CHAPTER 36 Triple Arthrodesis
OVERVIEW AND APPROACH
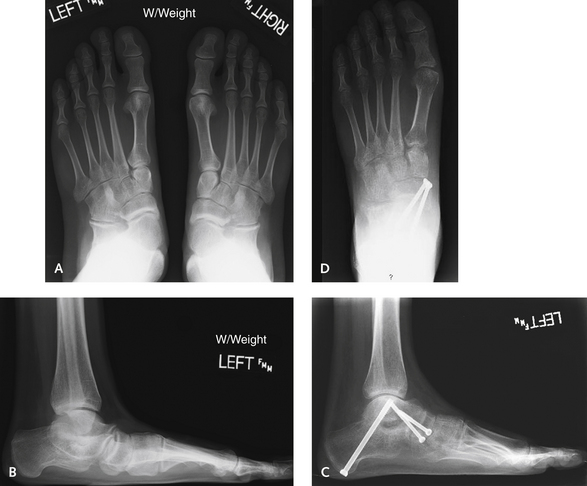
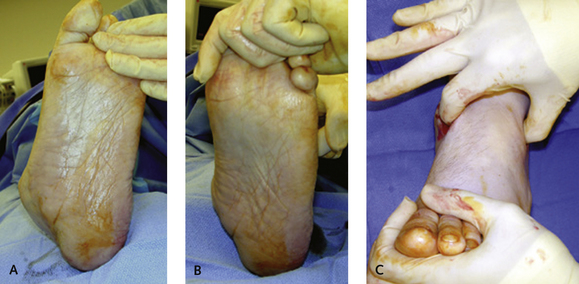
Posttraumatic arthritis generally follows a talus or calcaneus fracture, but for most patients with arthritis and deformity secondary to a calcaneus fracture, a subtalar rather than a triple arthrodesis is the procedure of choice. A triple arthrodesis usually is the preferred procedure after a talar neck fracture with malunion, particularly when a varus malunion associated with arthritis is present (Figure 36-1). In the presence of a middle facet tarsal coalition, a subtalar arthrodesis is sufficient, and a triple arthrodesis is preferred only in the setting of arthritis or deformity, which typically is associated with a naviculocuneiform coalition, and when the coalition is not resectable. In patients with inflammatory arthritis, caution is indicated in selecting an isolated TN fusion, even when this is the only involved hindfoot joint. An isolated TN arthrodesis is associated with a higher incidence of nonunion, and once this occurs, correction is far more difficult because of bone loss and erosion, even with a triple arthrodesis.
SURGICAL APPROACHES
Over the years, I have been performing more hindfoot arthrodesis procedures through a single medial incision. Initially, I identified correction of a severe fixed valgus deformity as the specific indication for use of this approach, to limit the risk of lateral wound complications occurring as the hindfoot position is corrected to neutral (when using a lateral incision). This rationale still holds; nevertheless, I have been very pleased with the ability to correct deformity and associated arthritis from a single medial incision. Although the medial approach to triple arthrodesis is discussed in more detail further on, the concept of use of a single incision to perform a hindfoot correction is important. As might be expected, the inclusion of the CC joint in the fusion in performing a triple arthrodesis from the medial approach is difficult. In my own experience, both anatomic observations and outcomes in clinical series have demonstrated that the CC joint can be exposed and included in the arthrodesis with this approach. Nonetheless, as supported by results with my frequent use of the medial approach to correct deformity, it is apparent that the CC joint does not always need to be included in the arthrodesis (Figure 36-2). In performing the more limited arthrodesis (subtalar and talonavicular), however, it is important to recognize the potential for inferior subluxation of the cuboid relative to the calcaneus. This subluxation will produce a fixed rotation of the transverse tarsal joint, causing pain under the cuboid and the base of the fifth metatarsal. A good example of this potential problem is presented in Figure 36-3: After a limited arthrodesis performed using a medial approach, intraoperative fluoroscopy revealed that the CC joint was inferiorly subluxated, demonstrated by pushing up from below the cuboid to correct the subluxation, and could be corrected only by including the CC joint in the arthrodesis. There are probably fewer indications for a limited lateral arthrodesis, such as a subtalar and calcaneocuboid arthrodesis, but when the correction can be obtained, it is well worth trying to leave the talonavicular joint untouched.
