11 Speech/Resonance Evaluation
Introduction
Children with a history of cleft lip and/or palate are at risk for communication disorders in the areas of speech, resonance, voice, and even language. These disorders are due to a variety of structural causes, including velopharyngeal insufficiency (VPI). The purpose of this chapter is to describe the clinical and instrumental evaluation that is typically performed by the speech-language pathologist as part of the care of the child with cleft lip/palate. (Note that because some readers may be unfamiliar with specialized phonetic symbols, Standard English letters are used for clarity.)
Causes of Communication Disorders in Children with Cleft Lip/Palate
Children born with cleft lip and palate are at risk for disorders of speech sound (articulation disorder), language, resonance (hypernasality, hyponasality, or cul-de-sac resonance), and even voice (dysphonia). There are several potential causes of speech/language delays and communication disorders in children with cleft lip and palate. These include dental and/or occlusal abnormalities, vocal tract obstruction, hearing loss, and VPI. These causes are further discussed in the following text.
Dental and/or Occlusal Abnormalities
Children with a cleft of the primary palate that extends into the alveolar ridge will often have dental and/or occlusal abnormalities. Dental anomalies, particularly supernumerary or displaced teeth, can interfere with tongue tip movement during speech production. Malocclusion is an even greater concern for speech. This is because it can affect the normal relationship between the tongue tip and the alveolar ridge ( Fig. 11.1 ).
Whenever there are structural abnormalities within the vocal tract, this can cause either obligatory distortions or compensatory errors. Obligatory speech distortions occur when the articulation placement is correct, but an abnormality of the structure results in a distortion of speech.1,2 Obligatory distortions are common with dental/occlusal anomalies, and often cause distortion of sibilant sounds (s, z, sh, ch, j). In contrast, compensatory speech errors are the result of incorrect articulatory placement in response to abnormal structure.1,2 An example of a compensatory error is when the production of the sounds “t” or “d” is altered from the normal placement (tongue tip to alveolar ridge) to an abnormal placement (dorsum of the tongue to the palate). This commonly occurs in response to an anterior crossbite.
Definitions of Common Terms
Velopharyngeal dysfunction (VPD) is the inability of the velum to completely close the nasal cavity from the oral cavity during the production of oral (nonnasal) sounds.
Velopharyngeal insufficiency (VPI) describes an anatomic or structural defect that prevents adequate velopharyngeal closure, and the most common type of VPD.
Velopharyngeal incompetence (also VPI) refers to poor movement of the velopharyngeal structures caused by a neurophysiological disorder.
Velopharyngeal mislearning describes an articulation placement disorder that includes the substitution of nasal or pharyngeal sounds for oral sounds, resulting in an open velopharyngeal valve during the production.
Obligatory speech distortions occur when the articulation placement is correct, but an abnormality of the structure results in a distortion of speech.1,2
Obligatory distortions are common with both VPI and dental/occlusal anomalies, and often cause distortion of sibilant sounds (s, z, sh, ch, j).
Compensatory speech errors are the result of incorrect articulatory placement in response to abnormal structure. Some examples:
Glottal stop: a sound made by forceful closing the vocal cords and opening, such as pronounced with “uh-oh.”
Pharyngeal plosive: sound produced by tongue base against posterior pharyngeal wall while the tongue is held low in the oral cavity.
Pharyngeal fricatives: produced when air is forced through the narrowed pharyngeal airway, creating a turbulent sound. The tongue is held close to the posterior pharyngeal wall and the walls narrowed.
Posterior nasal fricatives: a nasal snort that is coarticulated with a pressure consonant.
Phoneme represents the smallest unit of a language′s phonology (speech sound) system.
Hypernasality is a type of resonance disorder that occurs when too much sound is transmitted through the nasal cavity during speech.
Hyponasality is a type of resonance disorder that occurs when obstruction in the nasopharynx or nasal cavity prevents sound from resonating in the nasal cavity during speech and is noted during the production of nasal consonants (m, n, ng).
Cul-de-sac resonance is a resonance disorder that is the result of a structural obstruction preventing sound from exiting the pharynx, oral cavity, or nasal cavity.
