21 Maximizing Safety with Microneedling
Abstract
Initially used in the treatment of scars, microneedling has been in use since the early 1990s. Since then, microneedling (once referred to as collagen induction therapy) has become a popular minimally invasive procedure for skin rejuvenation. Microneedles are used to penetrate the dermis and lead to percutaneous collagen, elastin, and capillary induction/reorganization. The needles used are on the order of microns, with needle length ranging from 0.5 to 1.5 mm. Microneedling can also work in synergy with a variety of drugs to augment transdermal delivery through micropores, among the most popular of which is platelet-rich plasma (PRP).
Key Points
Microneedling penetrates the dermis and initiates the body’s inflammatory and healing cascades, thus inducing a fluctuation of growth factors (FGF, TGF, and PDF) resulting in fibroblast activation and neocollagenesis, elastogenesis, and angiogenesis. 1 , 2 , 3
Within a week of microneedling, a fibronectin matrix scaffold develops, over which collagen organizes, ultimately leading to skin tightening. 3 , 4 , 5
Microneedling has been used successfully to treat acne scarring, nonacne scarring, hyperpigmentation, alopecia, and hyperhidrosis, as well as being used as a drug delivery technique. 2 , 3 , 4 , 5 , 6 , 7 , 8
Microneedling devices come in a variety of needle arrangements (e.g., tattoo devices, rollers, electronic devices) and materials (glass, silicone, metals, biodegradable polymers). The most commonly used methods for microneedling include rollers and electronic devices.
21.1 Safety Considerations
There is only one FDA-approved microneedling device currently on the U.S. market (SkinPen [Bellus Medical]).
The only FDA-approved use of microneedling is for atrophic scarring of the face (excluding within orbital rim).
SkinPen can be used in face/neck/body areas and is off label for use within the orbital rim. There are several different microneedling devices currently in practice, with a wide variety of needle quality and safety features. The SkinPen is the first to offer quality control research and data confirming their disposable needling tip device’s safety and quality.
Cross contamination of needles, and in turn bodily fluids, must be carefully controlled. Ideally, the microneedling device used should have a sealed hand-piece with a disposable microneedling unit for one-time use only. When combined with PRP, utmost care must be taken to systematically organize plasma and not inadvertently mix among patients.
Varying methods of anesthetic, including over-the-counter topical anesthetics, as well as specialty compounded formulations, are used to minimize patient discomfort. Under the direct supervision of a qualified medical provider, compounded topical formulations of analgesics can be used with caution. In our practice, when performing microneedling on multiple treatment areas, a staggering multistep approach with topical anesthetics is used to avoid lidocaine toxicity.
Cases of granulomas have been reported, particularly when using nonsterile preparations, topically in conjunction with micro needling. Ideally, only sterile products that are manufactured to be delivered intradermally should be applied on the surface when performing microneedling.
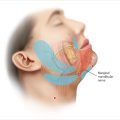
Needle depth can range from 0.25 mm to 3 mm depending on the device. An understanding of the anatomy of the treatment area is necessary to determine the safety of the needle depth. 1 , 2 , 7 Similar to chemical peel and laser safety, certain treatment areas are treated with a deeper depth of microneedling, while other treatment areas are treated with a shallower depth of needle penetration (▶ Fig. 21.1) (Video 21.1). 3 , 9 , 10
Devices that offer deeper microneedling settings (1.5 mm-3.0 mm) must be used with caution, particularly in patients with thin skin, as deeper needles (> 3mm) can cause sensory nerve damage.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree