14
Urticaria and Angioedema
• Urticaria (hives) is characterized by wheals: evanescent, pale to pink-red, edematous papules or plaques (Fig. 14.1); lesions often have central clearing, a peripheral erythematous flare, and associated pruritus.



Fig. 14.1 Wheals. Wheals can be small or large in size (A) as well as annular or polycyclic (B), but they still retain the classic central pallor and erythematous flare. C Occasionally, more uniform edematous plaques are seen. B, Courtesy, Julie V. Schaffer, MD.
• Individual wheals last <24 hours, which can be documented by outlining them with ink.
• Angioedema represents deeper dermal and subcutaneous or submucosal swelling (Fig. 14.2); affected areas are ill-defined, have minimal or no overlying erythema, and may be painful as well as pruritic.
• A classification scheme and DDx for urticaria and angioedema are presented in Table 14.1; patients with angioedema may have associated urticaria, including physical urticaria.
Table 14.1
Classification and differential diagnosis of urticaria and angioedema.
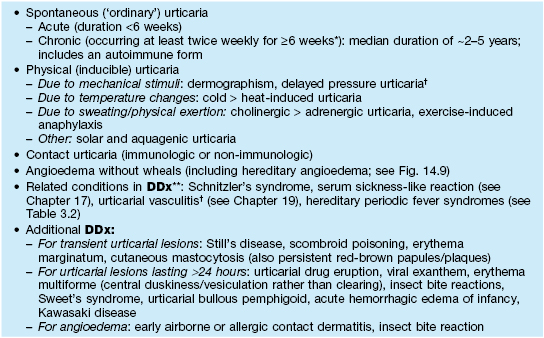
* Urticaria occurring less frequently than this over a long period is referred to as episodic or recurrent.
† Individual lesions tend to last >24 hours; urticarial vasculitis features burning/pain, purpura upon resolution, and a subgroup associated with hypocomplementation and autoimmune connective tissue disease (e.g. SLE).
** Consider for chronic urticaria with associated symptoms such as fevers, pain, and arthralgias.
SLE, systemic lupus erythematosus.
• Stimuli for mast cell degranulation are shown in Fig. 14.3.
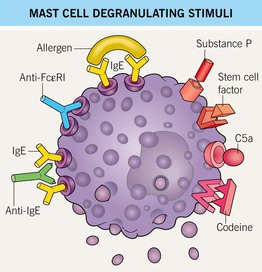
Fig. 14.3 Mast cell degranulating stimuli. Both immunologic and non-immunologic stimuli can lead to release of mediators. Stem cell factor is also known as KIT ligand. Autoantibodies against the high-affinity IgE receptor (FcεRI) and the Fc portion of IgE are implicated in chronic autoimmune urticaria.










