft-side nostril (overcorrection), which is a “good problem” to have as cleft lip repairs are often associated with a much more difficult to correct smaller cleft-side nostril. If the asymmetry persists, a minor nasal sill excision usually corrects the problem. At the conclusion of the primary rhinoplasty, alar base and nasal tip symmetry should be improved resulting in a more projected, defined, and symmetric nasal tip.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree