1. Applied Anatomy for Safety in Facelifting
1.1 Introduction
Safety is paramount to achieving excellent results in rhytidectomy. Safety depends on the surgeon having a comprehensive knowledge of the anatomy of the face and neck in three dimensions. The fundamental goal in rhytidectomy dissection is to adequately release and mobilize the tissues the surgeon wishes to reposition and, in the process, preserve all vital structures. A prerequisite for accomplishing this safe release is a commanding knowledge of facial anatomy with respect to the key points of retention and their relationship to all vital structures. The first principle of anatomy in facelifting is that facial soft tissues are arranged in a series of concentric layers. This layered approach not only provides an excellent system for understanding and organizing facial anatomy, but also constitutes the practical method for performing a lamellar superficial musculoaponeurotic system (SMAS) facelift. A lamellar dissection offers the advantage that both skin and SMAS can be treated individually, which allows the excursion, vector, and tension of each layer to be adjusted differently, resulting in a natural, comprehensive rejuvenation while minimizing secondary deformities.
This chapter focuses on the step-by-step relevant anatomy the surgeon confronts while performing a high-SMAS lamellar dissection; all the information discussed here is essential knowledge for the surgeon planning to perform any type of facelift technique.
1.2 Anatomical Considerations in Skin-Flap Dissection
Although the general thickness of subcutaneous tissue varies from person to person based on age and weight, there is a proper thickness for skin-flap undermining, especially when performing a lamellar dissection. When beginning skin-flap undermining in the cheek, the flap must be relatively thin so as to avoid including SMAS fibers in the skin flap, which will render the SMAS flap too thin and therefore useless. If dissection is in the proper plane, the fat on the undersurface of the flap will have a rough, “cobblestone” appearance to it, which is more visible when the flap is transilluminated (Fig. 1.1). When the dissection is too deep, the undersurface will look smooth and contain streaks of fine white tissue; when it is transilluminated, this flap will appear thicker and “cloudy.” When beginning skin-flap undermining in the postauricular area, it is important to understand that, superiorly and anteriorly, there is little subcutaneous fat between skin and fascia, which makes it difficult to establish the correct subcutaneous plane. Beginning the dissection more posterior and inferior, the surgeon will encounter more subcutaneous fat and establish the correct plane more easily, facilitating dissection of the postauricular flap and lateral neck. Unlike the cheek-skin flap, which should remain thin, the neck flap should be slightly thicker to help avoid an, overresected appearance in the neck. 1

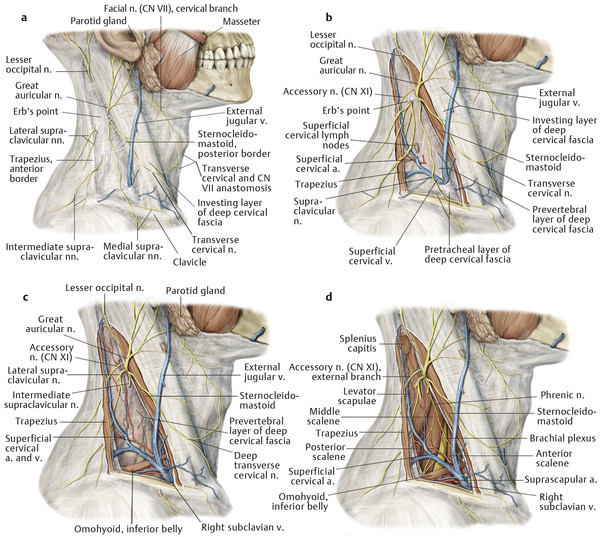
1.2.1 Great Auricular Nerve
As skin undermining progresses to the upper lateral neck, care must be taken to preserve the great auricular nerve (Fig. 1.2). This sensory nerve is derived from the cervical plexus and provides sensation to the earlobe and lateral cheek. The great auricular nerve runs obliquely from the posterior belly of the sternocleidomastoid muscle to the earlobe. The classic external landmark for locating the nerve is at the midbelly of the sternocleidomastoid muscle, 6.5 cm inferior to the bony external auditory canal. 2 The most common area of injury to the nerve is where the nerve emerges from around the posterior border of the sternocleidomastoid muscle at the most peripheral aspect of the subcutaneous undermining. The key to preventing injury is to stay within the subcutaneous plane and not violate the superficial cervical fascia (an extension of the SMAS and platysma), which overlies the sternocleidomastoid muscle. Staying superficial to this fascia over the muscle and not exposing muscle fibers enables preservation of the nerve. In most cases, the nerve lies deep to the plane of skin-flap dissection and is not seen; however, in very thin faces or secondary facelifts, where little subcutaneous fat may be present, the nerve is at greater risk and extra caution is therefore advised.
1.2.2 Retaining Ligaments
Proper skin-flap redraping requires a thorough knowledge of the retaining ligaments of the face (Fig. 1.3). These ligaments are vertically oriented fibers that penetrate the concentric horizontal layers of the face and function in a supportive role. 3 , 4 First described by Furnas, there are two types of retaining ligaments: (1) true osteocutaneous ligaments that run from the periosteum to the dermis and are made up of the zygomatic and mandibular ligaments and (2) retaining ligaments formed by a coalescence of superficial and deep facial fascia that form fibrous connections and vertically span from deep structures, such as the parotid gland and masseter muscle, to the overlying dermis; examples include parotid and masseteric cutaneous ligaments. The parotid cutaneous ligaments span the entire surface of the parotid gland, and the masseteric cutaneous ligaments are a series of fibrous bands found along the entire anterior border of the masseter muscle, starting in the malar region and extending down to the mandibular border.
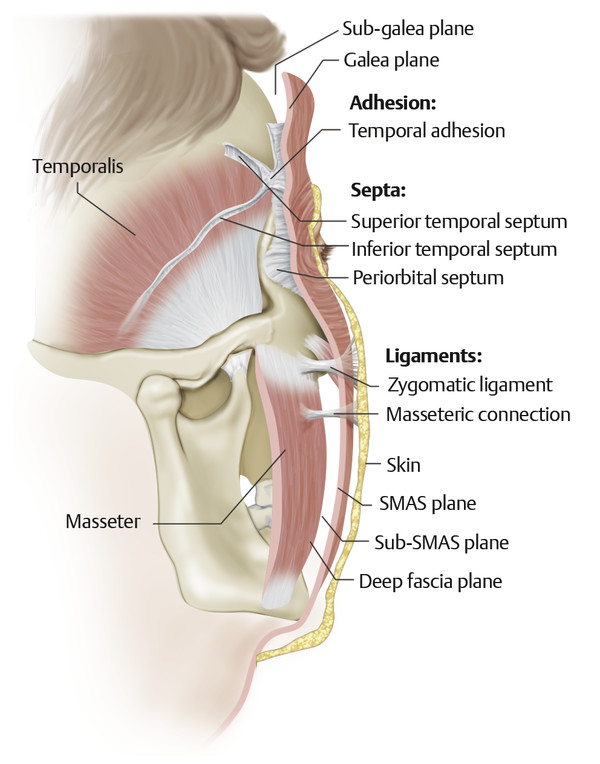
Based on this understanding of the retaining ligament anatomy in the face, the plan for skin-flap elevation and ligament release is shown here (Fig. 1.4). As skin-flap elevation progresses over the cheek, one first encounters fibrous, dense attachments over the parotid gland, where the dissection will be more difficult; these attachments represent the parotid cutaneous ligaments that must be released. Anterior to the parotid and inferior to the zygoma, once these ligaments are released, the dissection can proceed more easily. Superiorly, as the dissection approaches the malar eminence, one encounters the zygomatic ligaments. These stout bands of ligament attach the malar pad to the underlying malar eminence and must be released for proper skin-flap redraping; however, skin undermining does not arbitrarily include the entire face. In the performance of a lamellar SMAS flap, preserving the platysma cutaneous attachments in the perioral cheek and jowl area allows this tissue to be better elevated and supported via SMAS-flap elevation (Fig. 1.5). This area of connection between skin and SMAS also preserves important perforating vessels to the cheek flap, thereby reducing the likelihood of flap compromise. 5
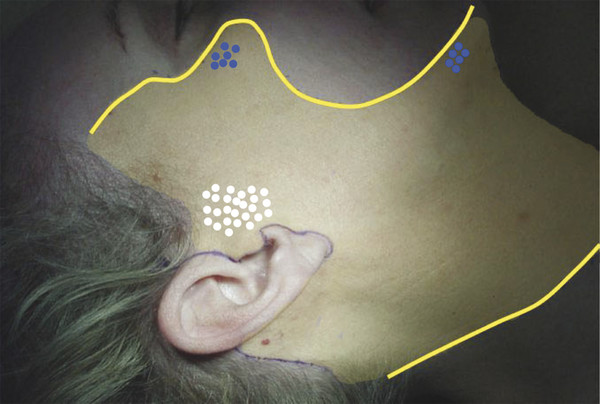
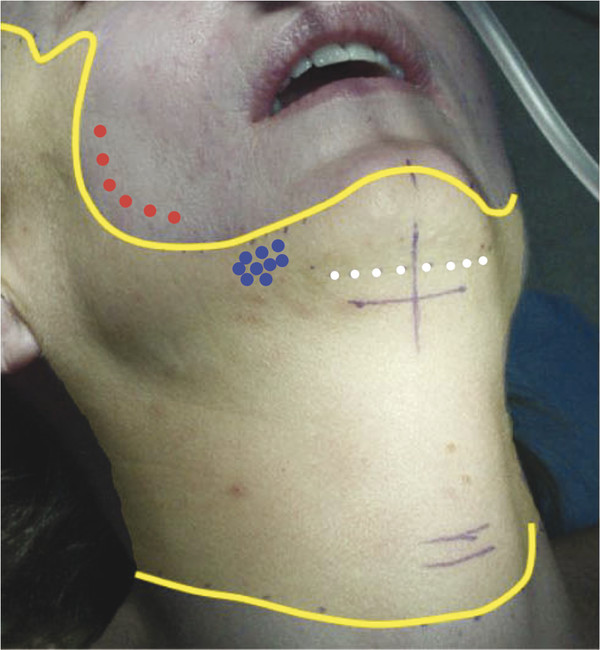
Complete skin-flap elevation in the neck combines wide undermining from both the lateral approach and the submental incision. Proper skin redraping and smooth contour of the chin and jawline require release of the submental crease and mandibular ligaments (Fig. 1.5). The mandibular ligaments are discrete fibrous bands that attach the parasymphyseal dermis to the mandible. Although some bleeding is usually encountered in completion of this step, it is not so great as to prevent release of these ligaments. If skin undermining has been carried out appropriately, at its completion, the skin redrapes smoothly and without tension as a result of the release of retaining ligaments where necessary, while preserving the important structures, including the great auricular nerve and the deeper SMAS layer, so that it can subsequently be released and repositioned for optimal rejuvenation.
1.3 Anatomical Considerations in SMAS-Flap Elevation
Unlike skin, the SMAS is an inelastic layer that is capable of providing sustained support for sagging deep-layer tissues. This is the fundamental reason why a lamellar dissection is performed and why the SMAS layer must be separately released and repositioned. As in skin-flap elevation, the basic goal of SMAS-flap elevation is adequate release of the flap to obtain the desired effect while preserving vital anatomical structures, which requires a precise knowledge of the relationship of the SMAS layer to the retaining ligaments already discussed and to the deeper facial layers and vital structures, such as the facial nerve and parotid duct.
The SMAS represents the superficial fascia of the face and forms a continuous layer throughout the face and neck. The SMAS is contiguous with the superficial cervical fascia inferiorly in the neck. Superiorly past the zygomatic arch, it becomes the temporoparietal fascia in the temple and then the galea in the scalp. 6 The SMAS layer varies in thickness from one area of the face to another. It is dense and thick over the parotid gland, and it is this portion that is most commonly understood by surgeons as clinically representing the SMAS. As the SMAS is traced medially, it is thinner and less distinct over the masseter and buccal fat pad. In the malar region, the SMAS is also thin and ultimately blends into the epimysium of the upper lip elevators. The layer deep to the SMAS is the parotid–masseteric fascia (deep facial fascia). This layer in the cheek is made up of the parotid capsule over the parotid gland and continues anteriorly to form the fascial layer over the masseter muscle. The significance of this layer is that branches of the facial nerve always lie deep to this layer in the cheek. Recognizing the importance of this point and being able to identify this layer allow safe, extensive mobilization of the SMAS superficial to it.
1.3.1 Facial Nerve
The facial nerve emerges through the stylomastoid foramen and is immediately protected by the parotid gland. Within the parotid, it divides into an upper and lower trunk and then into its five major branches: temporal, zygomatic, buccal, marginal mandibular, and cervical (Fig. 1.6). The branches leave the parotid gland lying on the surface of the masseter immediately deep to the parotid–masseteric fascia. Medial to the masseter, the nerve branches lie on the buccal fat pad, at the same depth as the parotid duct and facial vessels. The nerve branches then proceed to innervate the mimetic muscles on their deep surface (except for the deep layer of muscles: the mentalis, levator anguli oris, and buccinator). This point is important because during elevation of a SMAS flap in the region of the malar eminence, the zygomaticus major and minor muscles are frequently encountered. When these landmarks are seen, the surgeon should maintain the dissection superficial to these muscles. This location is safe for dissection because it ensures protection of the nerve branches.
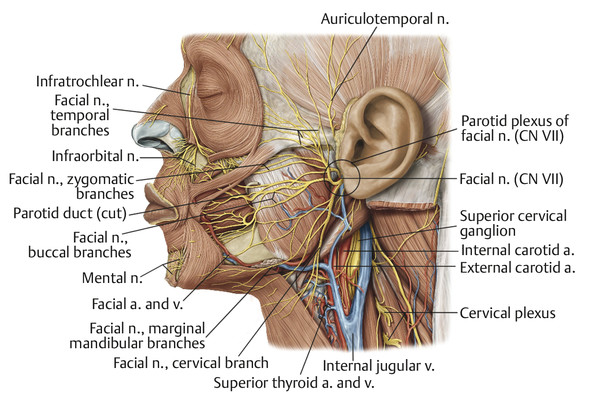
The facial nerve branches of greatest concern during a facelift are the temporal and marginal mandibular branches. Because the zygomatic and buccal branches have multiple interconnections and cross over, injury to these branches is not likely to cause a clinically noticeable deficit; however, this is not the case for the teporal and marginal mandibular branches. The frontal branch or collection of branches can be considered to travel along a line connecting the base of the tragus to a point 1.5 cm above the lateral eyebrow. 7 Another useful landmark is the point at which all temporal branches will cross the upper border of the zygomatic arch from 0.8 to 3.5 cm from the external acoustic meatus or tragus. 8 Unlike all other branches, which always lie deep to the deep facial fascia, the temporal branch penetrates the deep fascia just above the zygomatic arch and travels in the temporal region on the underside of the temporoparietal fascia. Thus, unlike SMAS elevation, which is always safe superficial to the parotid–masseteric fascia, elevation of the temporoparietal fascia across the location where the temporal branch traverses the deep fascia will result in temporal branch division. A SMAS flap can be elevated “high” at the upper border of the zygomatic arch, however, because the temporal branch is still deep to the SMAS at this level. 9 , 10 Because of this complex anatomy, any surgeon performing a facelift or temple lift must have a detailed, three-dimensional knowledge of the temporal branch to prevent injury.
The marginal mandibular branch exits the parotid approximately 4 cm beneath the base of the earlobe, near the angle of the mandible. In most cases, it courses above the inferior border of the mandible, and in all cases where it is anterior to the point where the facial vessels cross the mandibular border, it courses above the inferior border of the mandible. In 19% of cases, it lies up to 2 cm below the mandibular border posterior to the facial vessels. 11 In these cases, the nerve travels superiorly and will cross over the facial vessels as it continues above the level of the mandibular border. These vessels are palpable at the anterior border of the masseter and serve as a useful landmark for locating the marginal mandibular branch. This location is also likely to be where the nerve is at greatest risk for injury because the covering platysma and superficial fascia are thinner and the nerve is more superficial crossing over the facial vessels. In general, any subplatysmal dissection should proceed cautiously over the region of the angle of the mandible to prevent marginal mandibular branch injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree