17 The Management of Brow Ptosis
Abstract
“The Management of Brow Ptosis” describes the treatments that can be used when the position of the eyebrows, which affects facial expression and influences the way in which others judge a patient’s mood and personality, has become lower with age because of gravity, soft tissue deflation, and the actions of eyebrow depressor muscles. Patients often attempt to raise ptotic eyebrows by using the frontalis muscle; this action eventually becomes involuntary and leads to a paradoxical rise in the central eyebrow position of some older patients. A rise in the brows with age can also occur as an involuntary reflex compensatory mechanism to overcome the effects of an involutional bilateral blepharoptosis. Brow ptosis can create an apparent skin redundancy in the upper eyelids and in the medial and lateral canthal areas. This can lead to the appearance of more severe upper eyelid dermatochalasis centrally, hooding of the eyelids temporally, and skin redundancy medially. It is important to recognize brow ptosis and to determine its most appropriate management for the individual patient. This may also include accepting the brow ptosis, particularly in a male patient, but modifying an upper eyelid blepharoplasty to prevent the brow from being drawn down more to meet the upper eyelid incision. This can otherwise lead to a very unsatisfactory postoperative appearance.
17.1 Introduction
The position of the eyebrows affects facial expression and influences the way in which a patient’s mood and personality are judged by others. There are a variety of eyebrow shapes. In general, the female eyebrow has a higher arch than a man’s, which tends to be flatter (Fig. 17‑1a,b). The eyebrow position tends to become lower with age from the effects of gravity, soft tissue deflation, and the action of the depressors of the eyebrow (the corrugator supercilii, the depressor supercilii, the procerus, and the orbicularis oculi muscles). The brow may become ptotic to a very variable degree (Fig. 17‑1c).

Patients often attempt to raise ptotic eyebrows by using the frontalis muscle. This action eventually becomes involuntary and leads to a paradoxical rise in the central eyebrow position of some older patients. A rise in the brows with age can also occur as an involuntary reflex compensatory mechanism to overcome the effects of an involutional bilateral blepharoptosis. Brow ptosis can create an apparent skin redundancy in the upper eyelids and in the medial and lateral canthal areas. This can lead to the appearance of more severe upper eyelid dermatochalasis centrally, hooding of the eyelids temporally, and skin redundancy medially. It is important to recognize brow ptosis and to determine its most appropriate management for the individual patient. This may also include accepting the brow ptosis, particularly in a male patient, but modifying an upper eyelid blepharoplasty to prevent the brow from being drawn down more to meet the upper eyelid incision. This can otherwise lead to a very unsatisfactory postoperative appearance.
Key Point
A rise in the brows with age may occur as an involuntary reflex compensatory mechanism to overcome the effects of an involutional bilateral blepharoptosis.
17.2 Applied Anatomy
17.2.1 Eyebrow
The applied anatomy of the eyebrows, the eyebrow elevator and depressor muscles, the scalp, the temple, and the facial nerve is presented in detail in Chapter 2. This anatomy should be carefully reviewed.
17.3 Preoperative Patient Evaluation
17.3.1 History
The patient’s complaints should be carefully noted. The patient may complain of the following:
Drooping or hooding of the upper eyelids.
A loss of the superior visual field.
A tired appearance commented on by others.
Headaches.
Ocular discomfort.
The complaint of drooping of the upper eyelids may simply be related to severe dermatochalasis causing a pseudoptosis, with the underlying eyelid height being normal. The lid position should be carefully evaluated, however, because a true blepharoptosis may also be present. Similarly, a severe dermatochalasis, often combined with a brow ptosis, may obstruct the patient’s superior visual field. Often, patients will have a more significant lateral brow ptosis than true dermatochalasis of the upper eyelids, and a browlift combined with an upper eyelid blepharoplasty may be required for such a patient.
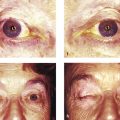
Patients who have a moderate-to-severe brow ptosis and dermatochalasis are obliged to use their frontalis muscle to overcome the superior visual field defect. Such patients commonly develop deep forehead furrows (Fig. 17‑2).

This leads to fatigue of the frontalis muscle, which in turn can cause a headache. The cosmetic effects of upper eyelid dermatochalasis and a brow ptosis can lead to complaints of a tired appearance. Occasionally, upper eyelid dermatochalasis and a severe lateral brow ptosis can lead to a secondary mechanical misdirection of eyelashes, causing chronic ocular discomfort.
Patients should be specifically questioned about previous periocular botulinum toxin injections and facial rejuvenation surgery. Patients who have previously undergone such injections, a cosmetic blepharoplasty, or a facelift may omit such information, particularly if accompanied by a new partner.
A history of contact lens wear, dry eye, a previous facial palsy, or thyroid dysfunction identifies a patient at risk of exposure keratopathy symptoms after an upper lid blepharoplasty. It is important to exclude a bleeding disorder, because a postoperative hemorrhage after a blepharoplasty is potentially sight-threatening. Previously undiagnosed hypertension should be excluded. Any allergies should be noted. The use of aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) should be discontinued 2 weeks before surgery.
17.3.2 Examination
The patient should undergo a complete ophthalmic examination. The patient’s best-corrected visual acuity should be recorded. The patient should be assessed in a sitting position with the eyes looking straight ahead. The palpebral apertures should be measured and the position of the skin creases recorded as described in Chapter 15. Any asymmetry of the brows should be noted. Any frontalis overaction should also be noted and the position and shape of the brows assessed after preventing frontalis overaction. The degree of mobility of the brows associated with gentle downward traction of the upper eyelid skin is assessed. Any subcutaneous soft tissue atrophy is sought immediately above the brow and in the adjacent temple. The secondary effects of brow ptosis on the upper eyelids must be recognized. In addition, it may be difficult to ascertain the true position of the brow in patients who pluck their eyebrows or who have their eyebrows threaded or tattooed. This can lead to an overresection of skin when undertaking an upper lid blepharoplasty if great care is not taken in this assessment.
Key Point
The secondary effects of brow ptosis on the appearance of the upper eyelids must be recognized.
The position of the hairline should be noted and any thinning of the hair documented. The vertical height of the forehead from the apex of the brow to the hairline is noted, as is any notable prominence of the frontal bone. (A patient with a high forehead, thinning of the hair, and a prominent frontal bone may be an unsuitable candidate for an endoscopic browlift procedure. Such a procedure is more difficult to perform in such a patient, and the procedure risks causing permanent damage to hair follicles in the anterior scalp area.)
An assessment of tear production and the tear film should be documented. The degree of upper eyelid laxity is assessed. Any herniation of medial and central upper eyelid fat is noted. The degree of excess upper eyelid skin is assessed. The skin quality and degree of actinic damage is assessed. Any prolapse of the lacrimal gland is noted.
Key Point
It may be difficult to ascertain the true position of the brow in patients who pluck their eyebrows or who have their eyebrows threaded or tattooed. This can lead to an overresection of skin when undertaking an upper lid blepharoplasty if great care is not taken in this assessment.
17.4 Surgical Planning
The options for surgical and nonsurgical management should be discussed in detail with the patient. Some patients, in particular dysthyroid patients with a medial brow ptosis and deep glabellar frown lines, may prefer the use of botulinum toxin instead of surgery. This is highly effective for such patients, whose glabellar furrows can create an aggressive appearance. It has the disadvantage, however, of being expensive and temporary in its effects. It has to be repeated every 3 to 4 months. The use of botulinum toxin in a cosmetic patient does, however, offer the following advantages:
Botulinum toxin injections to the brow depressor muscles can effect a “chemical browlift” in some patients without the need for surgery.
Botulinum toxin injections to the brow depressor muscles given 2 weeks before an endoscopic browlift procedure, or a transblepharoplasty browpexy or browlift procedure, can enhance the long-term results of the procedure (the injections should not be given at the time of the procedure, because postoperative edema can carry the toxin to the levator palpebrae superioris, resulting in a blepharoptosis that can last for 3–4 months).
Key Point
Botulinum toxin injections should never be given at the time of surgery or closer than 2 weeks to the time of surgery, because postoperative tissue edema can carry the toxin to the levator palpebrae superioris muscle, resulting in a blepharoptosis.
The use of botulinum toxin injections for cosmetic patients is described in detail in Chapter 14.
Botulinum toxin injections can be combined with the use of a dermal filler or structural fat grafting to reinflate the soft tissues of the lateral brow and to address any associated hollowing of the adjacent temple. This is discussed in Chapter 14.
The goals, limitations, risks, and potential complications of surgery should be fully discussed with the patient. The patient should be fully informed about the sites of incisions and resultant scars. Risks specific to the surgical approach should be explained: neurosensory loss or annoying paresthesia and itching in the distribution of the supraorbital and supratrochlear nerves, loss of hair around scalp incisions, palpability of any implants used for brow fixation after elevation, frontalis palsy from damage to the temporal branch of the facial nerve, and persistent headache.