The Lateral Incision
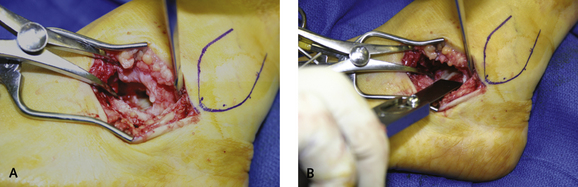
The incision is made from the tip of the fibular extending distally down over the sinus tarsi toward the CC joint (Figure 36-4). On the inferior surface of the incision, the peroneal tendon sheath is identified, and the terminal branch of the sural nerve must be looked for more distally in the incision. Both the peroneal tendons and the sural nerve are retracted inferiorly, and the incision can be deepened down on the periosteum directly over the calcaneus. The incision is extended distally toward the CC joint and then further toward the base of the fourth metatarsal. In the terminal aspect of the incision, care must be taken to ensure that no branches of either the sural or lateral cutaneous branch of the superficial peroneal nerve are present. The retinaculum of the undersurface of the peroneal tendon sheath is stripped and elevated off the lateral wall of the calcaneus. I prefer to save the contents of the sinus tarsi, because in the event of a wound dehiscence, sufficient tissue is always present for covering the peroneal tendons. The soft tissues are elevated sharply off the floor of the sinus tarsi until the anterior aspect of the posterior facet of the subtalar joint is visualized.
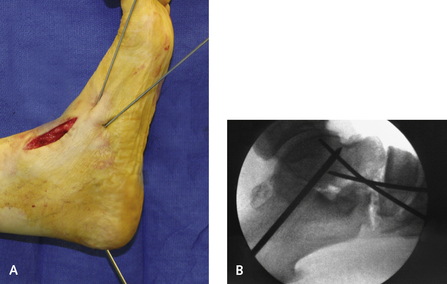
A laminar spreader is inserted into the sinus tarsi, and when it is placed on stretch, the interosseous ligament is easily visualized and cut to gain access to the posterior aspect of the subtalar joint and the middle facet. A 1-cm flexible chisel is used to denude the articular surface of the posterior facet. As with the CC joint, minimal bone is removed. The posterior facet must be debrided down to bleeding, healthy subchondral bone (Figure 36-5). Care is taken with the debridement of the posteromedial corner of the joint, where the flexor hallucis longus tendon is at risk for injury from the chisel. Finally, the more medial aspect of the subtalar joint and the middle facet must be completely denuded, including the undersurface of the talus and the dorsal surface of the middle facet. Before the medial incision is made, the space between the navicular and the cuboid is debrided with a rongeur. This debridement adds another segment and bone surface to the fusion mass and converts the triple arthrodesis to a “quadruple arthrodesis” (Figure 36-6).
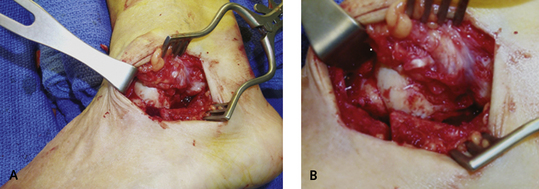
After the dissection, a retractor is inserted to pull aside the anterior tibial tendon and the medial soft tissues. The periosteum along the navicular bone is stripped, and then the TN joint is fully exposed with a curved periosteal elevator. Inserting an elevator directly into the joint to fully expose the head of the talus, followed by further stripping of the soft tissue dorsally and laterally, is useful. When a severe valgus deformity is corrected, pushing the midfoot into varus and then loosening the tension of the medial TN joint are helpful. I then cut around the medial joint from the outside in, through the remnant of the posterior tibial tendon and spring ligament into the TN joint. This step makes opening and distraction of the joint far easier. A smooth laminar spreader (Figure 36-7, A) or rongeur is inserted into the joint and then exchanged for a toothed laminar spreader to facilitate distraction of the joint. Another option to maximize visualization of the joint is to apply distraction using pins inserted through a laminar spreader through which distraction can be applied (see Figure 36-7, B). The entire joint is denuded of cartilage using a 1-cm flexible chisel. An important consideration with the navicular is that because this bone can be hard, it can fragment if not debrided gently. The same contour must be maintained with debridement of the talar head while a small flexible chisel is used. Presence of osteopenia increases the risk of injury with use of the laminar spreader, which may crush into the talus. At the completion of the joint debridement, surfaces should appose well, with maintenance of the overall joint contour. If bone is resected from either joint surface, the medial column of the foot will be shortened, followed by a varus malunion.
Reduction of Deformity and Fixation
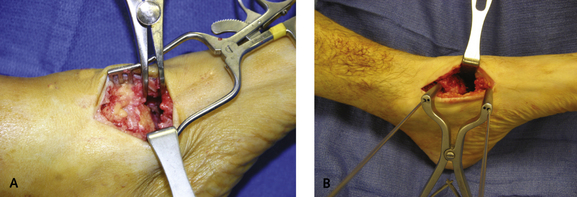
The reduction maneuver of the hindfoot relative to the forefoot is critical. For most deformities, the hinge point is the TN joint; therefore this is the joint that I reduce and fix first. The foot is rotated around the axis of the TN joint, and as the forefoot is adducted, the first metatarsal is plantar flexed to correct the forefoot relative to the hindfoot (Figure 36-8). This maneuver is unsuccessful only when the subtalar joint is rigid and the calcaneus is laterally translated, in which case I fix the subtalar joint first. In the latter instance, then the TN joint may not line up perfectly, although clinically the forefoot alignment may appear to be corrected. For some very severe deformities that feature gross posterior subluxation of the subtalar joint, it is helpful to address this problem first by inserting a laminar spreader between the anterior process of the calcaneus and the lateral process of the talus. This maneuver forces the calcaneus forward, reducing the subtalar subluxation.
In the past I routinely used cannulated screws for fixation of the arthrodesis of each of the joints, and for the most part I still prefer screws for fixation. I currently use one 7.0-mm cannulated screw for the subtalar joint and one or two 5.5-mm screws for the CC and TN joints. I have noted, however, that it is difficult to obtain good placement of screws across the TN joint. One screw is easy to insert from the plantar medial aspect of the navicular, but the available space is not always sufficient for a second screw, and even use of two screws inserted from the medial aspect of the joint does not provide adequate fixation of the dorsal joint surface (Figure 36-9). The fixation of the TN joint may then be quite inadequate, because the joint is compressed predominantly medially, which may be associated with a delayed union or even nonunion of the joint fusion (Figure 36-10). If I am not satisfied with the fixation in the TN joint after placement of one or more screws, I supplement this with a dorsal two-hole locking compression plate (Figure 36-11).
I generally begin with the TN joint fixation. One or two guide pins are inserted into the TN joint, the first from the inferior medial tuberosity, and the second from a slightly more dorsal location, immediately adjacent to the anterior tibial tendon. The head of the second, more dorsal screw will be close to the naviculocuneiform joint. The heads of all screws must be well buried flush with the margin of the bone and not protrude into the naviculocuneiform joint. As noted, this configuration of screw fixation will provide fixation and compression of the medial aspect of the talonavicular joint only. An alternative method of fixation is to use crossed screws, one from the medial navicular and the other introduced percutaneously from the dorsolateral aspect of the navicular just dorsal and medial to the cuboid (Figure 36-12).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree