Rehabilitation, Outcomes and Assessment
Static Versus Dynamic Splinting for Proximal Interphalangeal Joint Pyrocarbon Implant Arthroplasty: A Comparison of Current and Historical Cohorts
Riggs JM, Lyden AK, Chung KC, et al (Univ of Michigan Health System, Ann Arbor; Univ of Michigan, Ann Arbor; Univ of Michigan Med School, Ann Arbor) J Hand Ther 24:231-239, 2011§
Evidence Ranking
• B
Expert Rating
• 2
Abstract
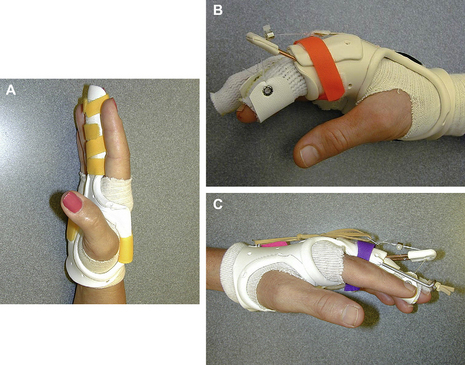
Study Design
Nonrandomized mixed current and historical cohort follow-up study. The purpose of the study was to test the effectiveness of static splinting after arthroplasty in patients with osteoarthritis. Dynamic splinting is recommended after proximal interphalangeal joint pyrocarbon implant arthroplasty; however, static splinting may be more feasible to deliver. Nine consecutive patients received static splinting in this study. These patients were compared with those of a historical control group (n = 10) who received dynamic splinting. Function and performance variables were measured preoperatively and 3 months after surgery. All patients underwent surgery by the same hand surgeon, and most of the patients were treated by the same certified hand therapist. Both static and dynamic groups showed improvement on several function and performance measures. Compared with the dynamic group, the static group showed greater improvements in the Michigan. Hand Outcomes Questionnaire subset of work performance (21.00 ± 14.75 vs 3.13 ± 14.13, p < 0.05) and Jebsen-Taylor Test (−11.58 ± 5.44 vs −2.81 ± 3.23, p < 0.03). Patients who received static splinting had similar outcomes to those who received the dynamic splinting. Static splinting requires less therapist training and offers greater patient convenience and is a promising protocol that should be evaluated in a larger study (Fig 1, Table 2).