Cutaneous Manifestations of Hodgkin Lymphoma
Hodgkin lymphoma is a distinct malignant lymphoma characterized by the presence of neoplastic Reed–Sternberg cells in association with different patterns of reactive cells. In the World Health Organization (WHO) Classification of Tumours of Haematopoietic and Lymphoid Tissues it is subdivided into two distinct entities: classical Hodgkin lymphoma (about 95% of cases) and nodular lymphocyte predominant Hodgkin lymphoma (about 5% of cases) [1]. Classical Hodgkin lymphoma is further classified into four subtypes: nodular sclerosis, mixed cellularity, lymphocyte-rich, and lymphocyte-depleted [1]. The Epstein–Barr virus (EBV) is detected frequently in all four subtypes of classical Hodgkin lymphoma.
Skin manifestations of nodal Hodgkin lymphoma were not uncommon in the past [2–7]. Modern treatment modalities have resulted in a dramatic decrease in cutaneous involvement, although occasional cases are still reported [8–10]. The incidence is probably less than 1%, but exact figures are missing.
Besides specific involvement by neoplastic cells, as in all systemic lymphomas the skin may be the site of nonspecific cutaneous manifestations, including various dermatoses and so-called “pruritus sine materia,” among others. This last condition is a characteristic (albeit not pathognomonic) sign of the disease, and the diagnosis of Hodgkin lymphoma should always be considered when evaluating these patients.
Nodal Hodgkin lymphoma may be preceded by, concomitant with, or followed by other cutaneous lymphoproliferative disorders including mycosis fungoides, lymphomatoid papulosis, and anaplastic large cell lymphoma (see also Chapters 2 and 4) [11–15]. Cases of Hodgkin lymphoma associated with granulomatous slack skin have also been described [16, 17]. These last may represent examples of mycosis fungoides-associated granulomatous slack skin in patients with Hodgkin lymphoma rather than true specific cutaneous manifestations of the disease. Similarly, the patient reported as having “follicular mucinosis” in association with Hodgkin lymphoma [18] may have had co-existent mycosis fungoides-associated follicular mucinosis.
Cutaneous relapse of Hodgkin lymphoma in patients who were treated for nodal disease and who are otherwise in complete remission should be regarded as highly unlikely. I have seen several such putative cases, all of them representing examples of cutaneous anaplastic large cell lymphoma or of lymphomatoid papulosis. In publications on this subject it is often impossible to ascertain whether the skin lesions did indeed represent specific cutaneous manifestations of the Hodgkin lymphoma or not [19]. Treatment in these cases should be tailored to the cutaneous disease, as skin lesions in this particular setting are most likely unrelated to the nodal Hodgkin lymphoma and do not represent a sign of relapse.
The onset of cutaneous manifestations of Hodgkin lymphoma has been observed in an HIV-infected patient [20] and nodal Hodgkin lymphoma may arise in the setting of immune suppression (see Chapter 17).
Primary Cutaneous Hodgkin Lymphoma
Rare cases of Hodgkin lymphoma presenting primarily in the skin without concomitant nodal disease have been described, even in recent years [21–25]. In my opinion, the vast majority, if not all, of these cases represent examples of lymphomatoid papulosis or cutaneous anaplastic large cell lymphoma (see Teaching case 24.1). Even patients who developed extracutaneous Hodgkin lymphoma in the follow-up period may have had a cutaneous T-cell lymphoma rather than a true primary cutaneous Hodgkin lymphoma. Although it cannot be excluded that in exceptional cases Hodgkin lymphoma arises primary in the skin without concomitant extracutaneous disease, on a practical level such a diagnosis should not be accepted unless alternative explanations can be ruled out by compelling evidence.
Clinical Features
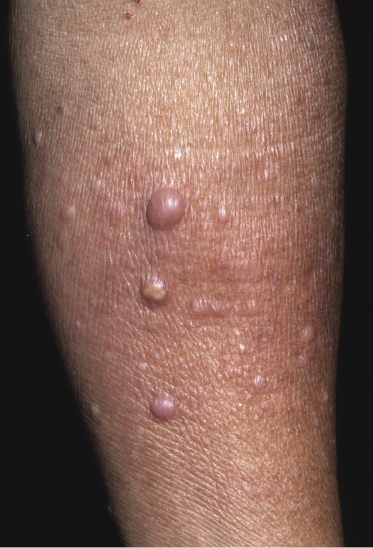
Clinically, skin lesions in Hodgkin lymphoma are usually confined to the drainage area of affected lymph nodes (retrograde lymphatic spread) [6, 26]. Papules, plaques, and tumors may all be observed (Figs 24.1 and 24.2) [26, 27]. Ulceration is not uncommon. In some cases lesions are generalized.

As already mentioned, the existence of a genuine primary cutaneous Hodgkin lymphoma is debatable, and cases published under this diagnosis most likely represent examples of lymphomatoid papulosis or cutaneous anaplastic large cell lymphoma.
Histopathology, Immunophenotype, and Molecular Genetics
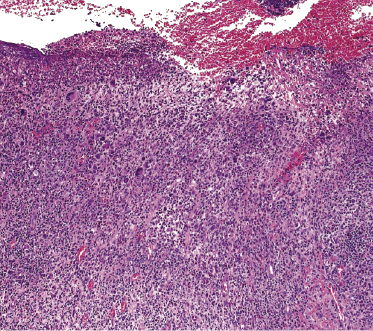
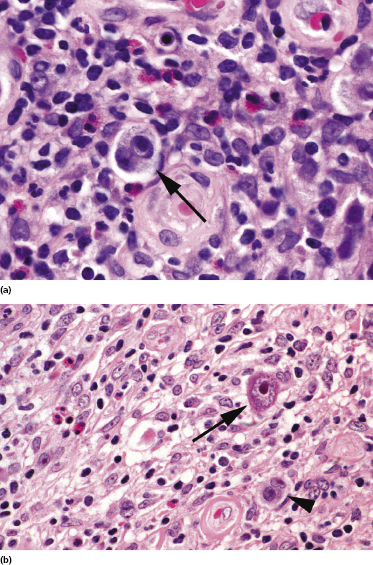
Histology shows the typical features of Hodgkin lymphoma with Reed–Sternberg and Hodgkin cells on a diffuse background of small lymphocytes, histiocytes, eosinophils, and plasma cells (Figs 24.3 and 24.4) [26]. Reed–Sternberg cells may be absent in some cutaneous lesions. It should be noted that Hodgkin and Reed–Sternberg-like cells may be found in a variety of other conditions including mainly lymphomatoid papulosis and cutaneous anaplastic large cell lymphoma, and thus cannot be considered specific for the diagnosis of cutaneous Hodgkin lymphoma.
In the lymph nodes, neoplastic cells in nodular lymphocyte-predominant Hodgkin lymphoma are positive for CD45, CD20, CD79a, and Bcl-6. CD30 and CD15 are usually negative in this subtype. A diagnosis of specific skin manifestations in this subtype of Hodgkin lymphoma may be very subjective and can only be made upon knowledge of nodal disease.
In classical Hodgkin lymphoma, which represent about 95% of all cases, Reed–Sternberg and Hodgkin cells are always positive for CD30 (Fig. 24.5a). The small lymphocytes are of both B- and T-cell lineages.
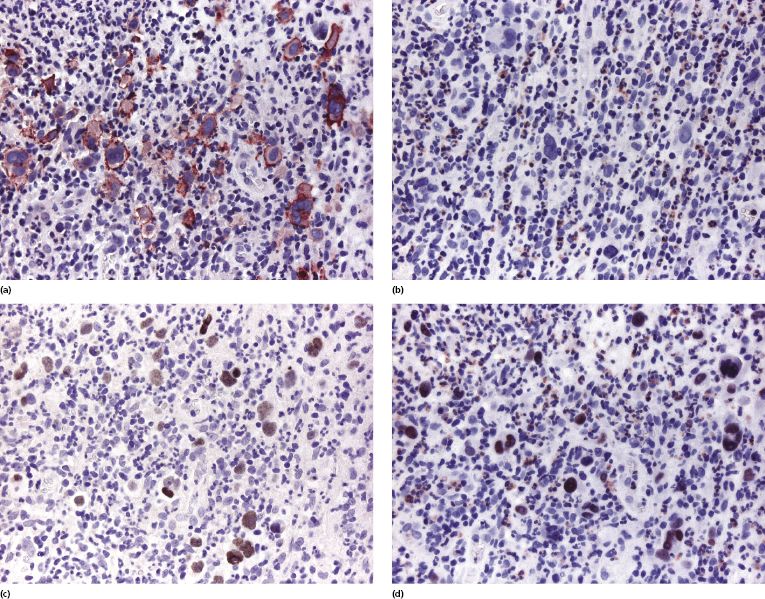
In the four subtypes of classical Hodgkin lymphoma neoplastic cells in the lymph nodes are only rarely positive for CD20 or CD79a. Staining for CD15 is usually positive in a proportion of the cells in the lymph nodes, but it may be negative in cutaneous lesions (Fig. 24.5b) [26, 28]. EBV can be detected in neoplastic cells by in situ hybridization in a subset of cases. Paired box gene (PAX)-5 is almost always positive in these subtypes, although sometimes with a weak staining pattern, confirming differentiation toward the B-cell lineage. Positivity for EBER-1 and PAX-5 can be observed also in specific cutaneous lesions (Fig. 24.5c and d), representing a good clue for differentiation of cutaneous classical Hodgkin lymphoma from other CD30+ T-cell lymphomas [29]. MUM-1 expression is also expressed by neoplastic cells, but positivity cannot be used for differentiation of Hodgkin lymphoma from simulators of it, as both lymphomatoid papulosis and cutaneous anaplastic large cell lymphoma are commonly positive. Zeta-chain-associated protein kinase 70 (ZAP-70), a protein that is part of the T-cell receptor, is positive in the majority of cases of anaplastic large cell lymphoma, but is consistently negative in Reed–Sternberg and Hodgkin cells [30]. Oct-2 and BOB.1, two markers that are usually strongly expressed in diffuse large B-cell lymphoma, are only focally and/or weakly expressed in cutaneous cases of classical Hodgkin lymphoma [29].
There are no molecular data on specific cutaneous manifestations of Hodgkin lymphoma. In the classical type, molecular analyses on microdissected Reed–Sternberg cells reveal clonal rearrangements of the immunoglobulin genes (molecular analyses of the entire biopsy specimen usually fail to reveal any clonality).
Treatment and Prognosis
Patients with specific cutaneous manifestations of Hodgkin lymphoma should be treated in a hematologic setting according to schemes tailored for the underlying disease. In the past, the prognosis for patients with skin manifestations of nodal Hodgkin lymphoma was poor in spite of aggressive treatment. Modern treatment modalities have resulted in a steady decline in the onset of specific skin manifestations, but cutaneous involvement has been reported rarely, even after successful allogeneic stem cell transplantation [8]. Since only occasional patients present with cutaneous involvement, there is little information on which to base both prognostic evaluation and therapeutic options. However, cutaneous Hodgkin lymphoma usually represents advanced (stage IV) disease and carries a bad prognosis. One recent case responded well to treatment [29]. Radiotherapy can be used to treat solitary or localized skin tumors.
As already mentioned, patients with “primary cutaneous” Hodgkin lymphoma most likely have lymphomatoid papulosis or cutaneous anaplastic large cell lymphoma, and thus should be managed conservatively with treatment modalities used for these conditions.

Full access? Get Clinical Tree


