2. Facial Analysis for Facelifting
It is a fundamental principle in surgery that surgeons must address the issues facing the patient before treatment. Therefore, in treating the patient who shows facial aging, a comprehensive analysis must be performed to ensure that as many of the patient’s concerns as possible are addressed.
It is particularly important that the rejuvenation procedure be tailored to the individual needs of the patient. Many surgeons are interested in a “cookbook recipe” for a procedure rather than an individualized approach to each patient’s particular needs. Such a “cookbook” approach will lead to suboptimal results in many cases.
Obviously, it is most important to listen to the patient’s concerns about his or her appearance. Most commonly, these concerns center on the appearance of the eyes and neck. We ask patients to bring in photographs of themselves when they were 15 years younger and they felt they looked good. These photographs can serve as a goal for the rejuvenation procedure and also demonstrate nicely the aging changes the procedure will address.
A careful medical history, including a detailed surgical history, is essential. It is important to obtain a complete list of prescription medications as well as over-the-counter medications that can cause bleeding during a procedure. Ask the patient about the use of nonprescription herbal medications that might also cause bleeding or anesthesia issues and about any known allergies. The patient’s history of smoking and of alcohol or illicit drug use is important because these substances could cause problems with flap viability or difficulties with anesthesia.
We begin first with a general assessment of the patient’s facial features and then with a review of all the findings from the facial analysis with the patient so that he or she can gain a detailed understanding of the procedures and any possible limitations to the procedures based on the examination. Assessment of the patient’s skin tone and the amount of actinic damage present in the skin is essential because patients who have significant actinic damage have reduced elasticity to their skin and are more prone to an earlier relapse of their aging changes because of this reduced elasticity; this susceptibility should be explained to the patient. 1 Other factors that lead to reduced elasticity of the skin include human immunodeficiency virus, or HIV, medications, corticosteroids, and a history of significant weight loss. Patients affected by any of these factors should understand that they may require an early secondary procedure.
The next assessment is that of the overall appearance of the face. In “attractive” faces, the facial thirds are generally balanced from menton to subnasale, subnasale to glabella, and glabella to hairline (trichion). 2 All patients have some degree of asymmetry to their faces: a wide side and a narrow side, one eye larger than the other eye, or the orbit on one side slightly higher. Other asymmetries may be present: eyebrow position, the nose, and the jaws (Fig. 2.1). These differences should be pointed out to the patient, along with the fact that all attractive faces are asymmetrical. Some asymmetries may be improved upon by surgery, but attempts to make the face completely symmetrical may actually result in an unnatural, strange effect.

In the event the patient decides to have a secondary facelift, it is essential to note any scars, both their location and their quality. The hairline needs to be carefully assessed to determine whether it has been displaced. When the hairline has already been displaced, the temporal incision will need to be made at the hairline to prevent further cephalic displacement of the hairline and a distorted appearance.
Appraisal of the hairline begins with the height of the forehead from the top of the eyebrows to the hairline. This information is important in determining the site and configuration of the incision if an open browlift is being considered. The hairline is evaluated for temporal recessions. The temporal hairline is evaluated for the distance from the lateral canthus as well as the direction of hair growth. The distance of the temporal hairline in a youthful-appearing patient is typically about three fingerbreadths (4.5 cm) from the lateral canthus. The color of the scalp skin is compared with the color of the facial skin in the temple area. Patients who have different-colored temporal skin and scalp skin may see a color change at the junction of the scalp skin and temporal skin when an incision is placed at the temporal hairline. When the temporal hair grows anteriorly or downward, the junction will be hidden by the hair. Hair that grows posteriorly reveals the junction of the temporal and scalp skin. These patients may require a few hair transplants into the area of the scar to hide the junction.
The next area to be examined is the eyebrows and forehead. The forehead is inspected for transverse rhytids related to frontalis muscle action. The glabella is inspected for vertical creases related to corrugator superciliaris muscle action, and the nasofrontal angle is examined for transverse nasal creases related to procerus and depressor superciliaris muscle action.
The aesthetic relationships of the brow are described by Westmore. 3 In women, the medial aspect of the brow begins in a line perpendicular to the lateral aspect of the nasal ala. The brow forms a gentle arch above the supraorbital rim peaking at the junction of the medial two-thirds with the lateral one-third. The lateral eyebrow ends on an oblique line extending from the lateral aspect of the nasal ala through the lateral canthus. The lateral aspect of the brow ends at approximately the same level as the medial brow. The apex of the eyebrow lies perpendicular to the lateral limbus. In men, the eyebrow has less of an arch and lies at the level of the supraorbital rim. When the lateral part of the eyebrow is depressed, it causes a sad and tired look in the patient. If the medial end of the eyebrow is depressed relative to the lateral brow, the result is an annoyed or angry look.
We begin with the patient sitting in the upright position. Using an eyebrow pencil, the position of the eyebrow at rest is marked in the medial, central, and lateral brow relative to the orbital rim. The patient is given a mirror, and the eyebrow is then placed into a position that is pleasing to the patient; marks are made again in the medial, central, and lateral brow relative to the orbital rim. The distances between the points are then measured and recorded.
Attention is next directed to the upper eyelids. The eyebrow is elevated to the previously marked position that creates a pleasing appearance. The upper eyelids are then inspected for excess sagging skin and the presence of herniated fat in the medial and central compartments. The position of the lower edge or margin of the upper eyelid relative to the upper edge of the iris reveals the presence of any upper eyelid ptosis.
Next the lower eyelids are assessed for tone using a snapback test or lower lid distraction test. 4 The superficial musculoaponeurotic system (SMAS) will give support to the lower eyelid. If a lower eyelid blepharoplasty is planned at the same time as the facelift procedure, consideration should be given to a lower eyelid tightening procedure for patients with poor lower eyelid tone. The amount of the herniation of the lower-eyelid fat pads should be assessed.
Evaluation of crow’s feet is made along with that of the upper and lower eyelids. Crow’s feet can be released and improved at the time of the facelift procedure by undermining the skin over the orbicularis oculi muscles up to the lateral canthus. Use a finger to stabilize the lateral brow, and ask the patient to smile. A muscle band may be seen running inferiorly from the lateral brow down along the lateral orbital rim (Fig. 2.2). Connell and Marten describe this muscle band as the depressor orbicularis lateralis. 5 The muscle segment is a powerful depressor of the brow and may lead to recurrent lateral eyebrow ptosis if it is not addressed at the time of the facelift. If a muscle band occurs with animation, it is important to divide the muscle obliquely along the lines of the crow’s feet creases.

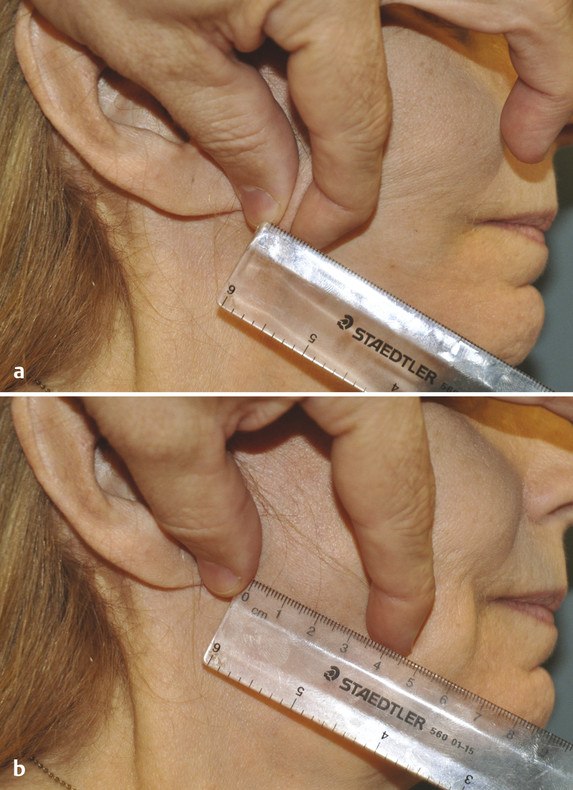
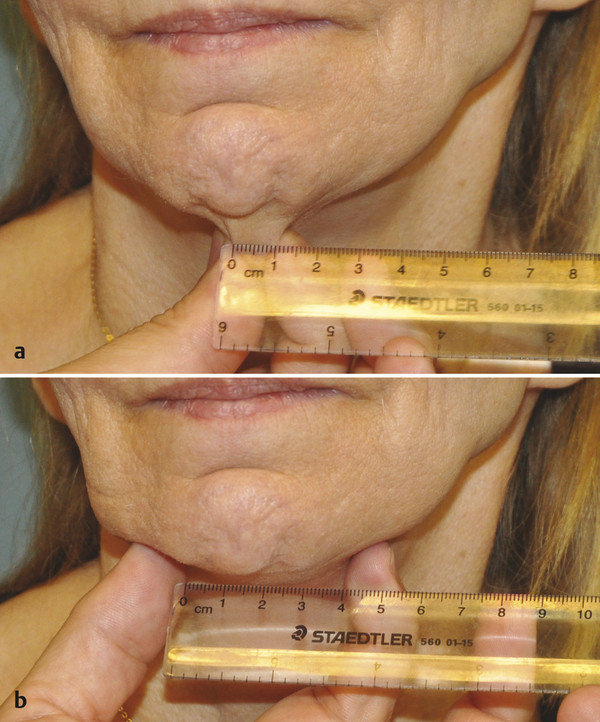
The amount of skin excess of the face is then measured in several locations. The amount of skin laxity is crucial in determining the placement of the incisions, especially in the temporal area. To measure skin laxity, an amount of skin is pinched together that re-creates the effect desired with the facelift, and the amount of skin between the fingers is measured. Then the skin is allowed to relax, and the amount is measured. The pinched skin measurement is then subtracted from the relaxed skin measurement, which determines the amount of skin excess.
The amount of skin excess in the face is measured in the temporal area (Fig. 2.3), anterior to the tragus (Fig. 2.4), and anterior to the earlobe (Fig. 2.5). A similar measurement is made in the vertical dimension in the cheeks (Fig. 2.6). Finally, skin pinches are made on one- half of the side of the neck and then in the midline to assess laxity across the entire neck (Fig. 2.7).
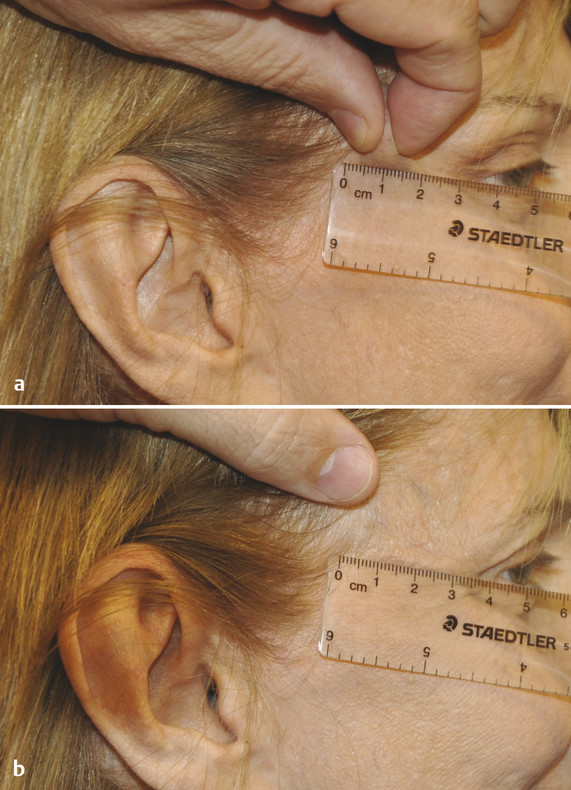
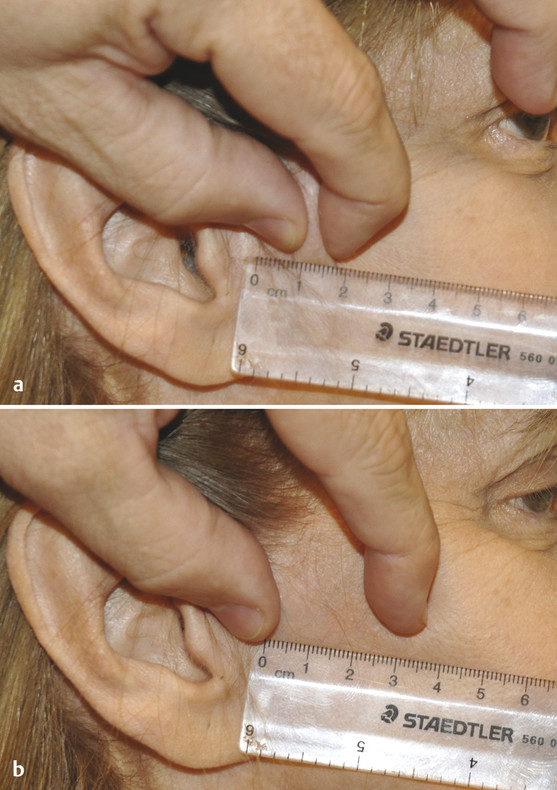

The use of skin pinches is crucial in determining the appropriate placement of the skin incisions. Patients who have a low sideburn and those with little skin laxity in the temple area and the upper cheek are good candidates for the temporal component of the facelift incision placed into the temporal hair.
Patients who naturally have a high sideburn or those with significant laxity in the temporal skin are better candidates for an incision placed at the temporal hairline. Another group of patients who frequently require an incision at the temporal hairline are those who need a secondary facelift. Secondary facelift patients frequently already have an elevated sideburn and widened distance between the lateral canthus and the temporal hairline. If the temporal element of the facelift incision is made into the hair in these patients, the distance of the hairline from the lateral canthus will be widened even more, and the sideburn will be elevated further. The result is the patient having a very unnatural and aged appearance. Instead of looking younger from the procedure, the patients actually look older.
The amount of skin available in the preauricular area is important, especially in the secondary facelift patient, whose skin shift is much more vertical than posterior. Thus, a patient who has had a previous facelift performed using a preauricular incision may not have enough skin laxity to allow for the scars being placed more posteriorly along the margin of the tragus.
Similarly, the amount of skin laxity and skin shift in the neck is critically important in planning the incision in the occipital area. When there is significant neck skin laxity and the incision is made into the occipital hair, there will be a shift of non–hair-bearing skin into the occipital and postauricular scalp because hair-bearing skin will be discarded to take up the laxity of the neck skin. It is for this reason that we typically place the incision in an S-shaped fashion along the occipital hairline.
The central face is then inspected. The main vector of aging is directed anteriorly and inferiorly. 6 The results are the characteristic changes seen in the aging face. In the malar areas, there is ptosis of the soft tissues off of the malar eminences. There is characteristically an edematous area over the malar eminences above the orbital septum. This area is pointed out to the patient and measured. The area may be improved with a facelift, but some residual fullness may remain after the surgery, and it is important to document this for the patient.
The inferior and anterior vectors of aging also lead to a deepening of the nasolabial creases. Traction on the SMAS in a posterior and superior direction will result in a flattening of the nasolabial fold and lessening in the depth of the nasolabial crease. 7 Additional techniques that may improve the nasolabial creases include fat transfer directly under the crease; in rare circumstances, a direct excision of the nasolabial crease may be indicated.
Patients may also develop downturned corners of their mouths. Women may complain that their lipstick will run out of the corners of the mouth and feel that they constantly have to dab at the corners with a tissue. Elevation and fixation of the SMAS in a posterior and superior direction can elevate the corners of the mouth without having to excise a triangle of skin, as described by Weston and colleagues. 8
Further inspection of the central face may demonstrate the presence of “marionette lines” and the presence of jowls. Just as the nasolabial fold can be flattened with elevation of the SMAS, the fold of skin and fat creating the marionette lines can be flattened, with resulting effacement of the marionette lines. The jowl can also be improved by releasing the mandibular ligaments along with traction on the SMAS to place the jowl back up into the cheek.
The mouth and chin areas are then examined for the presence of smoker’s lines around the lips. The lips are also inspected for lip ptosis, which may require a lip lift. Finally, the red lip is inspected for atrophy and thinning that may require some sort of augmentation.
Attention is next directed to the neck. The overall shape of the neck is observed. The cervicomental angle is analyzed to determine whether the neckline is defined or obtuse. There are many potential causes of the obtuse neck. The hyoid position may be low, which may result in a poorly defined cervicomental angle. There may be an abundance of adipose tissue in the neck, leading to poor definition of the neck. It is important to determine the location of this fat, whether it is supraplatysmal or subplatysmal. Finally, the platysma muscle may be tight and tenting from the mandible down to the base of the neck, which leads to a poorly defined cervicomental angle.
When the general skin tone is observed, the presence of transverse skin creases with dermal and platysmal muscle defects is noted. Generally, the level of undermining of the skin in the neck is below the lowest dermal- deficiency crease. If loose, crepe paper–like skin is noted in the central neck, it is measured. This area generally improves with the facelift and neck lift, but this problem can return over time, and the patient needs to be advised of this possibility.
Further examination of the neck notes the presence and location of platysmal bands, including an assessment of the tone of the bands, which helps to determine the need (or not) for transection of the platysma. The patient is asked to grimace while the neck is inspected, a maneuver that helps to determine whether the fat is above or below the platysma muscle.
Palpation of the neck is then performed, including the position of the hyoid bone, and the position is noted. The size and position of the submandibular glands and the position of the cricoid cartilage are then recorded. An assessment is made regarding the size of the digastric muscles. In a thin neck, the muscle can be observed on the lateral view defining the lower border of the submandibular triangle. In the obtuse neck, the digastric muscle may contribute to the poorly defined neck, and a tangential excision may be necessary, along with supraplatysmal and subplatysmal lipectomies, to achieve a refined neckline.
Using a comprehensive checklist makes it possible to achieve excellent results in facial rejuvenation procedures.
References
[1] Sundine MJ, Kretsis V, Connell BF. Longevity of SMAS facial rejuvenation and support. Plast Reconstr Surg 2010; 126 : 229-237 [2] Farkas LG, Hreczko TA, Kolar JC, Munro IR. Vertical and horizontal proportions of the face in young adult North American Caucasians: revision of neoclassical canons. Plast Reconstr Surg 1985; 75 : 328-338 [3] Ellenbogen R. Transcoronal eyebrow lift with concomitant upper blepharoplasty. Plast Reconstr Surg 1983; 71 : 490-499 [4] Hinderer UT. Aesthetic surgery of the eyelids and periocular region. In: Smith JW, Aston SJ, eds. Plastic Surgery. 4th ed. Boston: Little Brown; 1991:565–608 [5] Connell BF, Marten TJ. Surgical correction of the crow’s feet deformity. Clin Plast Surg 1993; 20 : 295-302 [6] Yousif NJ. Changes of the midface with age. Clin Plast Surg 1995; 22 : 213-226 [7] Sundine MJ, Connell BF. Analysis of the effects of subcutaneous musculoaponeurotic system facial support on the nasolabial crease. Can J Plast Surg 2010; 18 : 11-14 [8] Weston GW, Poindexter BD, Sigal RK, Austin HW. Lifting lips: 28 years of experience using the direct excision approach to rejuvenating the aging mouth. Aesthet Surg J 2009; 29 : 83-86Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree