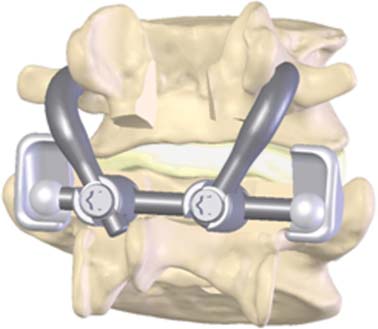
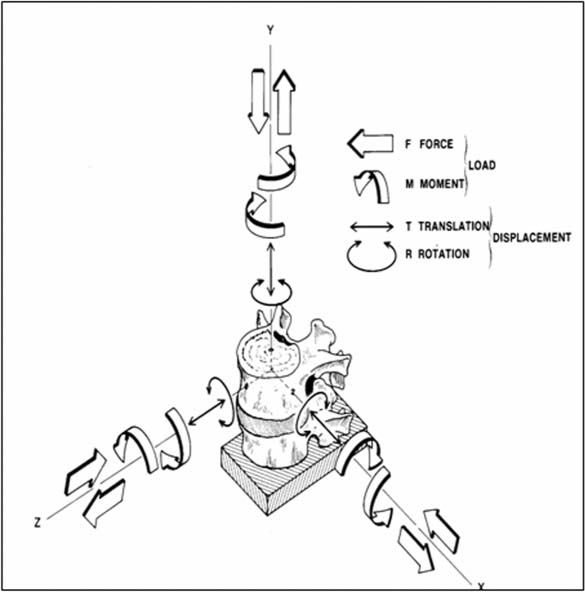
46 The Total Facet Arthroplasty System (TFAS) (Archus Orthopedics, Inc., Redmond, WA) is designed as a total joint replacement of the facets, employing proven technologies and approaches used successfully in total hip and total knee arthroplasty. It is a pedicle-based system that replaces the articulating zygapophyseal joint. The TFAS (Fig. 46–1) was invented by Mark Reiley, M.D., and designed in conjunction with Archus Orthopedics, Inc., as a patented, articulating joint prosthesis intended to provide stabilization of spinal segments in skeletally mature patients as an adjunct to laminectomy, laminotomy, neural decompression, and facetectomy in the treatment of several acute or chronic instabilities or deformities of the lumbar spine, including degenerative disease of the facets, degenerative disease of the facets with instability, grade I degenerative spondylolisthesis with objective evidence of neurological impairment, or central or lateral spinal stenosis. Although stability in all of these cases can be restored surgically with a properly designed implant, as in the case of pedicle rod fusion technologies, to provide a better outcome to the patient in terms of functionality and reduced incidence of complications, a “motion restoring” device that dynamically stabilizes and restores normal motions to the spine (TFAS) has been designed. With the advent of motion-preserving technology in the treatment of spinal disorders, many new products are positioning themselves as treatment alternatives to instrumented fusion. Many of these concepts are incremental line extensions of current fusion applications, as compared with TFAS, which represents a significant advancement in the treatment of posterior lumbar pathologies. Today, these pathologies are most frequently addressed via wide decompression procedures, which often lead to instability at the affected levels. Currently, instrumented fusion hardware is most commonly applied to address these iatrogenic instabilities. Adjacent level disease will be impacted at some level by motion-preserving technologies such as TFAS. The goal of these motion-preservation devices should be to re-create segmental function while attempting to restore stability and physiological motion to improve the biomechanics of the patient’s spine over the short and long term. With the advent of motion preservation devices for spine arthroplasty such as total disk and nucleus prosthetic replacements, the role of the facet joints in the etiology of spinal pathology, as well as the effect of surgical intervention on its temporal changes in physiology, contribution to biomechanics, and effect on the natural trajectory of spine disease, has been newly scrutinized.1–3 In the context of the functional spinal unit (FSU) segment biomechanics, the intervertebral disk, facets, and ligaments all play a key role. In general these structures have three main roles: to stabilize the vertebrae relative to each other and protect the nerves through a range of motion and loads; to provide proper motion for each FSU and the spine as a whole; and to transfer and share loads in the spinal column. Figure 46–1 Schematic of the Total Facet Arthroplasty System (TFAS). The FSU motion segment consists of two vertebral bodies and the intervening facet joints, intervertebral disk, posterior elements, and spinal ligaments. Each vertebral body interacts with its adjacent vertebrae by means of three articulating joints (Fig. 46–2). The major joint, in terms of load transmission and kinematic guidance, is the intervertebral disk joint. The disk and its components (annulus fibrosus, nucleus pulposus, and vertebral end plates) maintain the stiffness of the disk against compressive loading and allow for some degree of movement between vertebral bodies. Besides enabling bending movements between vertebral bodies, the intervertebral disk allows for twisting and small sliding movements. The posterior elements (pedicles, facets, transverse processes, superior articular processes, laminae, and spinous process) control the position of the vertebral bodies. These several processes serve as sites of attachment for muscles and ligaments that stabilize the lumbar vertebral column. The fine balance of all of these elements is usually disrupted by surgical procedures, such as decompression of stenosis in the lumbar spine, and is many times accompanied by adjuvant stabilization through rigid fixation with either or both metallic hardware and fusion. While stability is obtained, the additional elements: motion and load sharing, generally are not met. Lastly, damage to and pain from the diarthrodial facet joints and their corresponding capsular ligaments independent of surgical intervention for other causes can precede or coexist with spinal stenosis and deformities such as spondylolisthesis. The ability of spinal segments, from individual FSUs to multivertebral segments, to bear and transmit load while allowing for motion has been measured in the laboratory, characterized through mathematical modeling, and predicted through physiological loading regimes and ranges of motion. Unfortunately, up to this point, the study of the mechanics of the intervertebral joints has been reserved almost exclusively for the intervertebral disk joint, especially in the shadow of the design and development of artificial disk replacement hardware. Historically the facet joints have been attributed the role of motion limiters, which complement by their shape, size, location, and orientation the individual contributions of each anatomical spinal segment to the total role of the spine. The location of the facet joint along the spine determines its function (Fig. 46–3). In the cervical spine the loads transmitted across the facet joints are the lowest. However, the cervical spine exhibits the most freedom in lateral bending, extension, and axial torsion. The facet joints are located laterally almost in the coronal plane and are tilted in abduction to allow these motions. The cervical area is the region of lowest effective transmitted loads in the spine, but the region with most freedom in lateral bending, extension, and axial torsion, the facets, are located laterally, almost in the coronal plane, and are “tilted” in abduction to allow for these motions. In the lumbar spine, where axial rotation and lateral flexion are limited, the facets act like kinematic stops in these motions because most of the lumbar spine’s role is that of allowing flexion-extension in the sagittal plane, and the facets are subjected to the highest load magnitudes. As such, the facets are large, more centrally located, and oriented in a more sagittal (adducted) manner. In fact, they are almost parallel along that sagittal plane, allowing maximum flexion-extension while acting as “cam-like” stops for hyperextension and axial torsion. We know that the FSU has a documented “neutral zone” where the axial force transmitted by the spine is such that it is stiffer at the extreme ranges of motion and less so near the neutral position. A study of instrumented facet joints indicates that the facet joints have a similar dwell point or neutral zone (Fig. 46–4). Although its biomechanical activity and pathology can be as important and painful as those of the intervertebral disk, the zygapophyseal joint has been the subject of marginal attention. Figure 46–2 Degrees of freedom and motions of a functional spinal unit. (With permission from White and Panjabi, Clinical Biomechanics of the Spine, 2nd ed. Lippincott, Williams, and Wilkins, Philadelphia, PA).
Total Facet Arthroplasty System (TFAS)
 The Role of Total Facet Arthroplasty in Restoration of Spinal Biomechanics
The Role of Total Facet Arthroplasty in Restoration of Spinal Biomechanics
 Total Facet Arthroplasty System Investigational Device Exemption Clinical Study Inclusion Criteria
Total Facet Arthroplasty System Investigational Device Exemption Clinical Study Inclusion Criteria
 Facet Arthroplasty versus Dynamic Stabilization
Facet Arthroplasty versus Dynamic Stabilization
The Role of Total Facet Arthroplasty in Restoration of Spinal Biomechanics
Facet Biomechanics
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Facet Biomechanics
Facet Biomechanics Design Rationale
Design Rationale Product Performance
Product Performance Surgical Technique
Surgical Technique Conclusion
Conclusion