Mixed resonance occurs when there is hypernasality on oral consonants and hyponasality on nasal consonants. This can be due to a combination of VPI and nasopharyngeal obstruction.

Hearing Loss
Children with cleft palate are at increased risk for both conductive and sensorineural hearing loss.3–5 The cleft palate can cause abnormalities of the tensor veli palatini muscles, which are responsible for eustachian tube function. Eustachian tube dysfunction can result in chronic middle ear effusion and fluctuating conductive hearing loss. Fluctuating conductive hearing loss can cause a delay in speech and/or language development, but this delay is usually resolved quickly with treatment. Prophylactic insertion of pressure equalizer tubes is therefore often done in patients with cleft palate.
Children with cleft palate and associated craniofacial syndromes (i.e., Treacher Collins syndrome) are also at risk for anomalies of the external, middle, and inner ear. As a result, they may demonstrate a more significant conductive hearing loss and/or a sensorineural hearing loss. These types of hearing loss have a greater and more long-lasting effect on speech and language development.
Upper Airway Obstruction
Children with cleft lip and palate are at risk for upper airway obstruction for many reasons.6 Those born with Pierre Robin sequence, including micrognathia and glossoptosis, tend to have a very small oropharynx, which primarily affects respiration, but can also affect resonance. Children with unilateral cleft lip and palate often have a deviated septum. For older children and adults, the size of the nasal cavity and the depth of the pharynx may be affected by maxillary retrusion. Regardless of the cause, upper airway obstruction can cause hyponasality or cul-de-sac resonance.
Velopharyngeal Insufficiency
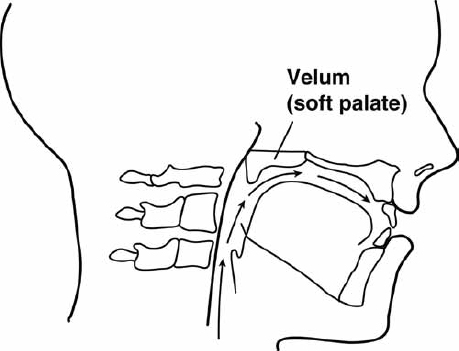
The primary purpose of a palate repair is to achieve normal velopharyngeal function for speech. As such, there is firm closure of the velum against the pharyngeal wall during the production of all oral sounds ( Fig. 11.2 ). The greatest concern for children with cleft palate is the risk for VPI.7 Despite undergoing palatoplasty surgery, 20 to 30% of children with repaired cleft palate will demonstrate some degree of velopharyngeal dysfunction (VPD), resulting in abnormal speech.
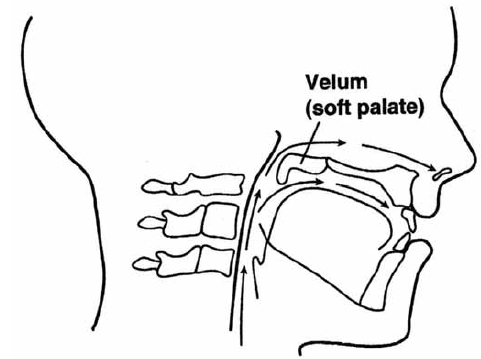
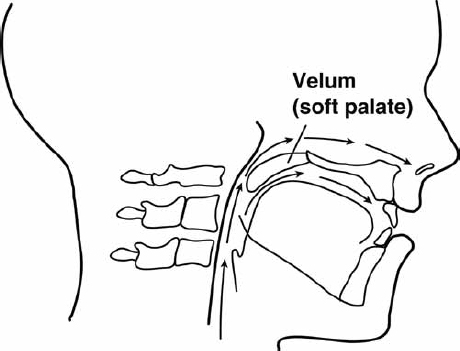
A word about terminology may be appropriate here. The term velopharyngeal dysfunction (VPD) is a general term that refers to the inability of the velum to completely close the nasal cavity from the oral cavity during the production of oral (nonnasal) sounds. Other terms are used to indicate a general causality.1,8,9 The term velopharyngeal insufficiency (VPI) is typically used to describe an anatomic or structural defect that prevents adequate velopharyngeal closure. VPI is the most common type of VPD because it includes the causes of cleft palate and submucous cleft palate ( Fig. 11.3 ). In contrast, the term velopharyngeal incompetence (also abbreviated VPI), is used to refer to a neurophysiological disorder that causes poor movement of the velopharyngeal structures ( Fig. 11.4 ). Both forms of VPI require surgical or prosthetic management. Finally, velopharyngeal mislearning is a term to describe an articulation placement disorder that includes the substitution of nasal or pharyngeal sounds for oral sounds, resulting in an open velopharyngeal valve during the production. Children with VPI often develop compensatory productions (a form of velopharyngeal mislearning), which require speech therapy after physical correction of the abnormal structure. These types of VPD are further outlined in Table 11.1 . Note that when the abbreviation VPI is used, it refers to velopharyngeal insufficiency and incompetence (both of which require physical management) in contrast to velopharyngeal mislearning (which requires speech therapy only).
