11 Inferior Turbinate Flap
Summary
There are many surgical techniques available for surgical repair of nasal septal perforations (NSPs), but the evidence shows that no single technique is recognized as being consistently reliable. The inferior turbinate flap (ITF) for repair of NSPs of moderate size is a relatively simple technique that offers a success rate comparable to most techniques. The key advantages of the ITF include abundant vascularity, wide arc of rotation, possibility to use a combined skeletal and epithelial support, and ease of harvesting and insertion. Even more, any endoscopic surgeon can master the technique, and it can be one more substitute solution to a difficult problem.
11.1 Indications
Medium (1–2 cm) and/or large (> 2 cm) size NSPs
NSP without osteocartilaginous support
Rescue flap for NSP
11.2 Contraindications
In any patient who has undergone sphenopalatine artery or anterior ethmoidal artery ligation on the ipsilateral side.
Previous inferior turbinectomy or inferior turbinate (IT) surgery may reduce the flap’s pliability, limit its ability to mold to the shape of the defect, and may also compromise its blood supply.
11.3 Anatomy
The IT bone develops from a cartilage ossification center during the fifth intrauterine month. At the core of the IT is its central osseous layer of nonhomogeneous, cancellous, sponge-like bone made of interwoven bony trabeculae separated by a labyrinth of interconnecting spaces containing fatty tissue and blood vessels. The histology of the IT is comprises an epithelial mucosal layer overlying a basement membrane, an osseous layer, and an intervening lamina propria. The medial aspect of the mucosal layer is thicker and has more surface area than the lateral mucosa of the turbinate. 1
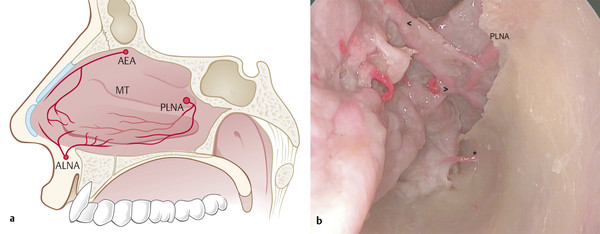
IT is vascularized by the posterolateral nasal artery (PLNA) (Fig. 11‑1). The PLNA descends vertically and slightly forward over the vertical apophysis of the palatine bone and enters the IT on the superior aspect of its lateral attachment between 1.0 and 1.5 cm from its posterior insertion. In 15% of cases the IT may receive supplementary irrigation from the palatine artery branches of the descending palatine artery. 2 Wu et al 3 studied the vascular anatomy of the IT in 11 cadavers. They observed that mean outer diameter of the PLNA is 1.10 ± 0.11 mm (range: 0.82–1.30); and it enters the IT on the superior aspect of its lateral attachment, 1.0 to 1.5 cm from its posterior tip; and divides in 2.50 ± 0.52 (range: 2–3) arteries as part of IT circulation. After the division the arteries enter a bony canal; one branch remains high and lateral while the other runs in a lower and more medial position. Both remain in bony canals or are closely applied to the bone for much of the length of the turbinate. The lower (medial) branch gives off branches that pierce the bone of the interior turbinate in its anterior part and form a regular pattern of alternating superior and inferior branches at right angles to the main artery. As the arteries run anteriorly, they increase in size, suggesting that there is a significant additional blood flow from anteriorly. These blood supplies are from an anastomosis with the anterior ethmoidal artery and the lateral nasal artery, which is a branch of the facial artery.
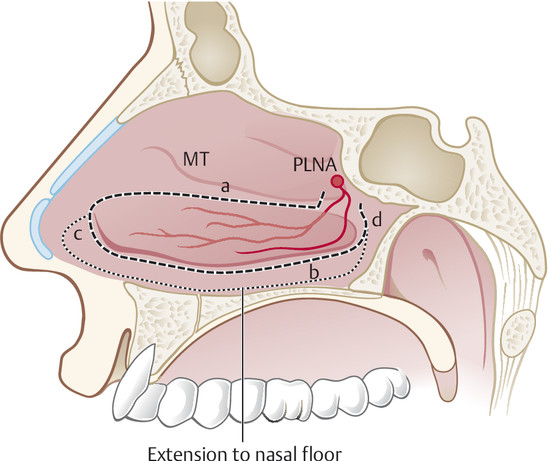
The ITF presents an excellent anteroposterior distance but lacks of a wide width. Gras-Cabrerizo et al 4 studied four cadaveric specimens and showed an anteroposterior distance range between 4.2 and 5 cm, with a width range between 1.2 and 1.4 cm. Amit et al 5 obtained similar results with a mean length and width of 4.8 and 1.8 cm, respectively, in 11 cadaver specimens. Harvey et al 6 obtained a similar length (5.4 cm), but with greater width (2.2 cm) extending its dissection to the inferior meatus and/or fossa floor.
11.4 Surgical Steps
11.4.1 Sinonasal Cavity Preparation
Cottonoids impregnated with a solution of 1:10,000 epinephrine are placed in the nasal cavity bilaterally during the surgical setup. At the beginning of surgery, the sites corresponding to the planned incisions are injected with lidocaine 1% with epinephrine 1:100,000. One must avoid injecting the area adjacent to the flap’s vascular pedicle (i.e., it causes vasospasm of the pedicle potentially impairing its viability) and the interior turbinate (i.e., it may be equivalent to an intravascular injection).
11.4.2 Posteriorly Based Inferior Turbinate Flap: Surgical Technique
The nasal cavity is decongested and prepared as previously described.
The IT can be gently medialized to better visualize its medial surface and the mucosa from the inferior meatus, and then subsequently laterally fractured to gain access to the lateral nasal wall.
An uncinectomy allows the identification of the natural ostium of the maxillary sinus and the posterior portion of the IT. In some cases enlargement of the maxillary sinus ostium posteriorly allows a better exposure of the PLNA and eases the preservation of the pedicle (Fig. 11‑2).
Elevate the mucosa from the anterior aspect of the ascending process of the palatine bone in a submucoperiosteal plane and proceed posteriorly to identify the crista ethmoidalis, sphenopalatine foramen, and sphenopalatine artery and its terminal branches. The sphenopalatine foramen is identified superior to the posterior IT, posterior to the basal lamellae of the middle turbinate. The pedicle blood supply to the IT can sometimes be visualized as pulsating. There is significant anatomical variation of the sphenopalatine artery branches and, accordingly, the sphenopalatine foramen or foramina. In fact, the PLNA may extend anterior to the posterior wall of the maxillary antrum. 7 , 8 Recognizing this anatomic variation during the maxillary antrostomy and mucoperiosteal elevation is vital to avoiding injury to the vascular pedicle.
Define the superior and inferior limits of the flap.
Make a posterior to anterior incision along the superior sagittal plane of the IT (superior incision).
Then make an inferior sagittal incision along the inferior meatus (inferior incision); in some cases one can extend the flap to the inferior meatus and nasal floor.
A vertical incision at the head of the IT then connects the two incisions (anterior incision). This incision is in S-shape, starting from the superior incision and sloping around the contour of the head of the IT and onto the inferior meatus. Care should be taken to avoid disrupting the valve of Hasner.
Use a periosteal elevator (freer dissector or Cottle elevator) to raise the mucoperiosteum off the IT from anterior to posterior both medial and lateral to the IT bone. The donor site is left open and allowed to heal, which is frequently the case after partial turbinectomy.
After harvesting the flap, margins of the perforation are easily elevated and/or rimmed with a 12-blade or a phaco blade. The two mucosal layers surrounding the perforation edges are separated from each other at least 3 to 4 mm in width circumferentially.
Finally the edges are sutured with absorbable suture (i.e., 2–0 Vicryl). Usually anterior, middle, and posterior sutures are placed to achieve complete closure. Sometimes the posterior sutures are difficult to place and they are reserve for the second surgery when the pedicle is detached from the lateral wall.
Second stage: After 6 weeks to 6 months, the pedicle is detached from the lateral nasal wall; bipolar cautery is used for hemostasis. The pedicle is transacted and the excess pedicle is discarded. At 3 weeks after surgery, the contralateral side of the flap has usually reepithelialized. Patients are instructed to keep the sides moist with nasal saline spray during the 3-week period.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree