Fig. 1
AP radiograph shows an attempted tibio-talo-calcaneal (TTC) fusion

Fig. 2
Lateral radiograph shows nonunion at the tibiotalar joint and loose hardware
3 Preoperative Problem List
1.
Nonunion ankle fusion
2.
Retained hardware
3.
Leg length discrepancy
4 Treatment Strategy
1.
Pre-operative labs: CBC, CRP, and ESR
2.
Revision ankle fusion with removal of hardware
3.
Application of Ilizarov-Taylor Spatial Frame for fixation
4.
Intra-operative cultures
5.
Staged lengthening after treatment of potential infection
5 Basic Principles
All nonunions should be assessed for possible infection, and fusion nonunions are no exception. Pre-operative antibiotics were held until after cultures were taken. Medial and lateral incisions were used to access the ankle and remove the medial and lateral malleoli. The tibial and talar surfaces were recut to the level of healthy bleeding bone. The cuts were apposed to maximize surface contact at the fusion site. BMP (Bone morphogenic protein ) was added to assist with fusion. The wounds were closed and the Ilizarov external fixator was applied using two rings. Strong compression was applied across the tibiotalar fusion site. The subtalar joint was previously fused and this was therefore compressed without concern. Weight bearing as tolerated ambulation was encouraged post-operatively. Post-operative leg lengths measured a 6 cm discrepancy, and the patient affirmed that she wanted to undergo distraction osteogenesis of the tibia. Cultures were negative. A staged lengthening was performed through a proximal tibial osteotomy site 4 weeks after the fusion surgery. The distraction proceeded at 1 mm per day for 60 days. To reduce the time in the frame and improve the healing of the new bone, a locked IM nail was inserted into the regenerate bone and the frame removed after only 3 months.
6 Images During Treatment
See Figs. 3, 4, 5, 6, 7, 8, 9, and 10.

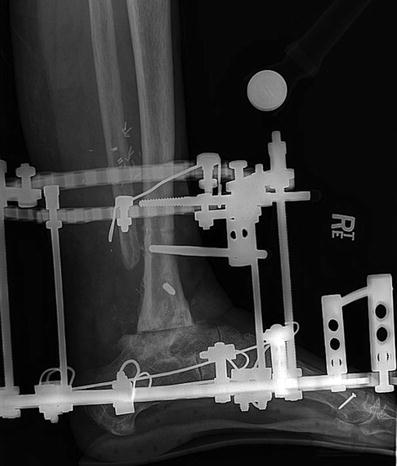





Fig. 3
The two-ring ankle fusion frame is seen with the fixation kept deliberately distal in the tibia to allow for a longer IM nail insertion later
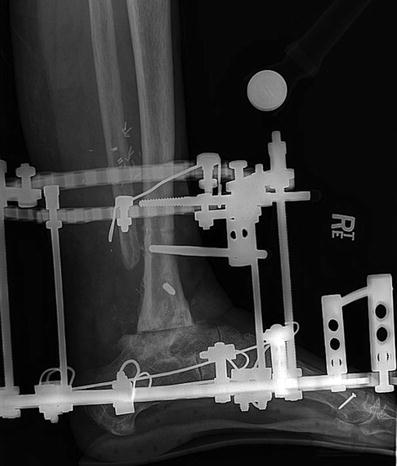
Fig. 4
Lateral view of the ankle fusion frame
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








