Cases in subdisciplines of craniomaxillofacial surgery—corrective jaw surgery, maxillofacial trauma, temporomandibular joint/skull base, jaw reconstruction, and postablative reconstruction—illustrate the ease of use, cost effectiveness, and superior results that can be achieved when using computer-assisted design and 3D volumetric analysis in preoperative surgical planning. This article discusses the materials and methods needed to plan cases, illustrates implementation of guides and implants, and describes postoperative analysis in relation to the virtually planned surgery.
Three dimensional (3D) facial analysis and virtual surgical simulation has revolutionized the way surgeons diagnose, treat, and reconstruct head and neck diseases and defects. In our modern computer era, digital planning has been the standard in architectural design, engineering, and biomedical fabrication; this trend has recently made an impact on clinical medicine and surgery. In all aspects of surgery, proper planning facilitates more predictable operations and operative results, but prior to the use of virtual planning, much of this relied on inaccurate surgical models, intraoperative trial and error, and 2-dimensional (2D) imaging. This process increases operative time, operator frustration, and postoperative inaccuracies.
The goal of this article is to illustrate the ease with which virtual surgery and computer-assisted design can be integrated into one’s armamentarium, and benefit the surgeon and the patient with more precise surgical planning, decreased operating time, and creation of accurate postoperative results compared with traditional craniomaxillofacial surgical treatment planning. At their institution, the authors have reliably achieved excellent results in corrective surgery of the jaws, maxillofacial trauma, temporomandibular joint reconstruction, skull base surgery, jaw reconstruction, head and neck oncologic surgery, and postablative reconstruction. For the 90+ cases the authors have virtually planned and completed, the cost has ranged from 2000 to 4000 dollars per case depending on the amount of templates and implants fabricated. These techniques have become the authors’ preferred method for complex craniomaxillofacial surgery and reconstruction.
Corrective jaw surgery
Orthognathic surgery is widely used in the correction of craniomaxillofacial deformities. There is a rich history of preoperative planning and evolution of surgical techniques dating back to the 1800s and, for the most part, the basis of these procedures has not changed in the last several decades. Traditional planning for correction of skeletal facial deformities is complex, and requires several sets of patient data to establish the correct diagnosis and treatment plan. Facial and intraoral photographs, lateral cephalogram, orthopantomogram, and articulated dental casts are necessary to begin this process. After evaluating the aforementioned data, most surgeons digitally or manually trace the lateral cephalogram and plan sagittal maxillomandibular movements based on correction of predefined cephalometric measurements. Correction of yaw and roll, however, can be much more difficult and generally relies on precise dental cast mounting, clinical examination, and facial/intraoral photographs. After determining the amount of correction of the maxilla and mandible in all 3 planes, “surgery” on the dental models is performed to replicate the intraoperative repositioning of the jaws, and interocclusal splints are fabricated with acrylic. These splints are essential in repositioning the jaws, especially when maxillary and mandibular surgeries are performed together, but their accuracy is dependent on several factors. Because most of these movements are in the 1- to 10-mm range, small errors and discrepancies in each step of the workup can compound and lead to inaccurate and unpredictable final results. Facebow records, interocclusal records, deformation of dental impression material, inaccurate mounting, shrinkage of acrylic splints, inaccurate placement of line markings, and small discrepancies in model surgery all lead to some degree of error, rendering the exact measurements in movement planning not totally predictive of the end result. Facebow records rely on the arc of rotation of the mandible when transferred, but the hinge axis is connected to the maxillary arm of dental articulators. Complex facial asymmetries are nearly impossible to correct in 2D planning, and many times asymmetries are induced, due to the compounding of small errors throughout the planning and model surgery process.
In an operation whereby planning in millimeter increments is so important, computer-assisted virtual surgery proves to be a valuable asset in producing more predictable results. By eliminating several sources of error, one can plan more precisely and achieve more accurate movements. The first step in this process involves acquisition of the appropriate data set. Noncontrast maxillofacial computed tomography (CT) is acquired while the patient occludes in maximum intercuspation. To ensure an accurate transfer of the patient’s occlusion to the radiographic data, a facebow bite jig is fabricated by impressing the dentition with hard-set acrylic. When set, this model provides an accurate representation of the patient’s bite. The patient is sent to the CT scanner with the jig in place and 1-mm cuts or high-resolution CT is acquired (see case 1 , Figs. 1 A and 2 A). A gyroscope is then attached to the facebow jig to measure the natural head position, yaw, pitch, and roll, thus replacing the need for facebow transfer and dental cast articulation. The CT scan, along with traditional gypsum maxillary and mandibular dental models, is sent to the desired modeling company. The dental casts are laser scanned and digitally merged into the maxillofacial CT to allow for accurate representation of the dentition without scatter artifact. Treatment planning is completed via the software using the 3D facial reconstructions of the CT scan. Accurate correction of yaw, pitch, and roll as well as midline correction and facial heights can be completed in all 3 planes of space. Using plain cephalometric films as in traditional orthognathic treatment planning only allows for two dimensional correction, whereas all other planes of space are evaluated using clinical photographs and examination. 3D cephalometry allows the surgeon to view the skeletal defects in relation to the entire facial skeleton.
Fig. 3 shows a 17-year-old otherwise healthy female referred for surgical correction of a skeletal class III occlusion and vertical maxillary excess.
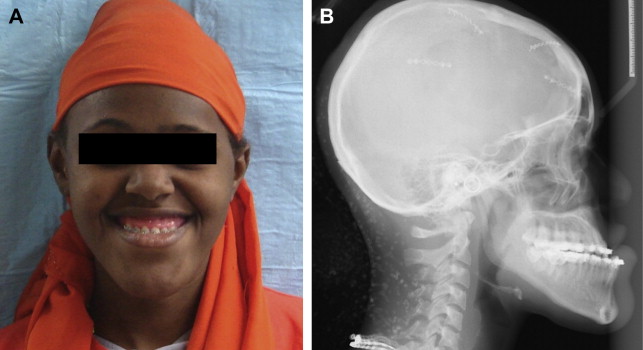
Initial steps in treatment planning as already described call for acquiring a high-resolution CT while the patient wears an interocclusal record with an acrylic facebow (see Fig. 1 A), and measuring natural head position with a gyroscopic attachment to the facebow bite jig (see Fig. 1 B). After acquisition of the CT scan (see Fig. 2 A), the laser scanned dental models are integrated into the radiographic data and the planning phase can begin. The head position as measured by the gyroscope allows for calibration of the 3D movements in the virtual software, and cephalometric landmarks can be marked and referenced. The central condylar hinge axis is virtually applied to the mandible and assists in accurate autorotation (see Fig. 2 B). The surgical movements are then planned via Internet meeting with the surgeons and biomedical engineer from the modeling company.
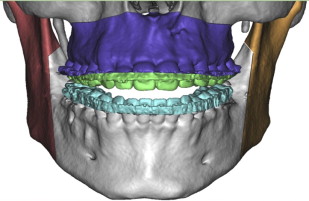
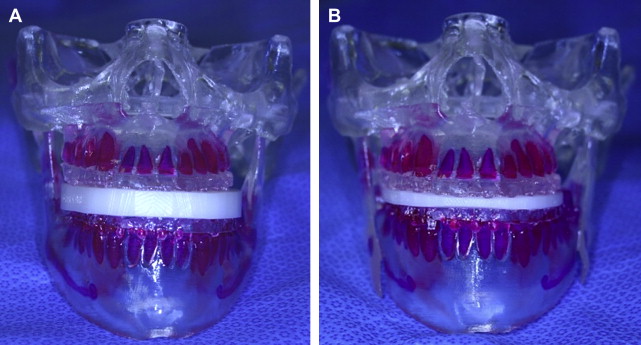
Lefort I and sagittal split osteotomies are performed virtually, and the correction of the midline discrepancies, vertical excess, and prognathism are completed. Correction of yaw, pitch, and roll are confirmed by numerical leveling of the 3 axes compared with the preoperative gyroscopic facebow measurements. The osteotomized bony segments are color coded ( Fig. 4 ), and can be moved in all 3 planes of the space with the computer mouse. Once the ideal virtual surgery is performed, the plan is submitted and the modeling phase can begin. The modeling company (Medical Modeling Inc, Golden, CO) fabricates stereolithographic models of the skull as well as intermediate ( Fig. 5 A) and final (see Fig. 5 B) occlusal splints.