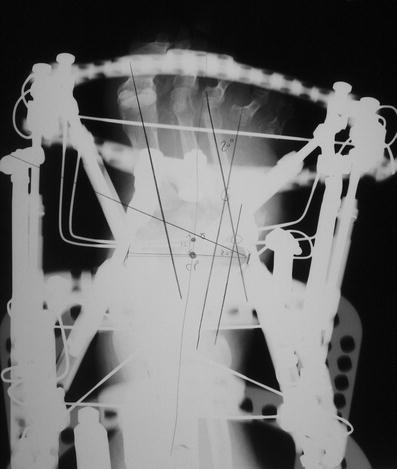
Fig. 1
A midfoot Charcot neuroarthropathy deformity (Eichenholtz stage II, unstable, with superficial plantar medial ulceration and previous resection of the fourth and fifth metatarsals). Anteroposterior view radiograph shows midfoot adduction deformity

Fig. 2
Lateral view radiograph shows rocker bottom and equinus deformities. Note the dorsal displacement of the forefoot and the break in Meary’s angle
3 Preoperative Problem List
1.
Diabetes mellitus
2.
Peripheral neuropathy
3.
Charcot neuroarthropathy of the Lisfranc and midtarsal joints
4.
Superficial plantar medial ulceration
5.
Equinus
4 Treatment Strategy
The chronic Charcot foot (i.e., Eichenholtz stage 2 or 3) can be stable or unstable. The unstable Charcot foot is difficult to shoe or brace and typically results in ulceration. The stable Charcot foot is easier to shoe or brace but is still prone to ulceration if deformity is present. The goal of surgical treatment in cases of chronic Charcot neuroarthropathy (i.e., Eichenholtz stage 2 or 3) is to establish a plantigrade foot. Achilles tendon lengthening, ostectomy, débridement, osteotomy, arthrodesis, and open reduction with internal fixation are well-known surgical reconstructive procedures aimed to reestablish the normal foot position. Acute correction via open reduction with rigid internal fixation or plantar plating is frequently used for reconstruction (Cooper 2002). Also, acute correction via open reduction with application of static external fixation has been reported (Jolly et al. 2003). Recently, a new, minimally invasive method of gradual distraction with external fixation that provides both realignment and stabilization has been presented (Lamm and Paley 2006; Lamm et al. 2010). By applying an external fixator (Taylor Spatial Frame (TSF)), dynamic gradual deformity correction and distraction can be performed, and then once the foot is in the corrected position, a minimally invasive formal fusion of the Charcot joint is performed. The surgeon then has the option of compressing through the external fixation or removing the external fixator and implanting internal fixation (intramedullary foot fixation). In this case the distraction of the forefoot on the hindfoot took 3 weeks utilizing a butt frame (TSF) external fixation device. A second stage surgery was then performed to create a formal midtarsal and Lisfranc fusion through a medial longitudinal incision with insertion of the intramedullary foot fixation screws. A non-weight-bearing short-leg cast was applied for 10 weeks.
5 Basic Principles
A common factor is equinus which is typically present with a Charcot deformity and is important to be evaluated and treated when present.
Midfoot Charcot collapse commonly occurs through the tarsometatarsal and/or midtarsal joints, which creates the characteristic “rocker bottom” deformity. The indications for Charcot reconstruction via intramedullary foot fixation are an unstable Charcot midfoot or a stable but deformed Charcot midfoot without a history of osteomyelitis.
6 Images During Treatment
See Figs. 3, 4, 5, 6, 7, 8, and 9.

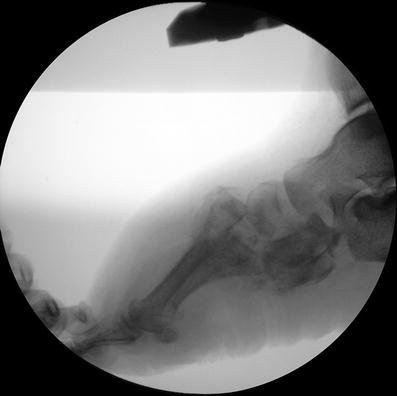

Fig. 3
The lateral view still image, obtained by using videofluoroscopy, confirms the instability of the midfoot Charcot demonstrating significant forefoot dorsiflexion
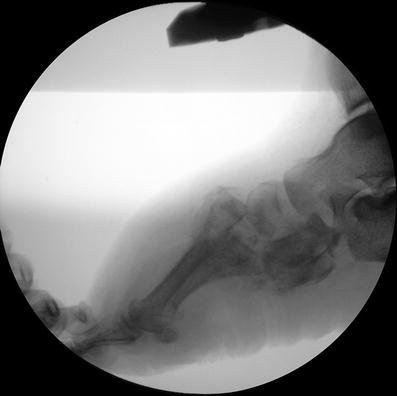
Fig. 4
The lateral view still image, obtained by using videofluoroscopy, confirms the instability of the midfoot Charcot demonstrating significant forefoot plantar flexion