Clinical Assessment
Patient History
Prior to the perceptual evaluation of resonance and velopharyngeal function, the examiner should obtain a thorough history through chart review, a pre-evaluation questionnaire (if possible), and a family (or patient) interview.10,11 In particular, it is important to determine information in the following general categories:
Current concerns of the parents and other family members
Diagnoses
Surgical history
Feeding/swallowing history
Motor developmental history
Speech/language/learning developmental history
Airway history
Previous or current speech therapy
Speech Samples for Assessment
Choosing appropriate speech samples for the assessment is very important, and key to obtaining information needed for a definitive diagnosis. Separation of the oral speech samples from the nasal speech samples during testing allows the examiner to isolate the type of abnormal resonance, when it occurs. For children, the speech samples should also be developmentally appropriate in areas of content, speech sound production, and syntax. Children are generally ready for this level of testing around the age of 3 years old.
Single Word Articulation Tests
Because speech sound production is negatively affected by both dental/occlusal anomalies and VPI, an articulation test is a necessary part of the assessment. There are two formal articulation tests that were specifically designed to assess patients with possible VPD: the Iowa Pressure Articulation Test, a part of the Templin-Darley Tests of Articulation,12 and the Bzoch Error Patterns Diagnostic Articulation Test.13,14 These tests focus on words with the pressure-sensitive phonemes that are particularly affected by VPD. (A phoneme represents the smallest unit of sound created in a language that can convey a specific meaning.) However, any articulation test can be used.
Although a formal, single-word articulation test is routinely done by many clinicians, normal speech does not consist of isolated single words. In addition, velopharyngeal function, and even articulation, may be normal at the single word level, but abnormal in connected speech, which increases the demands on the oral-motor system. Therefore, it is far better (and actually much easier) to assess articulation through syllable repetitions and repeated sentences.
Syllable Repetition
The use of syllable repetition as part of the speech assessment allows the examiner to isolate a single consonant and single vowel while eliminating the effects of other contiguous phonemes. At the same time, the child is producing sounds in a way that simulates the motoric demands of connected speech.1,9,15 Isolating sounds in this way makes it easier to note specific errors on consonants. It also allows the examiner to clearly identify phoneme-specific nasal emission on consonants, or phoneme-specific hypernasality on vowels.
As part of the syllable repetition test, the child is asked to produce consonants in a repetitive manner (i.e., “pa pa pa pa pa,” “pee pee pee pee pee,” “ta ta ta ta ta,” “tee tee tee tee tee,” etc.). Particular attention is paid to pressure-sensitive phonemes, which may be substituted by a compensatory production, nasalized, or produced with nasal emission. Consonants should be tested with both a low vowel (i.e., “a” as in “father”) and then again with a high vowel (i.e., “ee” and in “heat”) for comparison. This is because phoneme-specific nasality can occur on high vowels due to the high posterior tongue position in normal production.
Sentence Repetition
A very effective way to test articulation and velopharyngeal function is to use a battery of sentences that the patient can repeat. It is preferable to use sentences that contain phonemes that are similar in articulatory placement (e.g., “Pick up the book,” “Take teddy to town,” “Do it for daddy,” “Go get the cookie,” “Fred has five fish,” etc.). By asking the patient to repeat certain sentences, the examiner can quickly and easily assess articulation, nasal emission, and even resonance in a connected speech environment.
Sentences that contain many pressure-sensitive consonants, particularly those that are voiceless (i.e., “Sissy sees the sun in the sky”) are most sensitive to nasal emission and the other related characteristics (weak consonants or short utterance length). Sentences with a high number of voiced, oral sounds and fewer pressure sounds (i.e., “How are you?”) are more sensitive to hypernasality. Sentences with a high frequency of nasal phonemes (i.e., “Mama made lemonade”) are most sensitive to hyponasality.
Counting
Counting can provide the examiner with a fast, easy, and reliable screening test. A good test of hypernasality and/or nasal emission is counting from 60 to 70 or repetition of the numbers 60 or 66. The number 66 is particularly good to use because it contains several/s/sounds, the high vowel “eee,” and several/s/blends (/kst/and/ks/), all of which tax the velopharyngeal mechanism. To test for hyponasality, counting from 90 to 99 allows the examiner to assess the production of the nasal/n/in connected speech.
Spontaneous Connected Speech
Listening to spontaneous connected speech should always be done as part of the assessment. This is because, in comparison to single words and even short utterances, this type of speech requires a greater demand on the velopharyngeal system for rapid and efficient opening and closing of the valve. As a result, hypernasality, nasal emission, and even articulation errors are likely to be more prevalent in connected speech than in single words or single sentences.
What to Assess
Several authors have suggested specific protocols, rating scales, and recording procedures for speech assessment of children with a history of cleft palate.1,16–22 Unfortunately, there is not yet a standard assessment protocol that is used universally. This affects the ability to compare outcome results of cleft palate surgery and surgery for velopharyngeal insufficiency. However, the use of standard rating scales and recording procedures is not as critical when assessing individual patients to determine appropriate recommendations for treatment.
Articulation
As part of a standard articulation test, the examiner typically records all misarticulations and determines which are placement errors, errors due to oral-motor dysfunction, or developmental errors. When there are structural abnormalities (e.g., VPI or malocclusion), the examiner must also determine if there are compensatory errors or obligatory distortions.
As noted previously, compensatory articulation productions are often developed when there are dental/occlusal anomalies or inadequate intraoral air pressure for production of consonant sounds due to VPI.23 For example, when there is interference with tongue tip movement from the anterior teeth, the examiner should look for the dorsum of the tongue articulating against the palate. When there is VPI, the examiner should determine whether sounds are produced in the pharynx where there is a greater amount of air pressure.
Common compensatory productions for VPI include glottal stops, pharyngeal plosives, pharyngeal fricatives, and posterior nasal fricatives. These productions can often be coarticulated with the correct oral sound. Therefore, the examiner must determine if there is a coarticulation with each sound. For example, the examiner can determine if a glottal stop is being coarticulated with the oral sound by looking for a contraction at the neck, or even feeling the neck during sound production. Pharyngeal fricatives and nasal fricatives can be difficult to distinguish for an inexperienced listener. However, the truth is that it doesn′t matter because the treatment is the same.
Obligatory distortions secondary to VPI include hypernasality and nasal emission. In addition, some oral phonemes will sound like their nasal cognates (i.e., “m” for “b,” “n” for “d,” “ng” for “g”). It should be remembered that obligatory distortions (including hypernasality and nasal emission) cannot be corrected with speech therapy.23
Once all articulation errors are recorded, the examiner should test stimulability. In general, if the individual can produce the correct speech phoneme without nasality after instructions on changing placement, this is a good prognostic indicator for correction with therapy.7 On the other hand, if nasality occurs with normal articulation placement, this strongly suggests VPI, which requires surgical correction. If the patient has compensatory errors as a result of VPI, it is usually best to correct the structural defect first, and then initiate therapy to correct the faulty placement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree