Disorders of the Mouth 
Diseases of the Lips ICD-9: 528.5 ° ICD-10: K13.0

Figure 33-1. Angular cheilitis Mild erythema and scaling in bilateral commissures. (Courtesy of Dr. Nathaniel Treister.)
Conditions of the Tongue, Palate, and Mandible ICD-9: 528.6, 528.7, 529 ° ICD-10: K14
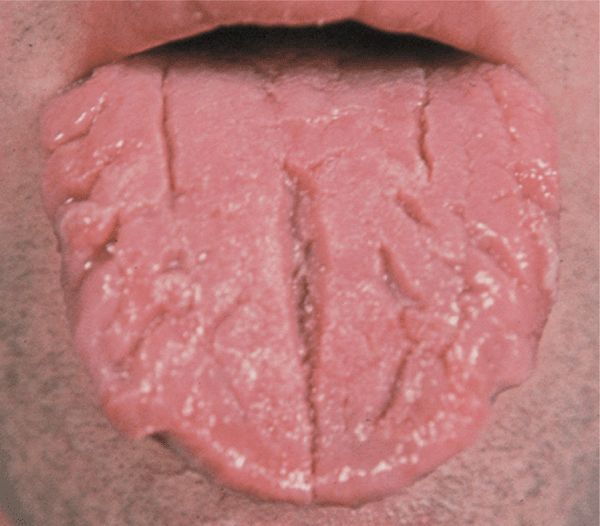
Figure 33-2. Fissured tongue Deep furrows on the dorsum of the tongue are asymptomatic.
Figure 33-3. Hairy tongue Defective desquamation of filiform papilla noted in posterior aspect of tongue. Tongue has a white surface due to retained keratin. (Courtesy of Dr. Nathaniel Treister.)

Figure 33-4. Migratory glossitis Areas of hyperkeratosis alternate with areas of normal pink epithelium, creating a geographic pattern in a female with psoriasis.
Diseases of the Gingiva, Periodontium, and Mucous Membranes ICD-9: 523  ICD-10: K06
ICD-10: K06
Erosive Gingivostomatitis
Reaction pattern associated with viral infection, autoimmunity, lichen planus (LP), erythema multiforme, pemphigus, cicatricial pemphigoid. Findings: Erythema, desquamation, and edema of gingivae. Other mucocutaneous sites may be affected.
Lichenoid Mucositis
Findings: Reticulated white plaques and painful erosions on mucosal surfaces.
Etiology: LP, drugs (NSAIDs, antihypertensive agents), allergic contact dermatitis, graft-versus-host disease.
Figure 33-5. (A) Torus palatinus Bony protrusion in the midline, upper palate. (B) Mandibular torus Unilateral protrusion near premolars, above the mylohyoid muscle insertion into the mandible. (Courtesy of Dr. Nathaniel Treister.)

Figure 33-6. Lichen planus: Wickham striae Poorly defined violaceous plaque with lacy, white pattern on the buccal mucosa.

Figure 33-7. Lichen planus: desquamative gingivitis The gingival margins are erythematous, edematous, and retracted. The lesions were painful, making dental hygiene difficult, resulting in plaque formation on the teeth.
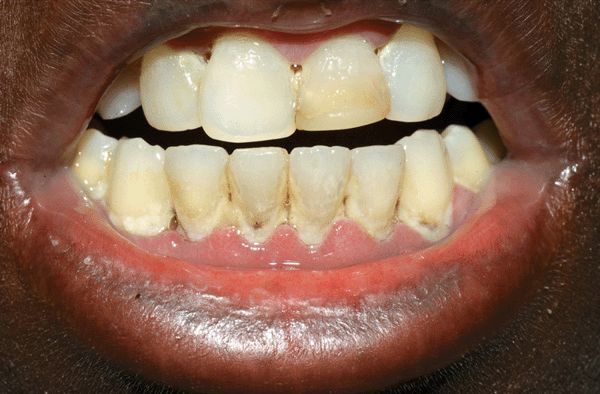
Figure 33-8. Acute necrotizing ulcerative gingivitis (ANUG) Very painful gingivitis with necrosis on marginal gingiva, edema, purulence, and halitosis in a 35-year-old female with advanced HIV disease. ANUG resolved with oral clindamycin.
 Oral mucosa covers and protects tissues beneath it and conveys sensory information from the surface.
Oral mucosa covers and protects tissues beneath it and conveys sensory information from the surface. Normal function is required for mastication, deglutition, chemosensory function, and phonation.
Normal function is required for mastication, deglutition, chemosensory function, and phonation. Impaired oral mucosal health causes pain, malnutrition, infection, compromised immune function, and exacerbations of medical disorders.
Impaired oral mucosal health causes pain, malnutrition, infection, compromised immune function, and exacerbations of medical disorders.
 Associated with increased moisture at commissures, salivation (at sleep).
Associated with increased moisture at commissures, salivation (at sleep). Predisposing factors: thumb sucking in children; sagging face and loss of teeth in older persons; candidiasis in immunocompromised persons; Staphylococcus aureus in atopic dermatitis and isotretinoin treatment.
Predisposing factors: thumb sucking in children; sagging face and loss of teeth in older persons; candidiasis in immunocompromised persons; Staphylococcus aureus in atopic dermatitis and isotretinoin treatment. Findings: erythema and maceration at commissures (see
Findings: erythema and maceration at commissures (see  Diagnosis: KOH for candidiasis; culture for S. aureus, Candida.
Diagnosis: KOH for candidiasis; culture for S. aureus, Candida. Management: Identify and treat causes.
Management: Identify and treat causes.

 Normal variant in up to 11% of population. Asymptomatic.
Normal variant in up to 11% of population. Asymptomatic. Findings: Multiple folds with anterior-posterior orientation on the dorsal surface of the tongue (
Findings: Multiple folds with anterior-posterior orientation on the dorsal surface of the tongue ( Associated disorders: Psoriasis, Down syndrome, acromegaly, Sjögren syndrome.
Associated disorders: Psoriasis, Down syndrome, acromegaly, Sjögren syndrome. Synonyms: Lingua fissurata, lingua plicata, scrotal tongue, grooved tongue, furrowed tongue.
Synonyms: Lingua fissurata, lingua plicata, scrotal tongue, grooved tongue, furrowed tongue.

 Pathogenesis: Defective desquamation of filiform papillae resulting in hair-like projections on the dorsum of the tongue.
Pathogenesis: Defective desquamation of filiform papillae resulting in hair-like projections on the dorsum of the tongue. Associations: Heavy tobacco use, mouth breathing, systemic antibiotic therapy, poor oral hygiene, general debilitation, radiation therapy, chronic use of bismuth-containing antacids, lack of dietary roughage.
Associations: Heavy tobacco use, mouth breathing, systemic antibiotic therapy, poor oral hygiene, general debilitation, radiation therapy, chronic use of bismuth-containing antacids, lack of dietary roughage. Symptoms: Gagging sensation, altered taste, halitosis, cosmetic disfigurement.
Symptoms: Gagging sensation, altered taste, halitosis, cosmetic disfigurement. Findings: Furry plaques on dorsal tongue (
Findings: Furry plaques on dorsal tongue ( Management: Eliminate predisposing factors; good oral hygiene.
Management: Eliminate predisposing factors; good oral hygiene. Synonym: Lingua villosa (nigra).
Synonym: Lingua villosa (nigra).
 Pathogenesis: Epstein–Barr virus infection; low CD4 cell counts.
Pathogenesis: Epstein–Barr virus infection; low CD4 cell counts. Findings: White corrugated plaques on lateral aspects of tongue (see Fig. 27-66). Does not occur in successfully treated HIV/AIDS.
Findings: White corrugated plaques on lateral aspects of tongue (see Fig. 27-66). Does not occur in successfully treated HIV/AIDS.
 Irregular areas of dekeratinized and desquamated filiform papillae (red in color) are surrounded by elevated whitish or yellow margins (
Irregular areas of dekeratinized and desquamated filiform papillae (red in color) are surrounded by elevated whitish or yellow margins ( Etiology: unknown; possible link with psoriasis. Incidence: common; usually asymptomatic.
Etiology: unknown; possible link with psoriasis. Incidence: common; usually asymptomatic. Synonym: Geographic tongue.
Synonym: Geographic tongue. Pathogenesis: genetic predisposition, ? autosomal dominant in some series, more common in females, Native Americans, Eskimos (torus palatini); local stressors (mandibular and palatal tori), bony protrusions
Pathogenesis: genetic predisposition, ? autosomal dominant in some series, more common in females, Native Americans, Eskimos (torus palatini); local stressors (mandibular and palatal tori), bony protrusions Associations: bruxism
Associations: bruxism Symptoms: may be complicated by ulceration; usually asymptomatic
Symptoms: may be complicated by ulceration; usually asymptomatic Findings: palatal tori are usually in midline of palate and less than 2 cm, but can vary in size through life; mandibular tori found usually near premolars; rarely bilateral. They are smooth, nodular protrusions (
Findings: palatal tori are usually in midline of palate and less than 2 cm, but can vary in size through life; mandibular tori found usually near premolars; rarely bilateral. They are smooth, nodular protrusions ( Management: not needed; if create ulcerations or complicate dental prosthesis, surgery can be done. Have been used as autogenous bone grafts.
Management: not needed; if create ulcerations or complicate dental prosthesis, surgery can be done. Have been used as autogenous bone grafts.
 Gingivitis: Erythema, edema, blunting of interdental papillae without bone loss. Predisposing factors: poor oral hygiene, tobacco use, diabetes.
Gingivitis: Erythema, edema, blunting of interdental papillae without bone loss. Predisposing factors: poor oral hygiene, tobacco use, diabetes. Periodontitis: Chronic infection of connective tissue, periodontal ligament, and alveolar bone; most common cause of tooth loss in adults.
Periodontitis: Chronic infection of connective tissue, periodontal ligament, and alveolar bone; most common cause of tooth loss in adults. Course: Accumulation of subgingival calculus (calcified plaque) and Actinobacillus actinomycetemcomitans infection results in painless soft tissue edema, insidious alveolar bone resorption, deepening periodontal pockets, and tooth loss.
Course: Accumulation of subgingival calculus (calcified plaque) and Actinobacillus actinomycetemcomitans infection results in painless soft tissue edema, insidious alveolar bone resorption, deepening periodontal pockets, and tooth loss.
 Incidence: 40-60% of individuals with LP have oropharyngeal involvement.
Incidence: 40-60% of individuals with LP have oropharyngeal involvement. Findings:
Findings: Milky-white papules.
Milky-white papules. Wickham striae: Reticulate (netlike) patterns of lacy-white hyperkeratosis [buccal mucosa (
Wickham striae: Reticulate (netlike) patterns of lacy-white hyperkeratosis [buccal mucosa ( Hypertrophic LP—leukoplakia with Wickham striae usually on the buccal mucosa.
Hypertrophic LP—leukoplakia with Wickham striae usually on the buccal mucosa. Atrophic LP—shiny plaque often with Wickham striae in surrounding mucosa.
Atrophic LP—shiny plaque often with Wickham striae in surrounding mucosa. Erosive/ulcerative LP—superficial erosions with overlying fibrin clots that are seen on the tongue and buccal mucosa; can be painful (
Erosive/ulcerative LP—superficial erosions with overlying fibrin clots that are seen on the tongue and buccal mucosa; can be painful ( Bullous LP—intact blisters (rupture and result in erosive LP).
Bullous LP—intact blisters (rupture and result in erosive LP). Desquamative gingivitis—bright red gingiva (
Desquamative gingivitis—bright red gingiva (
 Precipitating factors: Poor oral hygiene, HIV/AIDS, immunosuppression, alcohol and tobacco use, nutritional deficiency.
Precipitating factors: Poor oral hygiene, HIV/AIDS, immunosuppression, alcohol and tobacco use, nutritional deficiency. Findings (
Findings ( Etiologic agents: Bacteroides fusiformis, Prevotella intermedia, Borrelia vincentii, Treponema.
Etiologic agents: Bacteroides fusiformis, Prevotella intermedia, Borrelia vincentii, Treponema. Management: Systemic antibiotics such as clindamycin, metronidazole, amoxicillin. Dental hygiene.
Management: Systemic antibiotics such as clindamycin, metronidazole, amoxicillin. Dental hygiene. Synonyms: Trench mouth, Vincent disease.
Synonyms: Trench mouth, Vincent disease.
 Findings: Hypertrophy of both the free and attached gingivae, particularly the interdental papillae (
Findings: Hypertrophy of both the free and attached gingivae, particularly the interdental papillae ( Inflammatory enlargement: Most common cause of gingival enlargement. Caused by edema and infective cellular infiltration caused by prolonged exposure to bacterial plaque; fibrosis occurs if untreated.
Inflammatory enlargement: Most common cause of gingival enlargement. Caused by edema and infective cellular infiltration caused by prolonged exposure to bacterial plaque; fibrosis occurs if untreated. Drug-induced fibrous hyperplasia of gingivae: May cover the teeth and is associated with:
Drug-induced fibrous hyperplasia of gingivae: May cover the teeth and is associated with: Anticonvulsants: phenytoin, succinimides, valproic acid.
Anticonvulsants: phenytoin, succinimides, valproic acid. Calcium channel blockers: nifedipine, verapamil.
Calcium channel blockers: nifedipine, verapamil. Cyclosporine.
Cyclosporine. Systemic conditions/disorders:
Systemic conditions/disorders: Pregnancy, puberty, vitamin C deficiency, glycogen storage disease.
Pregnancy, puberty, vitamin C deficiency, glycogen storage disease. Chronic myelomonocytic leukemia (
Chronic myelomonocytic leukemia (