The limitations of an upper eyelid blepharoplasty performed alone in the presence of a significant brow ptosis should be explained. Under these circumstances, an upper eyelid blepharoplasty should be very conservative to prevent further lowering of the brow and an unsatisfactory appearance, or the patient should undergo a brow fixation procedure such as a suture browpexy to stabilize the position of the brow. When taking the initial history, patients should be carefully questioned to ascertain their goals and their expectations of surgery.
The patient should also be shown the potential effects of a browlift on the sub-brow skin. In some patients with significant age-related soft tissue deflation, a browlift can induce oblique skin lines in this area that are aesthetically displeasing. The patient must be made aware of this possibility, which may require the additional use of dermal filler injections or structural fat grafting.
Key Point
Consider the potential benefits of botulinum toxin injections in patients with a brow ptosis, either as an alternative to surgery or to supplement the effects of surgery.
17.4.1 Anesthesia
Browlift procedures may be performed with either general or local anesthesia, or under local anesthesia with intravenous sedation. The patient should be kept in a semirecumbent position with the head elevated at least 30 degrees to reduce venous engorgement and bleeding. The use of tumescent anaesthesia offers significant advantages for some browlift procedures (Box 17.1).*
Box 17.1
Tumescent local anesthetic solution: a 50 mL syringe filled with 0.25 mL of 1:1000 adrenaline, 30 mL of normal saline, 10 mL of 2% lignocaine, and 10 mL of 0.5% bupivacaine.
17.5 Surgical Procedures for The Management of Brow Ptosis
There are a variety of surgical procedures for the management of eyebrow ptosis, including the following:
The direct browlift.
The temporal direct browlift.
The “gull-wing” direct browlift.
The midforehead browlift.
The temporal browlift.
The transblepharoplasty browpexy.
The transblepharoplasty browlift.
The endoscopic browlift.
The coronal forehead and browlift.
The pretrichial forehead and browlift.
The lateral subcutaneous forehead and browlift.
The suture browlift.
In my practice the temporal direct browlift and the endoscopic browlift are the most commonly performed surgical procedures.
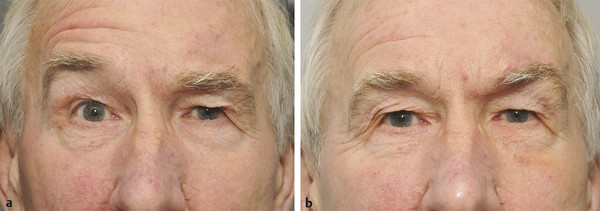
17.5.1 Direct Brow Lift
A direct browlift is a simple surgical technique that is suitable for older patients with functional rather than cosmetic concerns in whom the surgical scar can be hidden within natural creases and for patients with a severe brow ptosis related to a facial palsy. It can be performed quickly under local anesthesia with or without any sedation and can be combined with an upper lid blepharoplasty. Patients should be warned about the visibility of the postoperative scars and should be shown examples using photographs of other patients’ results at their consultation (Fig. 17‑3).
Surgical Procedure
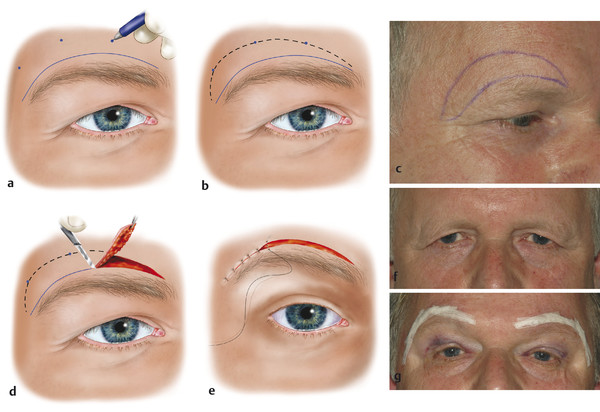
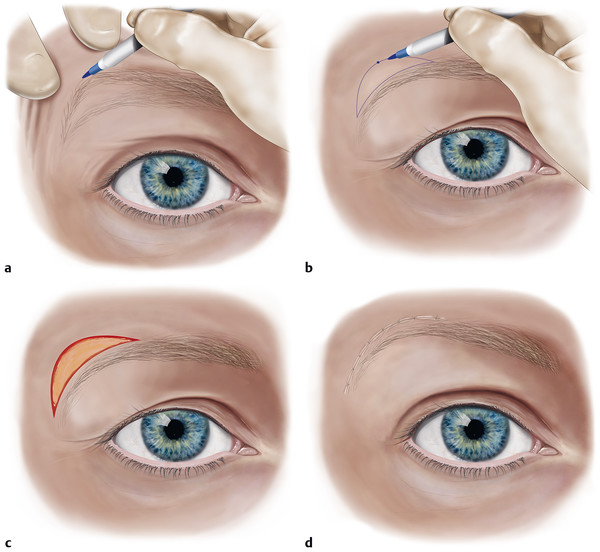
With the patient in a sitting position, an incision is marked just above the eyebrow with a gentian violet marker pen. The brow is mechanically elevated to the desired level and then released. A mark is then made on the forehead at a point that represents the leading edge of the raised brow (Fig. 17‑4a).
A slight overcorrection is desirable. An elliptical incision is then drawn out (Fig. 17‑4b).
If the browlift is to be combined with an upper lid blepharoplasty, the proposed blepharoplasty incisions should be marked out with an assistant raising the brow to the desired position to avoid overresection of upper eyelid skin.
The shape of the proposed area for excision can be adjusted according to the desired shape of the brow. For a marked temporal brow ptosis, the incision is modified and kept over the lateral brow only (Fig. 17‑5). A lateral “dog-ear” can be addressed with a “winged” extension to the incision if required.
The marked out area is infiltrated with 8 to 10 mL of 0.5% bupivacaine with 1:200,000 units of adrenaline mixed 50:50 with 2% lidocaine with 1:80,000 units of adrenaline.
A perpendicular incision is made through the skin and subcutaneous tissue with a no. 15 Bard–Parker blade down to the level of the frontalis and orbicularis muscles (Fig. 17‑4c). Great care should be taken medially to avoid any damage to the supraorbital and supratrochlear neurovascular bundles. For a cosmetic patient undergoing a temporal direct browlift, the skin and very superficial subcutaneous tissue only are removed, helping to maintain soft tissue volume in this area. With this approach there is no risk of any postoperative sensory loss, even in a patient with aberrant lateral branches of the supraorbital nerve.
The ellipse of tissue is excised and the wound is closed with buried interrupted subcutaneous 5–0 Vicryl sutures. The skin is closed with interrupted 7–0 Vicryl Rapide sutures, which pick up the edges of the skin (Fig. 17‑4d,e). These do not leave visible suture marks in the skin. (Alternatively, the skin can be closed with a subcuticular 5–0 nylon suture.) The skin closure is reinforced with sterile adhesive tape (Steri-Strips) (Fig. 17‑4f,g).
Normal saline sachets should be kept available in the refrigerator and used to moisten 4-by-4 gauze swabs, which are applied to the first operated side while the fellow side is undergoing the same procedure.

Postoperative Care
Postoperatively the patient is prescribed a topical antibiotic ointment to the brow wounds three times a day for 2 weeks. The patient is instructed to sleep with the head elevated for 3 to 4 weeks and to avoid lifting any heavy weights for 2 weeks. Clean cool packs are gently applied to the brow intermittently for 48 hours. The patient is instructed to remove the adhesive tape from the wounds after 2 to 3 days. The skin sutures are removed approximately 10 days postoperatively.
17.5.2 Temporal Direct Brow Lift
A temporal direct browlift is particularly effective to manage a temporal brow ptosis and can also yield a good cosmetic result in patients older than 50 to 55 years of age. It is not suitable for younger patients. It can also be used to address asymmetries in the position of the brows (Fig. 17‑5).
The procedure is often combined with an upper lid blepharoplasty, and the browlift can help to prevent a visible lateral extension of the blepharoplasty scar (Fig. 17‑6).

The resultant scar, confined to the lateral half of the eyebrow only, is far preferable to a scar that extends to the medial aspect of the brow. In addition, a temporal direct brow lift poses no risk to the supraorbital and supratrochlear nerves. If a significant amount of tissue has to be resected, however, temporal peaking of the brows can occur, particularly if the patient continues to exhibit involuntary frontalis overaction. The procedure offers the advantage of a long-lasting result. It can be used for patients who prefer to avoid the use of botulinum toxin injections, although these can be used in these patients to reduce frown lines and to help to maintain a satisfactory height and contour to the brows. There is also anecdotal evidence to suggest that such injections may also help with the appearance of the scars by inhibiting fibroblast activity.
Surgical Procedure
This is as described for a direct browlift, except that the incision is modified and kept over the lateral brow only (Fig. 17‑7, Video 17.1).
Postoperative Care
Postoperative care is as described for a direct browlift.
Key Point
If a browlift is to be combined with an upper lid blepharoplasty, the proposed blepharoplasty incisions should be marked out, with an assistant raising the brow to the desired position to avoid an overresection of upper eyelid skin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree