9 Pancreas transplantation
Introduction
Transplantation of the pancreas is the only treatment currently available that reliably offers insulin independence and normal glucose metabolism for patients with type I diabetes mellitus. Islet transplantation may ultimately supersede solid-organ pancreas transplantation in regularly providing insulin independence for diabetic patients. There are formidable obstacles before this can be achieved. Unless there is a significant breakthrough altering the pace of development in islet transplantation, solid-organ transplantation is here to stay for a number of decades rather than years.
The first pancreas transplant was performed in the University of Minnesota in 1966.1 Early experience with pancreatic transplantation was disappointing and this situation remained for many years. Difficulties were related to the management of the exocrine secretions and septic complications, a high incidence of thrombosis, acute rejection and pancreatitis. For the first 22 years of its 42-year history less than 1200 pancreas transplants were performed worldwide. Even after the introduction of ciclosporin in 1983, 1-year patient and graft survival rates were only 75% and 37% respectively. Understandably in the 1970s and 1980s enthusiasm for pancreas transplantation was scarce; the predominant sentiment was scepticism.
Indications for pancreas transplantation
Pancreas transplantation aims to provide patients who have type I diabetes with an alternative source of insulin. In 1998 Sasaki et al. reported a small number of patients with insulin-requiring type II diabetes who had received pancreas transplants with short-term success.2 The long-term outlook for such patients remains unknown.
There are a number of theoretical concerns in considering pancreatic transplantation for patients with type II diabetes.3 The pathogenesis of type II diabetes is fundamentally different from that of type I diabetes. Patients with type II diabetes have insulin resistance as part of their clinical syndrome and the influence of this on islet function in the long term after transplantation remains unclear. Furthermore, type II diabetes is much more prevalent than type I diabetes worldwide and carries a different, often much poorer, prognosis.4 The allocation of a scarce resource to such patients at the expense of those with type I diabetes clearly poses ethical difficulty.
Pancreas transplantation from living donors
The pancreas transplant database of all US transplants between 1988 and 2003 records 66 living-donor transplants out of approximately 15 000 pancreas transplants.5 The experience regarding perioperative morbidity and the long-term risks for the donor is inadequate to allow comment. The fact that it remains a fringe activity confined to very few centres presumably indicates that living-donor pancreas transplantation is not endorsed by the transplantation community in general. This is certainly the view that prevails in the UK and the rest of Europe. The discussion in this chapter is confined to allogeneic pancreas transplantation from deceased organ donors.
Patient selection for pancreas transplantation
Pancreas transplantation is performed in three distinct clinical settings, as presented below.
Simultaneous pancreas–kidney transplantation (SPK)
There is little debate that diabetic patients with renal failure should be offered kidney transplantation and there is good evidence that their prognosis is poor on dialysis.6 Such patients will already be obligated to immunosuppression on account of kidney transplantation. Combined kidney and pancreas transplantation offers these patients the opportunity to become insulin independent as well as dialysis independent. The risks and potential benefits of SPK transplantation compared with kidney transplantation alone for diabetic patients are summarised in Box 9.1. The evidence for the risks and benefits alluded to in Box 9.1 is reviewed in the final part of the chapter.
Box 9.1 Potential risks and benefits of simultaneous pancreas–kidney (SPK) transplantation
Risks
Perioperative morbidity and mortality
Potential for pancreas transplant to adversely affect kidney transplant outcome
Experience has taught us the crucial importance of recipient selection to the success of pancreas transplantation. Cardiovascular comorbidity is the most important factor leading to patient death in the early postoperative period after transplantation in diabetic patients. Patient selection needs to include a comprehensive medical evaluation, ideally performed by a multidisciplinary team within each transplant unit. Asymptomatic ischaemic heart disease is not uncommon in diabetics. Therefore, as a minimum the cardiac assessment should include a 12-lead echocardiography, exercise tolerance test and a non-invasive test of myocardial perfusion (a radioisotope scan or dobutamine stress echo). There is insufficient evidence to comment on the value of routine angiography.7 Any abnormality detected in non-invasive tests or those patients with symptoms of ischaemic heart disease should be investigated further, including angiography. Any correctable coronary artery disease should be dealt with prior to transplantation.8
Most pancreas transplant units will have an arbitrary and flexible upper age limit in determining suitability for SPK transplantation. With increasing experience, criteria for suitability of individuals for SPK transplantation have become more liberal. In the USA 19% and 15% of patients receiving SPK transplantation were aged 50 or older in 2004 and 2005 respectively.9
 Previous contraindications to transplantation have become relative contraindications or risk factors (Box 9.2).9
Previous contraindications to transplantation have become relative contraindications or risk factors (Box 9.2).9
Strong evidence to differentiate between contraindications and relative contraindications does not exist. Neither blindness nor previous amputation are regarded as contraindications. Hepatitis B, hepatitis C or human immunodefiency virus (HIV) infection in the potential recipient are not contraindications to pancreas transplantation either. Box 9.2 is intended as a guide only. No attempt has been made to separate absolute and relative contraindications. The use of imprecise definitions such as ‘significant’, ‘severe’ or ‘recent’ is also intentional. Appropriate patient selection requires a balanced assessment by experienced clinicians of the risk factors versus potential benefits.
Pancreas after kidney transplantation (PAK)
Historically the large majority of pancreas transplants performed have been SPKs. This was largely because of the relatively poor outcomes following solitary pancreas transplantation. Improved success of pancreas transplantation in the last 10 years has encouraged many transplant units to offer pancreas transplantation for diabetic patients who have previously undergone successful kidney transplantation. Until the end of 2000, PAK transplants constituted 11% of all pancreas transplants performed in the USA and 5% of pancreas transplants performed outside the USA.5 Around a quarter of US pancreas transplants between 2000 and 2005 have been solitary pancreas transplants.9 More detailed analysis of activity and outcome in different forms of pancreas transplantation is given in the next section.
Contraindications to PAK transplantation are the same as those for SPK (Box 9.2). Within the confines of these contraindications, all diabetics who have previously undergone successful kidney transplantation are potentially suitable candidates for PAK. In practice the procedure is most useful for those diabetics who have a potential living donor for kidney transplantation. With PAK outcomes now approaching those of SPK, an elective and early living-donor kidney transplantation has obvious benefits to the potential recipient and has additional benefits to the overall pool of patients awaiting transplantation by releasing another cadaveric kidney. Clearly some time should elapse after kidney transplantation to allow for recovery from surgery and stabilisation of allograft function and immunosuppression. The optimal timing has not been determined. Available data comparing early (within the first few months) with late (more than 4 months after kidney transplantation) PAK do not reveal any significant difference in the incidence of morbidity or outcome.10
Finally, an important consideration, in particular for patients who are being assessed some considerable time after kidney transplantation, is the adequacy of kidney function. Criteria based on strong evidence do not exist but a creatinine clearance of greater than 40 mL/min is commonly quoted as a minimum requirement.11 For recipients of kidney transplants who are not receiving calcineurin inhibitors, a higher creatinine clearance of not less than 55 mL/min is recommended. A renal allograft biopsy prior to PAK is useful for documentation of the baseline renal reserve and for the monitoring of the progression of allograft nephropathy (diabetic or otherwise).
Pancreas transplantation alone (PTA)
Universally agreed criteria that constitute indications for PTA are more difficult to find compared with those for SPK or PAK. Risks of transplantation for non-uraemic diabetics needs to take account of not only perioperative morbidity but also complications associated with immunosuppression. At present the majority of patients developing type I diabetes will be better served by insulin injections at the onset of disease. Clear indications for PTA are life-threatening complications of diabetes in patients managed with insulin, namely hypoglycaemic unawareness and cardiac autonomic neuropathy. In these two subpopulations of diabetic patients pancreas transplantation is truly life saving. Other indications for PTA are more controversial. The presence of two or more diabetic complications has been advocated as an indication.12 In the absence of conclusive data on some of the diabetic complications, as reviewed in the final section of this chapter, it is difficult to defend the logic behind the assertion that two or more complications constitute an indication for PTA. Disabling and intractable symptoms of diabetic neuropathy or early nephropathy with preserved renal function may be considered as indications. In diabetics with overt nephropathy and impaired renal function, the nephrotoxicity of the immunosuppressive drugs will need to be considered. Available evidence does not permit precise guidelines but patients with creatinine clearance less than 40 mL/min may be better served by SPK transplantation.
Pancreas transplantation activity worldwide
At the end of 2007 the total number of pancreas transplants performed worldwide exceeded 30 000. Nearly two-thirds of these have been performed in the USA. The International Pancreas Transplantation Registry (IPTR), based at the University of Minnesota, shares US transplant data with the United Network for Organ Sharing (UNOS). Reporting of data to the UNOS is compulsory, hence the IPTR records regarding US pancreas transplantation activity are accurate and complete. Non-US pancreas transplants are reported to the IPTR on a voluntary basis. Some national organisations, such as Eurotransplant, share data with the international registry. The IPTR estimates that >90% of non-US transplants are reported. Worldwide pancreas transplantation activity reported in a recent Council of Europe document suggests13 that a much greater proportion of non-US transplants are missing from the IPTR database (Fig. 9.1). Despite this probable under-representation of non-US transplants, there seems to be a genuine difference in the utilisation of pancreas transplantation between the USA and the remainder of the world. Figure 9.2 shows worldwide pancreas transplantation activity as recorded by the IPTR at the beginning of 2005.14
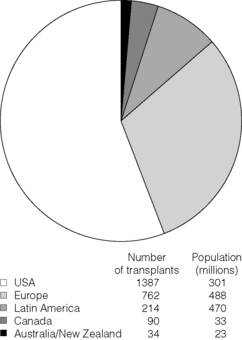
Figure 9.1 Pancreas transplants performed worldwide in 2006.
Data from International Figures on Organ Donation and Transplantation 2006. Transplant Newsletter 12(1), September 2007. Council of Europe.
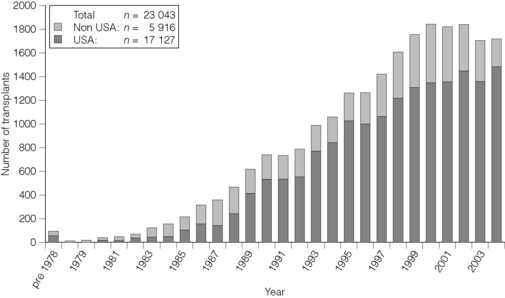
Figure 9.2 Pancreas transplants reported to the International Pancreas Transplant Registry (1 January 2005).
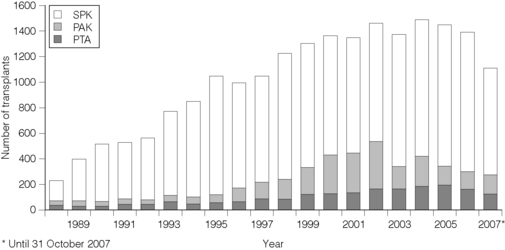
In the USA, SPK transplantation activity reached a peak of 972 transplants in 1998. Thereafter there has been a small decline and the activity has remained stable at a plateau of around 900 SPK transplants per annum. In contrast solitary pancreas transplantation activity (PAK + PTA) continued to increase from 64 in 1992 to 554 in 2002 (Fig. 9.3).
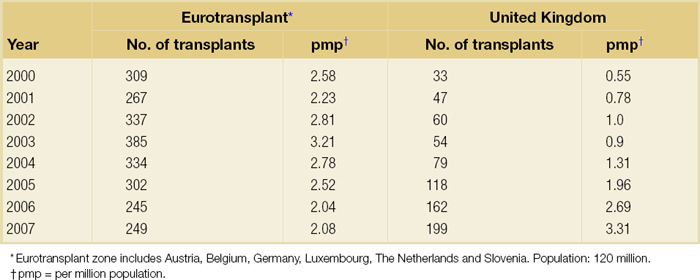
The total numbers of pancreas transplants performed in the UK and in the Eurotransplant zone are shown in Table 9.1 for comparison.15,16 In Europe, within the Eurotransplant zone pancreas transplantation activity has declined by about one-third since the peak of 2003. Conversely transplant activity has been steadily increasing in the UK. In 2006 and 2007 more pancreas transplants per million population were performed in the UK compared with the Eurotransplant zone.
The age profile of pancreas transplant recipients has also changed significantly over the last 15 years. In the USA between 1987 and 1992, 9% of pancreas transplant recipients were older than 45; in the period 2000–2004 this proportion had risen to 34%.9
Interestingly 5% of patients receiving pancreas transplants in the USA between 1994 and 2004 were classified as having type II diabetes at the time of transplant.9 There are no universally agreed criteria defining type I versus type II diabetes for the purposes of registration. Detectable or high C-peptide levels at the time of diagnosis of diabetes is often used to designate patients as type II diabetics. This may be misleading since the detection of C-peptide may simply reflect impaired elimination as a consequence of renal failure.3
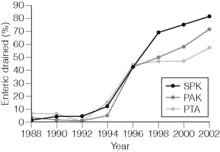
Management of exocrine secretions has also seen significant change (Fig. 9.4). Enteric drainage has been the predominant method in Europe but in the USA until the mid-1990s less than 10% of pancreas transplants were enterically drained. Enteric drainage has since surged in popularity in the USA also. Between 1996 and 2002 about half of US solitary pancreas transplants and two-thirds of US SPK transplants were enterically drained. In the most recent IPTR analysis,14 75% of all pancreas transplants (81% of SPK transplants) in the USA were enterically drained.
 Enteric drainage seems to have emerged as the preferred method of exocrine drainage worldwide in all but a small proportion of pancreas transplants.14
Enteric drainage seems to have emerged as the preferred method of exocrine drainage worldwide in all but a small proportion of pancreas transplants.14
Portal venous drainage gained popularity in the mid-1990s. Utilisation of portal venous drainage has remained relatively constant during the late 1990s and has increased slightly since 1999. In the USA between 1996 and 2002, 1091 of the 4394 (25%) enterically drained primary SPK cases have been performed with the portal venous drainage technique.17 Data from the IPTR 2000–2004 cohort reveal that this rate has since remained stable at around 25%.14
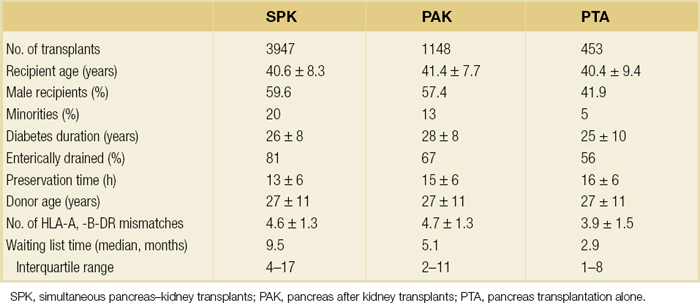
Other demographic data for patients transplanted in the USA between 1996 and 2002 are summarised in Table 9.2.
The pancreas donor and the organ retrieval procedure
Criteria for eligibility for pancreas donors
Absolute contraindications to organ donation are HIV infection, diagnosis of Creutzfeldt–Jakob disease (CJD), history of malignancy (except non-melanoma skin cancer and certain primary central nervous system tumours) and active systemic sepsis. Additional specific contraindications to pancreas donation are the presence of diabetes mellitus or gross pancreatic disease in the donor (including trauma, acute or chronic pancreatitis, excessive fatty infiltration). Neither hyperglycaemia nor hyperamylasaemia should preclude pancreas donation providing the pancreas appears normal on inspection. Increasing donor age, cerebrovascular/cardiovascular cause of death and donor obesity are associated with poorer pancreas transplant outcomes.18–20 A precise upper age limit for pancreas donors is difficult to define because of many confounding variables, the retrospective nature of the studies and small sample sizes of individual reports. IPTR analyses use 45 as the age cut-off distinguishing ‘young’ and ‘old’ donors. Historically no more than 3% of the US pancreas donors were older than 49.5 In the most recent cohort this has remained unchanged, donors older than 49 accounting for 3.4% of all deceased pancreas donors in the USA.9 In practice an upper age limit of around 55 is used by most transplant units and the general consensus is that the ideal pancreas donor will be younger than 45.
It is similarly difficult to quote an acceptable weight limit for donors. Body mass index (BMI) >30 should be regarded as a contraindication. Pancreas grafts from paediatric donors (age >4 years) and selected non-heart-beating donors can be used with excellent results.21,22 The influence of donor-related factors on pancreas transplant outcome is discussed on p. 189.
Pancreas retrieval operation
 University of Wisconsin (UW) solution was first developed as a pancreatic preservation solution23 and remains the benchmark for pancreas preservation. Other preservation solutions have been used but experience with these is limited.24
University of Wisconsin (UW) solution was first developed as a pancreatic preservation solution23 and remains the benchmark for pancreas preservation. Other preservation solutions have been used but experience with these is limited.24
The cold ischaemia tolerance of the pancreas is somewhere between that of the liver and the kidney. In pancreas allografts perfused with UW solution, 20–24 hours appears to be the limit for successful preservation, beyond which a time-dependent deterioration in outcome is demonstrable.25
Although there are no data that demonstrate a clear benefit from a preservation time cut-off below 20 hours, most surgeons intuitively aim for shorter preservation times. The mean (± SE) preservation time for the 2000–2004 cohort of pancreas transplants in the USA was 13.3 (± 5.9) hours for SPK, 15.3 (± 5.5) hours for PAK and 16.2 (± 5.8) hours for the PTA group.14
The pressure gradient between mean arterial pressure and portal venous pressure that maintains blood flow through the pancreas can be significantly diminished during the perfusion of the abdominal organs in retrieval operations. Particular attention is required to maintain an adequate gradient if a cannula for perfusion is placed in the portal venous system as well as the aorta. Many transplant units perfuse abdominal organs with an aortic cannula only. Some evidence supports the view that additional portal perfusion is unnecessary.26 For the interests of the pancreatic allograft, aortic perfusion alone is the most ‘physiological’ state that allows satisfactory perfusion and adequate drainage of the effluent.
Povidone–iodine during cold storage may be toxic to duodenal mucosa.27 If povidone–iodine is used for flushing the allograft duodenal segment during organ retrieval, further flushing of the duodenal segment with preservation solution on the back table should be considered.
Donor duodenal contents should be submitted for bacterial and fungal culture. The results may be important in guiding the management of infection in pancreas transplant recipients.28
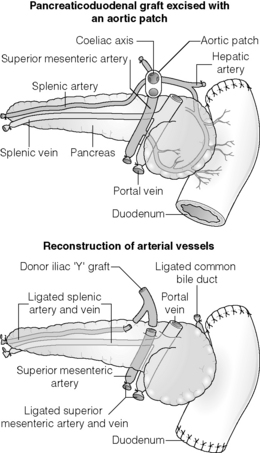
Further back-table preparation of the pancreas, which takes place in the recipient centre, is a crucial part of the procedure and takes a minimum of 2 hours. The short stumps of the proximal superior mesenteric artery (SMA) and splenic artery should be marked with fine polypropylene sutures at the time of retrieval. Demonstration of good collateral circulation between these two arteries by flushing them individually at the back table is reassuring. An iliac artery Y graft of donor origin anastomosed to the SMA and the splenic artery is the most common method of reconstruction for the graft arterial inflow (Fig. 9.5).
The pancreas transplant operation
General considerations
In the last 10 years the most common technique used for pancreas transplantation has been intra-abdominal implantation of the whole pancreas together with a donor duodenal segment. A list of previously employed techniques is given below. These are all associated with poorer outcomes and are rarely performed nowadays.
Management of exocrine secretions
Drainage of the exocrine secretions of pancreatic grafts into the recipient’s bladder was the most common technique, accounting for 90% of US pancreas transplants during the 1980s and early 1990s.29 The popularity of this technique was due to its perceived safety, primarily less serious consequences of anastomotic leaks (compared with enteric drainage) in the days of higher corticosteroids and unrefined immunosuppression. The ability to monitor amylase levels in the urine had been considered an additional advantage of bladder drainage. The latter point is contentious. The evidence with respect to the usefulness of urinary amylase monitoring is reviewed later in this chapter. The unphysiological diversion of pancreatic exocrine secretions into the urinary bladder causes frequent complications, often leading to chronic and disabling symptoms. As a consequence, conversion of the urinary diversion to enteric drainage is required in many patients. Complications of pancreatic transplantation, including specific problems associated with bladder drainage, are discussed in detail later in the chapter.
Any part of the recipient’s small bowel can be used for the anastomosis to the allograft duodenum. No data exist to demonstrate the superiority of one particular site over others. Roux-en-Y loops, which were commonly used, are becoming rare and a simple side-to-side entero-enterostomy is preferred.14 The correct alignment of the vascular anastomoses is also easier with enteric drainage.
Management of the venous drainage
Drainage of the venous outflow from pancreas grafts into the portal circulation was first described by Calne in 1984.30 This complex surgical technique using a segmental graft and gastric exocrine diversion in a paratopic position has never gained popularity. Drainage of the venous outflow into the systemic circulation at the level of the lower inferior vena cava (IVC) has been the norm in pancreatic transplantation. Since the mid-1990s there has been a resurgence of interest in portal venous (PV) drainage. The technique, described by Shokouh-Amiri et al.,31 involves placement of the graft slightly more cranially in the abdominal cavity with the utilisation of the superior mesenteric vein for the venous drainage. Several studies, including prospective randomised comparisons, have shown that this offers at least equivalent outcome to that of systemic venous (SV) drainage with no compromise in safety.32–34 The impetus for PV drainage was to achieve a more physiological insulin delivery. A theoretical benefit was considered to be avoidance of hyperinsulinaemia, which has been linked with atherogenesis.35 Systemic drainage does not always cause hyperinsulinaemia. Nor may it be the only factor, since hyperinsulinaemia occurs in non-diabetic recipients of kidney transplants receiving steroids.36,37 None of the studies of metabolic function after PV drainage have shown a clear benefit in terms of glucose metabolism, lipid profiles or atherogenesis. There is, however, evidence suggestive of an immunological advantage to PV drainage in the form of a reduction in the incidence of acute rejection. The mode of antigen delivery is known to modulate the immune response, which has been proposed as the mechanism responsible for the observed reduction in acute rejection rates in PV-drained grafts.12,32–34
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree