The Postoperative Period and Management of Complications
Introduction
Postoperative care for the patient undergoing autologous fat transfer is relatively straightforward. However, managing patient expectations postoperatively may be more involved. In contrast to the postoperative facelift patient who perceives that the contour of the jawline is now relatively straight and the neck similarly elevated, the patient after a fat transfer must continue to observe ongoing evolution of change even up to a year after the procedure. What may be interpreted as dissipation of fat over time must be reinterpreted clearly for the patient as the slow ebbing of edema.
Management of postoperative complications can also be quite different from what the surgeon who typically only performs lifting procedures is accustomed to encounter and treat. A systematic identification of the problem and related treatment must be undertaken to ensure adequate correction and resolution. Specific problems such as lumps, bulges, malar edema, overcorrection, and undercorrection will be reviewed, each having a specific approach for treatment, as opposed to more universal, postsurgical problems such as infection, hematoma, and nerve injury.
The Postoperative Period
Postoperative Care
Unlike traditional lifting procedures that may enlist the use of drains and compressive dressings, fat transfer does not require any such supportive devices. As no true incision is made, there are no sutures to care for or to remove from the body or face. Accordingly, no specific skin cleansing regimen or topical ointment is required. Patients are discharged with instructions to ice their recipient sites liberally for the first 48 to 72 hours postoperatively and to maintain a semi-inclined posture at night for the first week to minimize edema. Beyond the initial postoperative period, patients may note fluctuation in their swelling that may be worse when they wake up or after increased activity. Icing of the swollen area can help to counteract the edema, accelerating the return to baseline. It is not unusual for patients to find that icing for up to 2 weeks will ameliorate the edema and alleviate a common flushed sensation. Besides these simple instructions, the patient need not perform much else by way of postoperative care (Fig. 4-1).
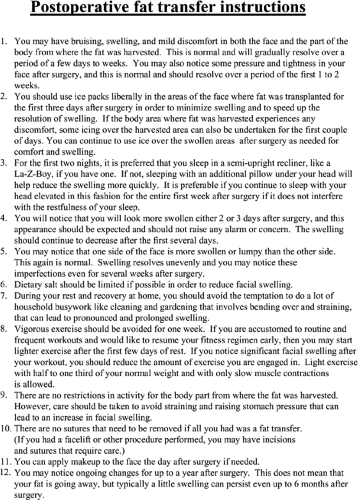 Figure 4-1: Postoperative instruction sheet given to patients to detail what they should know and expect regarding their convalescence. |
Restrictive activity can help to expedite resolution of edema. More specifically, patients are instructed not to engage in household busywork like gardening and cleaning. These activities require frequent bending over and straining that can lead to additional edema and delay recovery. Ideally, vigorous exercise should be modified to facilitate dissipation of edema. Patients who normally pursue a serious workout regimen will experience some degree of psychological deflation arising from a protracted abstinence from physical fitness. Accordingly, early return to light exercise may help to invigorate the patient’s spirits and thereby aid in recovery. Although no activity restriction needs to be made to the donor site from where the fat was harvested, raising intra-abdominal pressure can lead to increased and prolonged facial edema and should be avoided. Light, isometric weight lifting, in sitting and standing positions only, that involves about a third to half of the normal weight routinely lifted can be undertaken with slow muscle contraction without any harm. More vigorous walking is encouraged within a few days of surgery. Dietary salt restriction can also prove beneficial for minimizing postoperative facial edema.
Although infection is rare, we routinely prescribe perioperative antibiotics, such as cephalexin, that target skin flora to further minimize that likelihood. Narcotic pain medication is prescribed yet is frequently unnecessary, with patients usually relying on acetaminophen or no pain medicine at all. Following fat transfer, the face typically does not elicit any significant discomfort. In the facial recipient sites, patients commonly describe having a sensation of skin tightness or pressure, facial flushing, and/or mild periorbital soreness, all of which are normal in the postoperative period. At the donor site, patients frequently describe tenderness with a dull ache that resolves over a period of a few days.
As no bandages need to be changed or sutures removed, postoperative visits are made mostly to follow the clinical progress and to manage the patient’s postoperative expectations. For the surgeon just starting out in autologous fat transfer, frequent patient visits should be the norm so that the surgeon can begin to appreciate the nature of the postoperative course that results from his or her handiwork. For instance, the patient can be seen the following day after surgery, then a week after the procedure, and every week thereafter until most bruising and swelling resolve. For the more experienced fat transfer surgeon, a customized postoperative plan can be executed based on the patient’s level of anxiety or need for care. A patient who is fretful about the appearance of swelling can be seen every week for reassurance, whereas a less anxious patient who is comfortable with the recovery process can be asked to follow up 1 week after surgery and then 4 to 6 weeks thereafter.
Postoperative Course
Guiding the patient through the projected postoperative course before surgery is helpful in establishing realistic recovery times and thereby permits the patient to schedule time off from work and away from important social events. Variability in healing should always be emphasized before surgery and as the patient heals afterwards. However, as a guideline, most patients require a full 2 weeks off from work to look “socially acceptable.” Helping an individual to understand what he or she will look like immediately after surgery and in the ensuing months will relieve anxiety and dispel misconceptions.
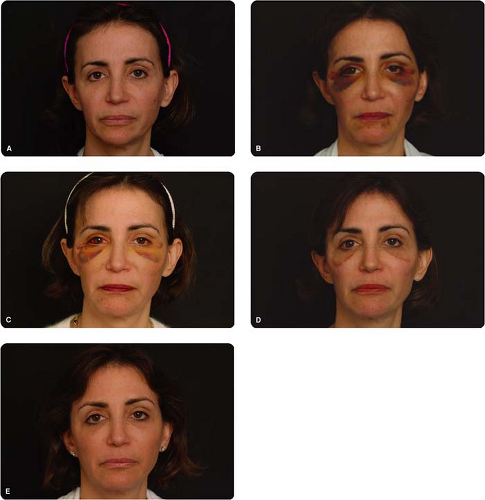
In the immediate postoperative period, the patient will exhibit a variable degree of ecchymosis and edema based proportionately on the volume of fat transferred. The greatest amount of ecchymosis and edema occurs from addressing the inferior orbital rim (Fig. 4-2). Performing concurrent ancillary procedures, such as face and browlifting, will generally worsen the degree of ecchymosis and edema due to increased operative time and surgical manipulation. Ecchymosis typically lasts for 2 weeks, but a lesser degree of periorbital ecchymosis at times can endure for even 1 to 2 weeks longer and may be difficult to camouflage completely. Patients should understand that recovery is variable and that 2 weeks may be insufficient to arrive at a point where the patient perceives he or she is socially acceptable. Informing a patient that recovery may exceed several weeks, however, may make undergoing a fat transfer less tenable, as most working individuals cannot afford that much time off from work. Judicious, albeit realistic, preoperative counseling is important in every case.
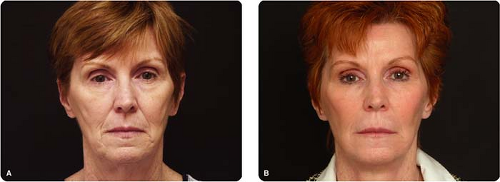
A patient at 2 weeks after surgery will still be swollen and may not feel socially acceptable. However, most onlookers, even those who are familiar with the patient, will often not perceive this deformity and will simply look at the patient as appearing more refreshed and rejuvenated. It is helpful to have the patient look at a photograph of another patient at 2 weeks postsurgery (Fig. 4-3). Most patients will find this result acceptable, but the surgeon can admonish that the photographed patient still did not like the way he or she looked at that time. The distinction between how patients view themselves and how others view them is important to emphasize. If the patient is very happy with the way he or she looks after the second postoperative week, adoration of the result at this early a phase can actually be problematic, as much of the volume present is still edema. Counseling the patient with regard to this is important for establishing realistic expectations down the road. Fortunately, if additional volume is needed,
another surgery can be easily performed to enhance the result. Conversely, taking away too much volume is much more difficult. For this reason, we routinely counsel all patients that touch up procedures are often necessary.
another surgery can be easily performed to enhance the result. Conversely, taking away too much volume is much more difficult. For this reason, we routinely counsel all patients that touch up procedures are often necessary.
Although swelling will persist for months, patients often are happy with their appearance by the fourth week. Patients should be advised about the continued resolution of edema so as not to mistake these changes as a sign of fat dissipation. Typically, most edema has resolved by the sixth postoperative month, and the volume that persists thereafter is relatively permanent. This brings up another common patient query
as to the longevity of the result. It is helpful to inform the patient that of the transferred adipocytes, some will survive and some will resorb. There is no exact percentage that can be quoted, and there are variables that can affect the survival, such as a history of smoking. If a patient gains significant weight, that weight will be noticeably evident in the face, as the transplanted fat cells hypertrophy. Even though some of the transplanted fat appears to be permanent, ongoing chronologic aging that will subtract volume over time will continue to erode the result. Based on the patient’s aging process, results will have variable longevity and will require additional sessions as indicated. Significant weight change can also affect the long-term result. Patients who have a marked weight loss following surgery are likely to notice diminished volume in their face.
as to the longevity of the result. It is helpful to inform the patient that of the transferred adipocytes, some will survive and some will resorb. There is no exact percentage that can be quoted, and there are variables that can affect the survival, such as a history of smoking. If a patient gains significant weight, that weight will be noticeably evident in the face, as the transplanted fat cells hypertrophy. Even though some of the transplanted fat appears to be permanent, ongoing chronologic aging that will subtract volume over time will continue to erode the result. Based on the patient’s aging process, results will have variable longevity and will require additional sessions as indicated. Significant weight change can also affect the long-term result. Patients who have a marked weight loss following surgery are likely to notice diminished volume in their face.
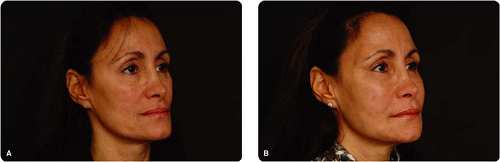
What we have noticed in many patients undergoing fat transfer is that some additional volume may be observed after a year. This curious phenomenon lacks a definitive explanation but has been commonly seen by our patients. In addition to this late change, we have noticed a change in skin tone and texture after the first year, during which time rhytids and uneven skin texture may improve (Fig. 4-4).
Management of Complications
Although many types of complications can theoretically arise after fat transfer, this section will address only the commonly encountered problems and how to correct them. Using a blunt infiltration cannula significantly reduces the likelihood of a sensory or motor nerve injury. In our practice, we have yet to encounter a temporary or permanent paralysis. Management of this problem is expectant, and a discourse on treatment of a permanent paralysis lies beyond the scope of this text. The use of blunt cannulas, as well as the practice of not forcing a cannula when meeting significant resistance, will also reduce the likelihood of vascular injury. Development of a hematoma is exceedingly rare, especially if these principles are followed. In our practice, we have seen one hematoma that resolved with aspiration. Arterial embolism with consequent skin necrosis has been reported but is an extremely rare condition. Treatment of this condition is limited and expectant. Discussion of adjuvant therapy and local wound care will not be entertained herein and would detract from the clarity and simplicity of the proposed management protocol.
Most surgeons who are adept at managing problems associated with lifting procedures (e.g., facelift, browlift, etc.) will need to learn a new set of tools to address the unique complications that arise after fat transfer. Although complications can occur anywhere in the face, the most common area for a problem after fat grafting is the periorbital region, where contour deformities are more readily apparent and more difficult to manage. Most of the following discussion will be centered on the treatment of periorbital complications but can be easily extrapolated to other areas of the face that experience similar complications.
Identification of the Complication
Identification of the problem at hand is primary. We have divided the types of common complications that can be encountered as follows: contour irregularities (further divided into the categories of lumps or bulges), persistent malar edema, overcorrection, undercorrection, and divoting at the cannula entry site (Table 4-1). This section will principally discuss the nature of each complication and briefly introduce the appropriate management. Detailed treatment protocols have been reserved for the subsequent section.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree