5 Systemic Diseases Associated with Septal Perforation
Summary
Systemic and infectious diseases can present with nasal septum perforations (NSPs) either at the beginning of the symptomatology or along the evolution of the clinical manifestations. A meticulous medical history and a physical examination are essential for the diagnosis in these patients. Complementary testing, including laboratory, imaging, and biopsies, also has a relevant role in this pathology involving very distinct etiologies. Infectious diseases and multisystemic disorders (vasculitis and autoimmune diseases) are discussed in this chapter (Fig. 5‑1).
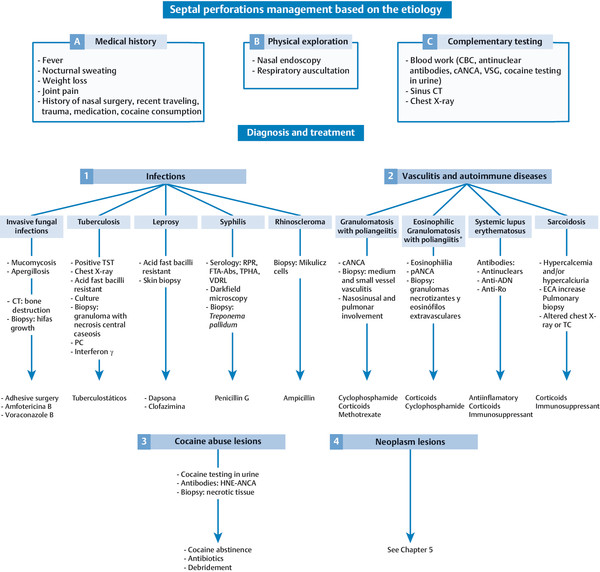
5.1 Infectious Diseases
Even though NSP is a rare manifestation of systemic or infectious diseases, multiple diseases have been related with septum perforations. It is very difficult to estimate the frequency of NSPs due to lack of information. In the following paragraphs the most frequent associated infections are described.
5.1.1 Tuberculosis
Approximately 260,000 of tuberculosis (TB) were reported between 2000 and 2011 in the United States and the United Kingdom. 1 The incidence of TB declined during these years in the United States (from 5.8 to 3.4 cases per 100,000), whereas the incidence increased in the United Kingdom (from 11.4 to 14.4 cases per 100,000). 1 The incidence of TB in Spain has been reported to be 13 cases per 100,000 habitants. 2 , 3 , 4
Mycobacterium tuberculosis is the main infectious agent causing TB. There are other atypical mycobacteria such as Mycobacterium kansasii that can also cause similar clinical and pathologic manifestations. 5 The nasal symptoms in patients diagnosed with TB are similar to a cold with rhinorrhea and nasal obstruction. 6 The most frequent affected location is the nasopharynx, characterized by adenoid hypertrophy, rhinorrhea, and cervical lymphadenopathies. If nasal polyps are observed, they usually grow predominantly from the inferior turbinate. 5
Primary nasal TB is a very rare finding. Butt revised the cases published during the 20th century and found 35 cases of nasal TB, of which only 12 were primary nasal TB. 7 It is rare for M. tuberculosis to infect the nasal mucosa nasal, because of its bactericide secretions, cilia movement, and the presence of nasal vibrissae. The main cause could be related to the inhalation of infected particles by a damaged or atrophic mucosa or by direct traumatic digital inoculation. 8 In the case of primary nasal TB, the symptomatology is usually unilateral and consists of nasal obstruction, rhinorrhea, and nosebleed when destructive lesions are present (ulcers or perforations). The most frequent location is the septum, followed by the lateral wall. 6
The differential diagnoses include malignancy processes; inflammatory granulomatosis (Wegener’s granulomatosis, sarcoidosis, leprosy, or syphilis); and viral, parasitic, or fungal infections.
The nonspecific nature of the symptoms and rareness of a nasal location usually lead to a delay in diagnosis. Although several imaging tests (computed tomography [CT], magnetic resonance imaging [MRI], and positron emission tomography–computed tomography [PET-CT]) can help delimitate the extension of the lesions, they lack diagnostic specificity.
The diagnosis should include acid-fast smear, culture, and tuberculin skin testing. With the use of polymerase chain reaction (PCR) and Xpert MTB/RIF assays for rapid diagnosis and detection of TB, treatment can be initiated earlier. 9 However, it is also important to have the biopsy samples for pathologic study and microbiologic culture, even though the results of the microbiologic culture are negative in up to 50 to 75% of cases. 5 Once the diagnosis of TB has been confirmed, the presence of pulmonary and systemic TB must be ruled out. 5 , 6 , 8
Treatment consists of anti-TB drugs, which achieve a rapid and complete response in the majority of cases. In a series of 50 cases with nasopharynx TB, all patients were disease-free 2 years after completing the treatment. 10
5.1.2 Leprosy
Leprosy is a potentially disabling disease causing deformities and physical disability due to an infectious agent. 6 In 2000 leprosy was eliminated, defined as a decrease in disease prevalence of less than 1 case per 10,000 habitants. 11 The prevalence and incidence of leprosy have remained constant since 2005, despite the existence of effective multidrug treatment. 12
Leprosy is caused by Mycobacterium leprae and is characterized by skin and peripheral nerve damage. In advanced cases it can affect the great majority of organs, including the ears, nose, and throat. 6 The nasal mucosa is affected in 95% of patients with lepromatous leprosy and in all patients with advanced states of disease. 13 , 14 The nasal symptoms range from nosebleed, thick nasal discharge, ulcerations, septum perforations to total destruction of the nasal support causing the saddle-nose deformity, palate fistula, or even cavernous sinus thrombosis, a potentially fatal complication. 6 , 14
The diagnosis of leprosy is based on clinical signs and symptoms. The observation of acid-fast bacteria in the skin-scraping examination confirms the diagnosis.
The recommended treatment of leprosy by the World Health Organization (WHO) includes dapsone, rifampin, and clofazimine. 15 The use of supervised multidrug therapy for fixed durations has been highly effective in treating all forms of the disease. 15
5.1.3 Syphilis
Syphilis is an infectious disease caused by a spirochete called Treponema pallidum that has a tropism for several organs and tissues in the body causing complex clinical manifestations. 16
In the United States approximately 6,000 cases are diagnosed each year of primary and secondary syphilis. 5 The incidence of syphilis reached an all-time low in 2000, with 2.1 cases per 100,000 persons in United States. 17 During the last 8 years a significant resurgence of this disease has been reported in several countries such as the United States, Canada, England, France, Spain, Ireland, Eastern Europe, Russia, and China. 17 It is estimated that 55,000 new infections occurred in 2014 in the United States. 17
Primary syphilis has little nasal manifestations, although few cases of nasal vestibule chancre have been reported. 5 Secondary syphilis can manifest as acute rhinitis with abundant nasal discharge with important irritation of the nasal mucosa. 18 If the disease progresses to tertiary syphilis, there is an important nasal involvement characterized by gummata of the nose, septal perforations, and destruction of the nasal support with saddle-nose and important deformity. 18 Involvement of nasopharynx is very uncommon.
The diagnosis of syphilis is based on the clinical signs and symptoms, physical examination, lesion-based test (dark-field microscopy, fluorescent antibody staining), and nontreponemal (rapid plasma reagin [RPR], venereal disease research laboratory [VDRL]) or treponemal (fluorescent treponemal antibody absorption [FTA-ABS], immunoglobulin G, Western blot) serologic tests. 19 Microorganism detection is useless for the diagnosis.
The mainstay of syphilis treatment is parenteral penicillin G. Doxycycline is an alternative in patients with penicillin allergy. 19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree