Diagnosis
kV
Diameter (cm)
Dose (Gy)
Interval (days)
Actinic keratoses
12–20
<2
2–3 × 8
4–7
>2
5–7 × 4
3–4
Bowen’s disease
12–20
<2
3–4 × 8
3–4
>2
8–10 × 4
Lentigo maligna
12
>2
12 × 10
2–7
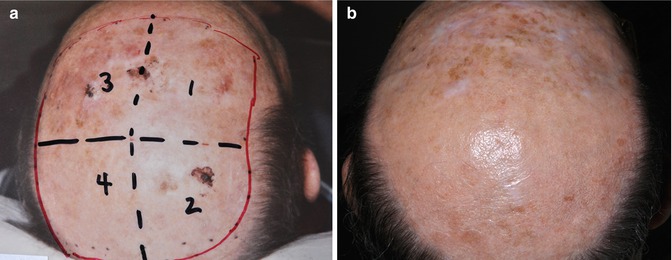
Fig. 8.1
(a) A 66-year-old patient with disseminated actinic keratoses on the scalp with four treatment fields (6 × 4 Gy, 12 kV, time interval 3–4 days). (b) Same patient 7 years after radiation treatment with durable remission
8.3 Bowen’s Disease
First described in 1912, Bowen’s disease (BD) is a form of intraepidermal squamous cell carcinoma (in situ SCC) [10]. In two thirds of patients, a solitary, sharply demarcated erythematous and scaly or crusted plaque ranging in size from a few millimeters to several centimeters can be found, mostly located on the head, neck, hands, and lower leg [11–13]. Often the pilosebaceous apparatus is involved [14]. Less common sites or variants include pigmented BD, subungual/periungual, palmar, genital, perianal, and verrucous BD. Its mucosal variant is called erythroplasia of Queyrat. A minority (<5 %) become invasive although this figure may be higher (10 %) in genital lesions (erythroplasia of Queyrat) [15]. Various radiotherapy techniques (soft X-rays, orthovoltage, or electron therapy) and regimens have been used to treat BD, but there are no studies directly comparing other treatments with RT, and data are sparse regarding dosing and toxicity. RT is advantageous in patients who refuse surgery, for lesions in cosmetically sensitive areas, for large and multiple lesions (Fig. 8.2a, b), and for patients with keloid formation [13]. Several retrospective studies indicate local control rates from 89 to 100 % (Table 8.2) despite wide ranges in doses used. Local recurrences seem to be equally low in patients treated with high- and low-dose regimens. Patients with grade 4 toxicities according to Cox et al. [16] (necrosis of cartilage/bone damage and/or ulceration with an additional requirement for a duration of >3 months) more often had hypofractionated regimens (dose per fraction >4 Gy) in an extremity location. In the study of 59 lower extremity BD lesions by Cox and Dyson [17], one fifth also failed to heal after RT. Dupree et al. [12] reported nonhealing ulcers in 25 % of patients with BD after a median of 27.5 months following RT, all of them on the lower extremity. Most patients with this side effect were treated with orthovoltage X-rays. Recent review articles on managing patients with BD emphasize the multitude of treatments for these patients [15, 18]. Despite this, RT remains an excellent and well-tolerated therapeutic option in selected patients with BD (in particular on digital, penile, or perianal sites), but risk factors for poor healing on the lower leg, such as poor vascularity, size of the lesion (>4 cm), and large fraction size (>4 Gy), should be taken into account [12, 13, 15]. When other treatments have failed, RT can be effective [19].
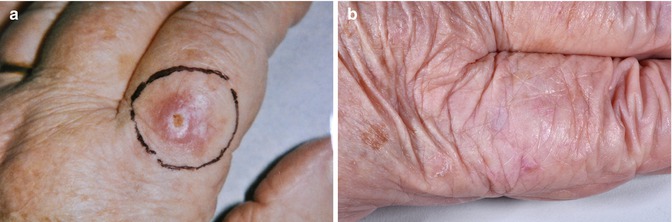
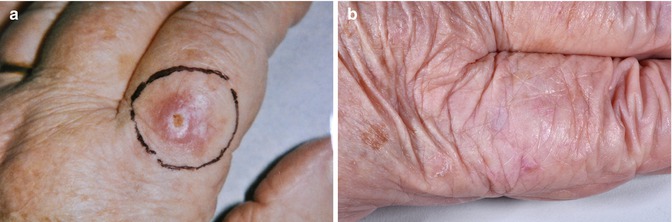
Fig. 8.2
(a) A 82-year-old patient with Bowen’s disease on her left index. (b) Same patient 5 years after radiation treatment (8 × 4 Gy, 20 kV, time interval 3–4 days)
Table 8.2
Summary of publications to treat Bowen’s disease with radiation therapy
Authors | Year | Number of lesions | Dose/fraction Gy | Total dose Gy | Local control (%) |
|---|---|---|---|---|---|
Schoefinius et al. [28] | 1974 | 33 | 2–5 | 40–60 | 100 |
Stevens et al. [29] | 1977 | 19 | 5 | 50 | 89 |
Panizzon [30] | 1983 | 41 | 4 | 40 | 100 |
Blank and Schnyder [31] | 1985 | 73 | 2–8 | 40–48 | 97 |
Cox and Dyson [17] | 1995 | 59 | 12–18 | 10–42 | 100 |
Caccialanza et al. [32] | 1999 | 62 | 2–5 | 40–70 | 98 |
Dupree et al. [12] | 2001 | 16 | 2.5–3.5 | 44.2–52.5 | 100 |
Lukas Vanderspek et al. [13] | 2005 | 42 | 3–15 | 10–52 | 100 |
8.4 Lentigo Maligna
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








