Fungal Infections of the Skin, Hair, and Nails 
Clinical Manifestation
Mucosal Candidiasis. Otherwise healthy individuals: oropharynx and genitalia. Host defense defects: in the esophagus and tracheobronchial tree.
Cutaneous Candidiasis. Intertriginous and occluded skin.
Disseminated Candidemia. Host defense defects, especially neutropenia. Usually after invasion of the gastrointestinal (GI) tract.
Epidemiology and Etiology
Etiology. C. albicans, C. tropicalis, C. parapsilosis, C. guilliermondii, C. krusei, C. pseudotropicalis, C. lusitaniae, C. glabrata.
Ecology. Candida spp. frequently colonize the GI tract and can be transmitted via the birth canal. Approximately 20% of healthy individals are colonized. Antibiotic therapy increases the incidence of colonization.
Ten percent of women are colonized vaginally; antibiotic therapy, pregnancy, oral contraception, and intrauterine devices increase incidence. C. albicans may transiently be present on the skin and infection is usually endogenous. Candida balanitis may be transmitted from sexual partner. The young and old are more likely to be colonized.
Host Factors. Host defense defects, diabetes mellitus, obesity; hyperhidrosis, warm climate, maceration; polyendocrinopathies; glucocorticoids; chronic debilitation.
Laboratory Examinations
Direct Microscopy. KOH preparation visualizes pseudohyphae and yeast forms (Fig. 26-1).
Figure 26-1. Candida albicans: KOH preparation Budding yeast forms and sausage-like pseudohyphal forms.
Culture. Identifies species of Candida; however, the presence in culture of C. albicans does not make the diagnosis of candidiasis. Sensitivities to antifungal agents can be performed on isolate in cases of recurrent infection. Rule out bacterial secondary infection.
Clinical Manifestation
Candidai Intertrigo. Pruritus, tenderness, pain. Initial pustules on erythematous base become eroded and confluent. Subsequently, fairly sharply demarcated, polycyclic, erythematous, eroded patches with small pustular lesions at the periphery (satellite pustulosis). Distribution: Inframammary or submammary Fig. 26-2, axillae, groins (Fig. 26-3, perineal, and intergluteal cleft.

Figure 26-2. Cutaneous candidiasis: intertrigo Small peripheral “satellite” papules and pustules that have become confluent centrally, creating a large eroded area in the submammary region.

Figure 26-3. Cutaneous candidiasis: intertrigo Erythematous papules with a few pustules, becoming confluent in the inguinal area and medial thigh. The lesions occurred during a holiday trip to the Caribbean.
Interdigital. Most common in obese elderly. Initial pustule becomes eroded, with formation of superficial erosion or fissure (Fig. 26-4). May be associated with Candida paronychia. Distribution: webspace usually between third and fourth fingers (Fig. 26-4); feet: maceration in webspace.

Figure 26-4. Cutaneous candidiasis: interdigital intertrigo An 80-year-old male with painful site in the webspace of the hand. Erosion with erythema is seen in the webspace between two fingers.
Diaper Dermatitis. Irritability, discomfort with urination, defecation, changing diapers. Erythema, edema with papular, and pustular lesions; erosions, collarette-like scaling at the margins of lesions. Distribution: genital and perianal skin, inner aspects of thighs and buttocks (Fig. 26-5).

Figure 26-5. Candidiasis: diaper dermatitis Confluent erosions, marginal scaling, and “satellite pustules” in the area covered by a diaper in an infant. Atopic dermatitis or psoriasis also occurs in this distribution and may be concurrent.
Occluded Skin. Under occlusive dressing, under cast, on back in hospitalized patient.
Follicular Candidiasis. Small, discrete pustules in ostia of hair follicles. Usually in occluded skin.
Differential Diagnosis
Intertrigo/Occluded Skin. Intertriginous psoriasis, erythrasma, dermatophytosis, pityriasis versicolor, streptococcal intertrigo,
Diaper Dermatitis. Atopic dermatitis, psoriasis, irritant dermatitis, seborrheic dermatitis.
Folliculitis. Bacterial (Staphylococcus aureus, Pseudomonas aeruginosa) folliculitis, Pityrosporum folliculitis, acne.
Diagnosis
Clinical findings confirmed by direct microscopy or culture.
Treatment
Prevention. Keep intertriginous areas dry, wash with benzoyl peroxide bar and use imidazole powder.
Topical Antifungals. Nystatin, azole, or imidazole cream.
Oral Antifungals. Nystatin (suspension, tablet, pastille.) Eradicates bowel colonization. May be effective in recurrent candidiasis of diaper area, genitals, or intertrigo.
Systemic Antifungal Agents. Fluconazole tablets (50, 100, 150, 200 mg), oral suspension (50 mg/ml); parenteral for IV infusion. Itroconazole capsules (100 mg), oral solution 10 mg/ml), ketoconazole tablets (200 mg), amphotericin B IV for severe disease.
Epidemiology
Incidence. Often mucosal candidiasis occurs in otherwise healthy individuals. In advanced HIV disease: oropharyngeal candidiasis is common, relapses after treatment, and may be associated with esophageal and tracheobronchial candidiasis.
Classification of Mucosal Candidiasis
Oropharyngeal Candidiasis
• Pseudomembranous candidiasis or thrush
• Erythematous or atrophic candidiasis
• Candidal leukoplakia or hyperplastic candidiasis
• Angular cheilitis
Esophageal and Tracheobronchial Candidiasis. Occurs in states of severe host defense defects. AIDS-defining conditions.
Clinical Manifestation
Oropharyngeal Candidiasis. Often asymptomatic. Burning or pain on eating spices/acidic foods, diminished taste sensation. Cosmetic concern about white curds on tongue. Odynophagia. In HIV disease, may be the initial presentation.
• Pseudomembranous Candidiasis. See Figs. 26-6 through 26-8. White cottage cheese-like flecks (colonies of Candida) on any mucosal surface; vary in size from 1–2 mm to extensive and widespread. Removal with a dry gauze pad leaves an erythematous mucosal surface. Distribution: Dorsum of tongue, buccal mucosa, hard/soft palate, pharynx extending down into esophagus and tracheobronchial tree.

Figure 26-6. Oral candidiasis: thrush White curd-like material on the mucosal surface of the lower lip of a child; the material can be abraded with gauze (pseudomembranous), revealing underlying erythema.

Figure 26-7. Oral candidiasis: thrush Extensive cottage cheese-like plaques, colonies of Candida that can be removed by rubbing with gauze (pseudomembranous), on the palate and uvula of an individual with advanced HIV/AIDS. Patches of erythema between the white plaques represent erythematous (atrophic) candidiasis. Involvement may extend into the esophagus and become associated with dysphagia.
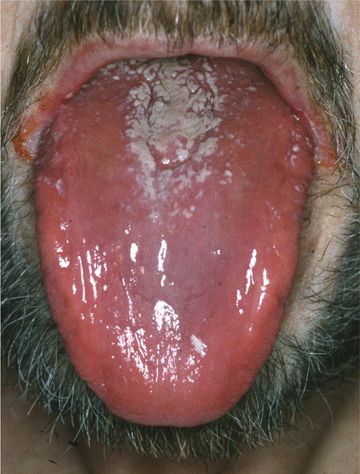
Figure 26-8. Oral candidiasis: atrophic and pseudomembranous A 48-year-old male with HIV disease. The surface of the tongue is shiny and red; posterior tongue has a white coating (thrush).
• Erythematous or Atrophic Candidiasis. Dorsum of tongue is smooth, red, atrophic (Fig. 26-8). Areas of thrush may also be present.
• Candidal Leukoplakia. White plaques that cannot be wiped off but regress with anticandidal therapy. Distribution: buccal mucosa, tongue, hard palate.
• Angular Cheilitis. Intertrigo at the angles of lips (Fig. 26-9). Erythema; slight erosion. White colonies of Candida in some cases. Usually associated with oropharyngeal colonization with Candida.

Figure 26-9. Angular cheilitis A 55-year-old male. The angle of the lips is moist and red. KOH preparation revealed candida pseudohyphae. Oral candidiasis was also present.
Esophageal and Tracheobronchial Candidiasis. Occurs in HIV disease when CD4+ cell count is low and is an AIDS-defining condition. Odynophagia, resulting in difficulty eating and malnutrition. Pseudomembranous lesions are seen on endoscopy.
Invasive Disseminated Candidiasis. In individuals with severe prolonged neutropenia. Portal of entry of Candida: GI tract, invading submucosa, and blood vessels; intravascular catheter. Candidemia: hematogenous dissemination to skin and viscera. Disseminated red papules (Fig. 26-14)
Differential Diagnosis
Pseudomembranous Candidiasis. Oral hairy leukoplakia, condyloma acuminatum, geographic tongue, hairy tongue, lichen planus, bite irritation.
Atrophic Candidiasis. Lichen planus, poor nutrition, vitamin deficiency
Diagnosis
Clinical suspicion confirmed by KOH preparation of scraping from mucosal surface. Endoscopy to document esophageal and/or tracheobronchial candidiasis.
Course
Most cases respond to correction of the precipitating cause such as use of inhaled glucocorticoids. Topical agents effective in most cases. Clinical resistance to antifungal agents may be related to patient noncompliance, severe immunocompromised, drug–drug interaction (rifampin–fluconazole).
Treatment
Topical Therapy. Nystatin or clotrimazole.
Systemic Therapy. Oral fluconazole, itraconazole, ketoconazole. Amphotericin B for severe resistant disease.
Epidemiology
More than 20% of women have vaginal colonization by Candida. C. albicans accounts for 80–90% of genital isolates.
Incidence. Most vaginal candidiasis occurs in the healthy population. Seventy-five percent of women experience at least one episode; 40–45% experience two or more episodes. Often associated with vulvar candidiasis, i.e., vulvovaginal candidiasis.
Risk Factors. Diabetes mellitus, HIV disease. Females: Often none; pregnancy. Males; uncircumcised.
Clinical Manifestation
Vulvitis/Vulvovaginitis. Onset often abrupt, usually the week before menstruation. Symptoms may recur before each menstruation. Pruritus, vaginal discharge, vaginal soreness, vulvar burning, dyspareunia, and external dysuria.
Vulvitis. Erosions, edema, erythema (Fig. 26-10), swelling, removable curd-like material. Pustule on lateral vulva and adjacent skin

Figure 26-10. Candidiasis: vulvitis and intertrigo Psoriasiform, erythematous lesions becoming confluent on the vulva with erosions and satellite pustules on the thighs.
Vulvovaginitis. Vaginal erythema and edema; white plaques that can be wiped off vaginal and/or cervical mucosa. May be associated with candidal intertrigo of inguinal folds and perineum. Subcorneal pustules at periphery with fringed, irregular margins. In chronic cases, vaginal mucosa glazed and atrophic.
Balanoposthitis, balanitis glans, and preputial sac: papules, pustules, erosions (Fig. 26-11). Maculopapular lesions with diffuse erythema. Edema, ulcerations, and fissuring of prepuce, usually in diabetic men; white plaques under foreskin.

Figure 26-11. Candidiasis: balanoposthitis A 52-year-old uncircumcised male. Erythema and a curd-like matter is seen on the glans penis and foreskin.
Differential Diagnosis
Vulvovaginal Candidiasis. Trichomoniasis (caused by T. vaginalis), bacterial vaginosis (caused by replacement of normal vaginal flora by an overgrowth of anaerobic microorganisms and Gardnerella vaginalis), lichen planus, lichen sclerosus et atrophicus.
Balanoposthitis. Psoriasis, eczema, lichen planus
Diagnosis
Clinical suspicion confirmed by KOH preparation of scraping from mucosal surface.
Treatment
Azole Creams or Suppository. Treat sexual partners and consider systemic therapy (as for mucocutaneous candidiasis p. 596) if recurrent.
Clinical Manifestation
Oropharyngeal Candidiasis. Refractory to conventional therapy. Relapsing after successful therapy. Chronic infection results in hypertrophic (leukoplakic) candidiasis.
Cutaneous candidiasis manifests as: Intertrigo. Widespread infection (Figs. 26-12 and 26-13) of the face, trunk, and/or extremities, Lesions become hypertrophic in chronic untreated cases. Infection of the nail apparatus is universal: Chronic paronychia; nail plate infection and dystrophy; eventually total nail dystrophy.

Figure 26-12. Mucocutaneous candidiasis Persistent candidiasis in an immunocompromised infant manifesting as erosions covered by scales and crusts, oropharyngeal candidiasis, and widespread infection of the trunk.

Figure 26-13. Mucocutaneous candidiasis A 3-year-old child with hypothyroidism had thrush, intertriginous candidiasis, warty hyperkeratoses, and crusts on the scalp and face; and also, candidal onychomycosis.
Many patients also have dermatophytosis and cutaneous warts.
Six Types of Chronic Mucocutaneous Candidiasis
• Chronic oral candidiasis
• Chronic candidiasis with endocrinopathy
• Chronic candidiasis without endocrinopathy
• Chronic localized mucocutaneous candidiasis
• Chronic diffuse candidiasis
• Chronic candidiasis with thymoma.
Clinical Manifestation
Cutaneous Lesions. Small disseminated erythematous cutaneous papules (Fig. 26-14). Lesions may occur acutely or chronically.

Figure 26-14. Invasive candidiasis with candidemia Multiple, erythematous papules on the hand of a febrile patient with granulocytopenia associated with treatment of acute myelogenous leukemia. The usual source of the infection is the gastrointestinal tract. C. tropicalis was isolated on blood culture; candidal forms were seen on lesional skin biopsy.
Systemic Dissemination. Eye with retinal changes. Liver, spleen, CNS
Differential Diagnosis
Malassezia folliculitis, which occurs on the trunk of healthy individuals.
Diagnosis
Lesional biopsy specimen: Candida yeast forms are visualized in the dermis; Candida species isolated on culture.
Course
Candidemia has high associated morbidity and mortality.
Treatment
Fluconazole in nonneutropenic patients; triazoles echinocandins, caspofungin, micafungin, anidulafungin, voriconazole and posaconazole, as well as lipid formulations of amphotericin B.
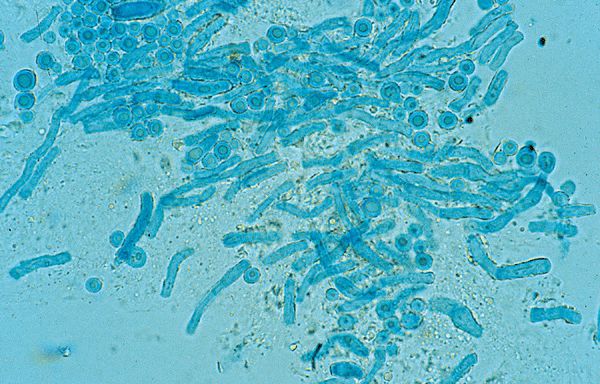
Figure 26-15. Malassezia furfur: KOH preparation Round yeast and elongated pseudohyphal forms, so-called “spaghetti and meatballs.”
Clinical Manifestation
Usually asymptomatic. Cosmetic concerns about dyspigmentation. Lesions present for months or years.
Macules, sharply marginated (Figs. 26-16 to 26-19) round or oval in shape, varying in size. Fine scaling is best appreciated by gently abrading lesions. Treated or resolved lesions lack scale. Some patients have findings of Malassezia folliculitis and seborrheic dermatitis.

Figure 26-16. Pityriasis versicolor A 43-year-old white female with orange-tan lesions of the lateral neck. Sharply marginated scaling macules.

Figure 26-17. Pityriasis versicolor: neck A 23-year-old obese black female with discoloration of the neck for 1 year. Sharply marginated brown scaling macules on the left side of the neck. The velvety texture and hyperpigmentation of the skin of the neck is acanthosis nigricans associated with obesity.

Figure 26-18. Pityriasis versicolor: chest and arm A 36-year-old male with pigmented patches on chest and arms for several years. Multiple pink, well-demarcated scaling macules becoming confluent on the neck, chest, flank, and arm.
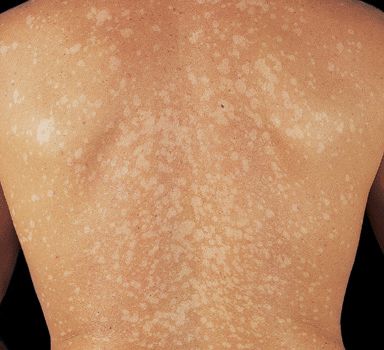
Figure 26-19. Pityriasis versicolor: back Multiple, small-to-medium-sized, well-demarcated hypopigmented macules on the back of a tanned individual with white skin.
Color. In nontanned skin, lesions are light brown (Fig. 26-18) or pink. On tanned skin, hypopigmented (Fig. 26-19). In brown- or black-skinned persons, dark brown macules (Figs. 26-17 and 26-20). Brown of varying intensities and hues (Fig. 26-18). In time, individual lesions may enlarge and merge, forming extensive geographic areas.
Figure 26-20. Pityriasis versicolor: face A 18-year-old black female hypopigmented scaling macule on chin. She had been applying cocoa butter to face since childhood.
Distribution. Upper trunk, upper arms, neck, abdomen, axillae, groins, thighs, genitalia. Facial, neck, or scalp lesions occur in persons applying creams or ointments or topical glucocorticoid preparations.
Differential Diagnosis
Hypopigmented Macules. Vitiligo, pityriasis alba, postinflammatory hypopigmentation.
Scaling Lesions. Tinea corporis, seborrheic dermatitis, cutaneous T cell lymphoma.
Laboratory Examinations
Direct Microscopic Examination of Scales Prepared with KOH. Filamentous hyphae and globose yeast forms, termed spaghetti and meatballs are seen (Fig. 26-15).
Wood’s Lamp. Blue-green fluorescence of scales; may be negative in individuals who have showered recently because the fluorescent chemical is water soluble. Vitiligo appears as depigmented, white, and has no scale.
Dermatopathology. Budding yeast and hyphal forms in the most superficial layers of the stratum corneum, seen best with periodic acid–Schiff (PAS) stain. Variable hyperkeratosis, psoriasiform hyperplasia, chronic inflammation with blood vessel dilatation.
Diagnosis
Clinical findings confirmed by positive KOH preparation findings.
Course
Infection persists for years if predisposing conditions persist. Dyspigmentation persists for months after infection has been eradicated.
Treatment
Topitcal agents. Selenium sulfide (2.5%) lotion or shampoo. Ketoconazole shampoo. Azole creams (ketoconazole, econazole, micronazole, clotrimazole). Terbinafine 1% solution.
Systemic therapy Ketoconazole 400 mg stat, 1 hour before exercise. Fluconazole 400 mg stat. Itraconazole 400 mg stat (drugs not approved for use in TV in the United States).
Secondary prophylaxis. Topical agents weekly or systemic agents monthly.
Malassezia Folliculitis. See “Infectious Folliculitis” Section 31.
Seborrheic Dermatitis. See “Seborrheic Dermatitis” Section 2.
 Superficial Fungal Infections. Caused by fungi that are capable of colonizing (cutaneous microbiome) and superficially invading skin and mucosal sites:
Superficial Fungal Infections. Caused by fungi that are capable of colonizing (cutaneous microbiome) and superficially invading skin and mucosal sites: Candida species
Candida species Malassezia species
Malassezia species Dermatophytes.
Dermatophytes. Deeper, Chronic Cutaneous Fungal Infections. Occur after percutaneous inoculation:
Deeper, Chronic Cutaneous Fungal Infections. Occur after percutaneous inoculation: Phaeohyphomycosis (eumycetoma, chromoblastomycosis)
Phaeohyphomycosis (eumycetoma, chromoblastomycosis) Sporotrichosis
Sporotrichosis Systemic Fungal Infections with Cutaneous Dissemination. Occur most often with host defense defects. Primary lung infection disseminates hematogenously to multiple organ systems, including the skin: Cryptococcosis, histoplasmosis, North American blastomycosis, coccidioidomycosis, and penicillinosis.
Systemic Fungal Infections with Cutaneous Dissemination. Occur most often with host defense defects. Primary lung infection disseminates hematogenously to multiple organ systems, including the skin: Cryptococcosis, histoplasmosis, North American blastomycosis, coccidioidomycosis, and penicillinosis. ICD-10: B36
ICD-10: B36 Superficial fungal infections are the most common of all mucocutaneous infections, often caused by overgrowth of mucocutaneous microbiome.
Superficial fungal infections are the most common of all mucocutaneous infections, often caused by overgrowth of mucocutaneous microbiome. Candida Species. Require a warm humid microenvironment.
Candida Species. Require a warm humid microenvironment. Malassezia Species. Require a humid microenvironment and lipids for growth.
Malassezia Species. Require a humid microenvironment and lipids for growth. Dermatophytes. Infect keratinized epithelium, hair follicles, and nail apparatus Trichosporon species Hortaea (Exophiala or Phaeoannellomyces) werneckii: Tinea nigra
Dermatophytes. Infect keratinized epithelium, hair follicles, and nail apparatus Trichosporon species Hortaea (Exophiala or Phaeoannellomyces) werneckii: Tinea nigra ICD-10: B37.0
ICD-10: B37.0 Etiology. Most commonly caused by the yeast Candida albicans. Less often by other Candida species.
Etiology. Most commonly caused by the yeast Candida albicans. Less often by other Candida species.
 Cutaneous candidiasis occurs in moist, occluded sites.
Cutaneous candidiasis occurs in moist, occluded sites. Many patients have predisposing factors.
Many patients have predisposing factors. ICO-10: B38.0
ICO-10: B38.0 
 Occurs with minor variations in host factors. Antibiotic therapy; glucocorticoid therapy (topical or systemic); age (very young, very old); host defense defects.
Occurs with minor variations in host factors. Antibiotic therapy; glucocorticoid therapy (topical or systemic); age (very young, very old); host defense defects. ICD-10: B37.3/B37.4
ICD-10: B37.3/B37.4 
 Occurs on the nonkeratinized genital mucosa
Occurs on the nonkeratinized genital mucosa Vulva, vagina
Vulva, vagina Preputial sac of the penis
Preputial sac of the penis Usually represents overgrowth of Candida in mucocutaneous microbiome.
Usually represents overgrowth of Candida in mucocutaneous microbiome. ICD-10: B37.7
ICD-10: B37.7 
 Characterized by persistent or recurrent Candida infections of the oropharynx, skin, and nail apparatus.
Characterized by persistent or recurrent Candida infections of the oropharynx, skin, and nail apparatus. Inheritance. Usually autosomal recessive or sporadic.
Inheritance. Usually autosomal recessive or sporadic. Host Defense Defect. Various specific and global defects in cell-mediated immunity.
Host Defense Defect. Various specific and global defects in cell-mediated immunity. Onset. Usually in infancy or early childhood.
Onset. Usually in infancy or early childhood. ICD-10: B37
ICD-10: B37 
 Etiology. C. albicans, C. tropicalis, and other non-albicans species.
Etiology. C. albicans, C. tropicalis, and other non-albicans species. Incidence. Fifth most common cause of nosocomial bloodstream infections in the United States.
Incidence. Fifth most common cause of nosocomial bloodstream infections in the United States. Risk Factors. Neutropenia. Venous access catheters. Hospitalization.
Risk Factors. Neutropenia. Venous access catheters. Hospitalization. Pathogenesis. Candida enters the blood stream having colonized venous access catheters or penetrated the intestinal mucosa. Candidemia seeds the skin and internal organs, i.e., hepatosplenic candidiasis.
Pathogenesis. Candida enters the blood stream having colonized venous access catheters or penetrated the intestinal mucosa. Candidemia seeds the skin and internal organs, i.e., hepatosplenic candidiasis. ICD-10: B36.0
ICD-10: B36.0 
 Etiology. Associated with the superficial overgrowth of the mycelial form of Malassezia furfur. Lipophilic yeast that normally resides in the keratin of skin (
Etiology. Associated with the superficial overgrowth of the mycelial form of Malassezia furfur. Lipophilic yeast that normally resides in the keratin of skin ( Clinical Findings. Chronic. Well-demarcated scaling patches. Variable pigmentation: hypo- and hyperpigmented; pink. Most commonly on the trunk.
Clinical Findings. Chronic. Well-demarcated scaling patches. Variable pigmentation: hypo- and hyperpigmented; pink. Most commonly on the trunk. Demography. Young adults. Less common when sebum production is reduced or absent; tapers off during fifth and sixth decades.
Demography. Young adults. Less common when sebum production is reduced or absent; tapers off during fifth and sixth decades. Predisposing Factors. Sweating. Warm season or climates; tropical climate. Hyperhidrosis; aerobic exercise. Oily skin. Temperate zones: more common in summertime; 2% prevalence in temperate climates; 20% in tropics. Application of lipids such as cocoa butter predisposes young children.
Predisposing Factors. Sweating. Warm season or climates; tropical climate. Hyperhidrosis; aerobic exercise. Oily skin. Temperate zones: more common in summertime; 2% prevalence in temperate climates; 20% in tropics. Application of lipids such as cocoa butter predisposes young children. Pathogenesis. Malassezia changes from blastospore form to mycelial form under the influence of predisposing factors. Dicarboxylic acid formed by enzymatic oxidation of fatty acids in skin surface lipids inhibits tyrosinase in epidermal melanocytes and lead to hypomelanosis; the enzyme is present in M. furfur.
Pathogenesis. Malassezia changes from blastospore form to mycelial form under the influence of predisposing factors. Dicarboxylic acid formed by enzymatic oxidation of fatty acids in skin surface lipids inhibits tyrosinase in epidermal melanocytes and lead to hypomelanosis; the enzyme is present in M. furfur.








